A Case of Takotsubo Cardiomyopathy in Sheehan’s Syndrome Secondary to Hydrocortisone and Levothyroxine Nonadherence
Author(s): Mohamed Ali Ahmed Mohamed (MRCP-UK)1*, Razan Abdulhaleem Mohamed Khalafallah (MRCP-UK)2
1Registrar of General Medicine and Cardiology - Western and Social Care Trust (NHS), The United Kingdom.
2Registrar of Cardiology - King Abdulaziz Cardiac Centre, Saudi Arabia.
*Correspondence:
Mohamed Ali Ahmed Mohamed, Registrar of General Medicine and Cardiology - Western and Social Care Trust (NHS), The United Kingdom.
Received: 20 February 2020; Accepted: 12 March 2020
Citation: Mohamed Ali Ahmed Mohamed, Razan Abdulhaleem Mohamed Khalafallah. A Case of Takotsubo Cardiomyopathy in Sheehan’s Syndrome Secondary to Hydrocortisone and Levothyroxine Nonadherence. Cardiol Vasc Res. 2020; 4(1); 1-4.
Abstract
Takotsubo Cardiomyopathy and Sheehan’s syndrome are quite rare conditions. Herein, we report a case of stress induced cardiomyopathy due to medications nonadherence in a known case of Sheehan’s syndrome. After glucocorticoid and levothyroxine replacement therapy, cardiac function recovered completely [1,2,3,9].
Keywords
Case History
A 59-year-old lady with a background medical history of type II diabetes mellitus, hypertension and panhypopituitarism secondary to significant post-partum haemorrhage 30 years ago; on replacement therapy with hydrocortisone (HC) and Levothyroxine (LT4). She stopped taking HC and LT4 as she ran out of medications for more than one week.
She had a recent presentation with recurrent vomiting, confusion, hypotension and severe hyponatraemia (107 mmol/L); this was treated as adrenal crises with IV fluids and hydrocortisone replacement and subsequently discharged home.
She presented to the Emergency Department a few hours following discharge with shortness of breath but had no chest pain, she was increasingly confused and agitated which required sedation.
On examination, she was confused and agitated, her vital observations were:
Blood pressure 106/55 mmHg – Pulse rate 67 beats per minute
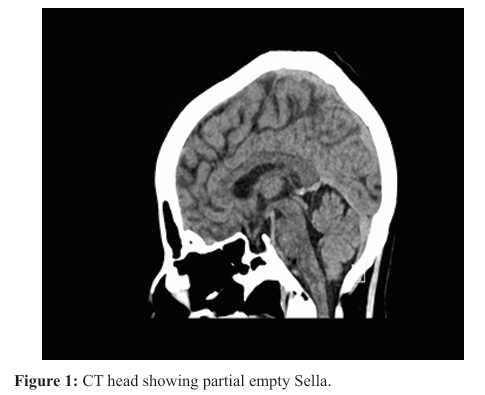
-SpO2 98% on room air – Temperature 36.7°C – Respiratory Rate of 19 breaths per minute. Cardiovascular and respiratory examination was unremarkable. An urgent CT brain showed empty Sella, otherwise no significant changes. (Figure 1). ECG showed significant dynamic ST and T wave changes in anterolateral leads (Figure 2 A and B).
Serum troponin was 7696 pg/ml (normal less than 50) with significant rise to 10100 pg/ml on serial check after 3 hours, serum Na 127 mmol/L and serum K 3.38 mmol/L. She was admitted as ACS-NSTEMI for further management
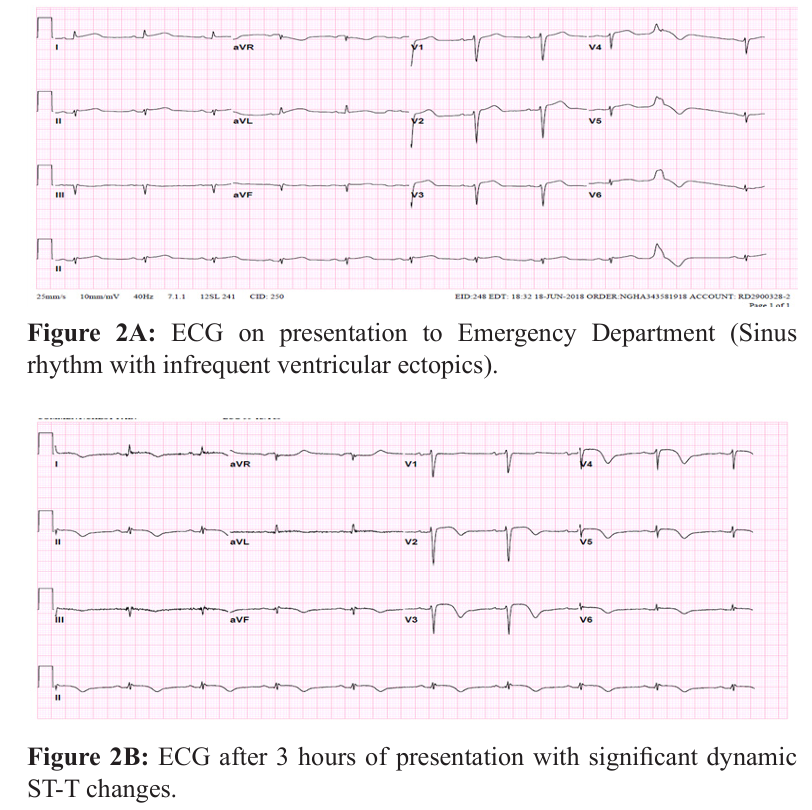
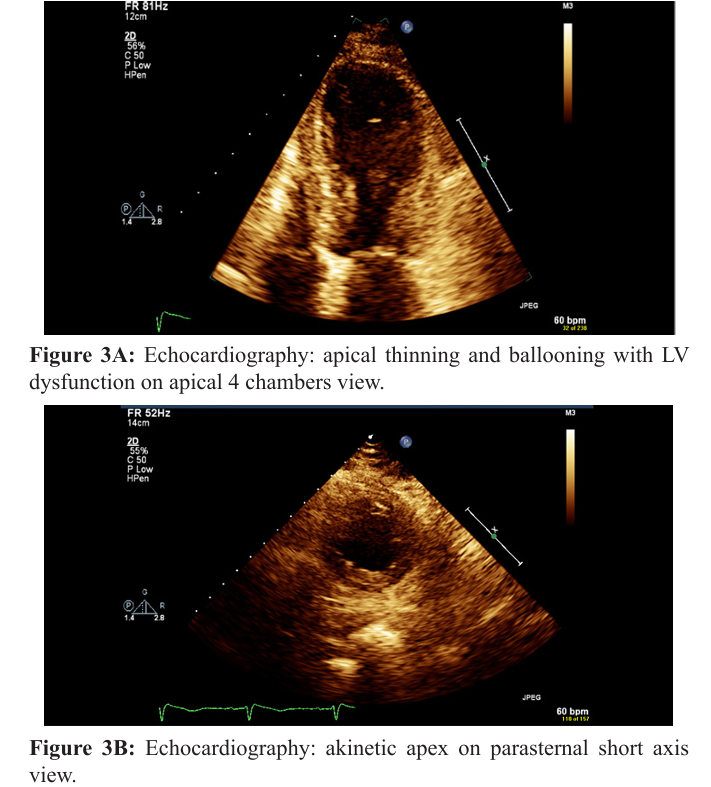
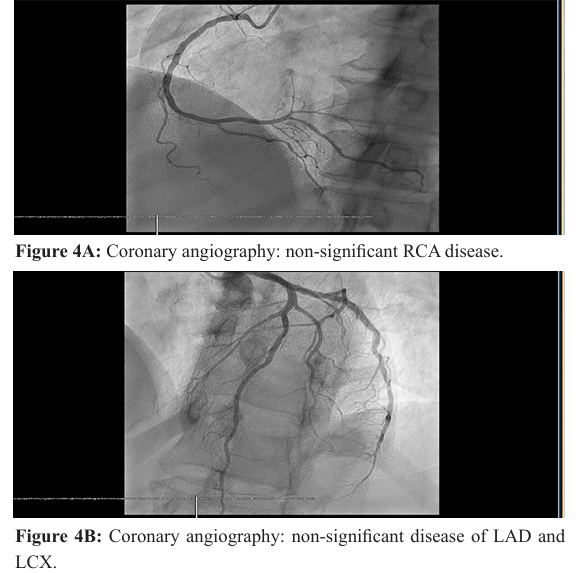
Echocardiography showed moderate to severe LV systolic dysfunction; EF 30-35% with apical akinesis. No significant valvular lesion (Figure 3 A and B) Coronary angiography was done as an emergency setting due to dynamic ECG changes and serial troponin rise which showed no significant coronary artery disease (Figure 4 A and B).
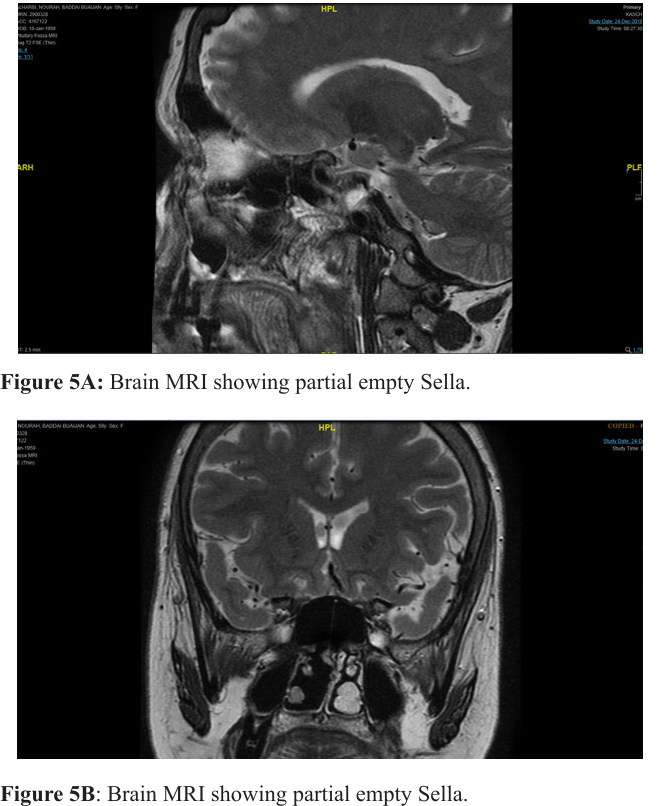
Hormonal assay confirmed panhypopiturism with adrenal insufficiency as Short Synacthen Test (SST) was positive, with Low FSH and LH and TSH. Brain MRI showed; Sella filled with CSF representing partial empty Sella turcica syndrome (Figure 5 A and B).
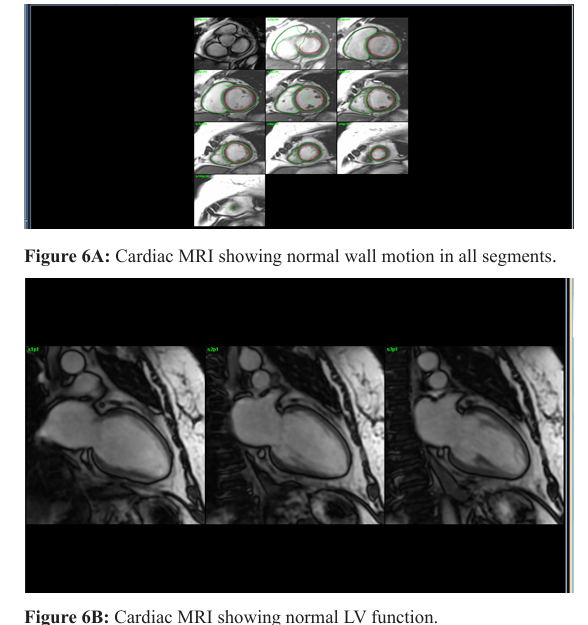
Levothyroxine and hydrocortisone doses were adjusted by consultant endocrinologist, and subsequently her condition improved and discharged home in a good condition. Cardiac MRI was done 3 months later as outpatient which showed normal size, wall motion and function of the left ventricle, LVEF = 55%. Normal size, wall motion and function of the right ventricle, RVEF = 64%. No myocardial scar or fibrosis noted (Figures 6A and B).
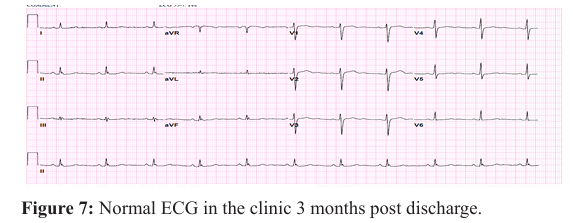
The ECG 3 months post discharge showed normal sinus rhythm with no ST-T changes (Figure 7).
Discussion
Sheehan’s syndrome was first described by Sheehan in 1937, it is a rare condition characterized by panhypopituitarism secondary to severe postpartum haemorrhage (PPH). It manifests with lethargy, lactation failure, amenorrhea, involution of breasts, loss of axillary and public hair and features of other pituitary hormone deficiencies. The cause of panhypopituitarism is thought to be ischemic necrosis of the anterior pituitary secondary to postpartum haemorrhage. Cardiac abnormalities have rarely been reported in patients with Sheehan’s syndrome [1,7,8].
There were few cases reported with cardiac abnormalities in Sheehan’s syndrome; two cases presented with symptoms of heart failure and subsequently diagnosed as dilated cardiomyopathy with complete recovery following hormonal replacement, one case presented with heart failure and cardiogenic shock with significant LV dysfunction and apical ballooning on LV angiogram and normal coronaries, diagnosed as Takotsubo cardiomyopathy, which recovered completely following hormonal replacement, and one patient presented with prolonged QT and ventricular tachycardia [1,2,3,9].
However, this case report is different as this lady is known to have Sheehan’s syndrome who stopped her medications as she ran out of them and therefore developed acute adrenal failure that manifests as confusion and cardiac involvement in form of acute coronary syndrome (ACS) as she reported shortness of breath with significant dynamic ECG changes and significant troponin rise on serial check, and what made it more challenging is that the patient has risk factors for CAD (Hypertension and Type II diabetes mellitus).
Although echocardiography was in keeping with Takotsubo cardiomyopathy, emergency coronary angiography was carried out to rule out coronary artery occlusion due to progressive troponin rise and dynamic ECG changes [6].
The complete normalization of left ventricular wall motion and function in the MRI study, when compared to the echocardiography 3 months prior to her acute presentation confirms that Takotsubo cardiomyopathy was the cause of LV dysfunction [4-6].
This makes it very essential to stress on the importance of taking medications regularly in patients with hypopituitarism as abrupt discontinuation of medications could have potential serious cardiac complications including stress induced cardiomyopathy, LV failure and arrhythmias which could be fatal.
References
- Zargar AH, Masoodi SR, Laway BA, et al. Clinical spectrum of Sheehan’s syndrome. Ann Saudi Med. 1996; 16: 338-341. Win CM, Pathak A, Guglin M. Not takotsubo: a different form of stress-induced cardiomyopathy—a case series. Congest Heart Fail. 2011; 17: 38-41.
- Researchgate.net/publication/272403452_A_Case_of_Stress-induced_Cardiomyopathy_in_Sheehan's_Syndrome
- Sunny D Shinde, Girish R Sabnis, Charan P Lanjewar, et al. A rare endocrine cause of electrical storm - a case report. European Heart Journal - Case Reports. 2017; 1: 1-5.
- Konstantinos Bratis. Cardiac Magnetic Resonance in Takotsubo Syndrome. Eur Cardiol. 2017; 12: 58-62.
- Eitel I, Behrendt F, Schindler K, et al. Differential diagnosis of suspected apical ballooning syndrome using contrast-enhanced magnetic resonance imaging. Eur Heart J. 2008; 29: 2651-2659.
- Dastidar AG, Frontera A, Palazzuoli A, et al. TakoTsubo cardiomyopathy: unravelling the malignant consequences of a benign disease with cardiac magnetic resonance. Heart Fail Rev. 2015; 20: 415-421.
- Fahrettin KeleÅ?timur. Sheehan's syndrome. Pituitary. 2003; 6: 181-188.
- Zargar AH, Singh B, Laway BA, et al. Epidemiologic aspects of postpartum pituitary hypofunction (Sheehan's syndrome). Fertil Steril. 2005; 84: 523-528.
- Wang SY, Hsu SR, Su SL, et al. Sheehan's syndrome presenting with early postpartum congestive heart failure. J Chin Med Assoc. 2005; 68: 386-391.