An Unusual Case of Acute Stent Thrombosis: A Review of a Rare Cause of Acute Stent Occlusion
Author'(s): Ben G.T. Coumbe1,2, Johan Aris Chandran1, Kien Hoe Ng1 and Joseph Tomson1*
1Royal Free Hospital, Pond Street, NW3 2QG, London.
2School of Clinical Medicine, University College London, Gower Street, WC1E 6BT, London.
*Correspondence:
Joseph Tomson, Royal Free Hospital, Pond Street, NW3 2QG, London, Tel: 07518 530406; E-mail: joseph.tomson@nhs.net.
Received: 16 October 2017; Accepted: 04 November 2017
Citation: Ben G.T. Coumbe, Johan Aris Chandran, Kien Hoe Ng, et al. An Unusual Case of Acute Stent Thrombosis: A Review of a Rare Cause of Acute Stent Occlusion. Cardiol Vasc Res. 2017; 1(1); 1-3.
Abstract
We present the case of a 55-year-old woman diagnosed with an ST-elevation myocardial infarction, on the background of receiving chemotherapy for metastatic ovarian cancer. She underwent primary angioplasty followed by a repeat angioplasty two hours later due to acute stent thrombosis. She was subsequently diagnosed to have acute severe thrombocytosis. This case highlights the role of exploring a broad differential diagnosis in cases of recurrent acute stent thrombosis and presents a very rare case of reactive thrombocytosis in a patient on systemic anti-cancer treatment presenting as a myocardial infarction. It highlights the benefits of inter-specialty liaison for delivering better patient care, especially in complicated treatment regimes for a number of disorders in various medical specialties.
Keywords
Case Presentation
A 55 year old woman was admitted to the emergency department with acute onset severe chest pain and shortness of breath. Her other relevant history was metastatic ovarian cancer for which she was being treated with gemcitabine/carboplatin chemotherapy, and hormone therapy (letrozole) for breast cancer. She had no identifiable cardiovascular risk factors.
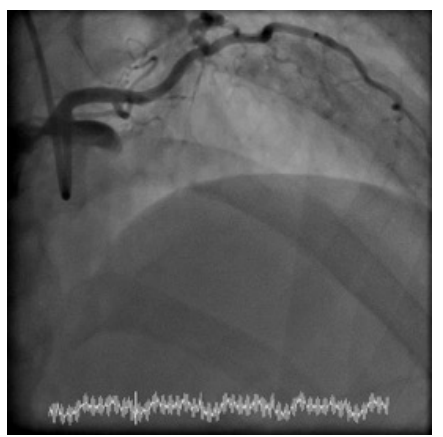
The patient was commenced on dual antiplatelet therapy with aspirin 300mg and ticagrelor 180mg, and after ECG confirmation of anterior ST elevation, underwent primary percutaneous coronary intervention to the left anterior descending artery (Figure 1), which was found to be completely occluded. Within 30 minutes of the procedure, she was noted to develop severe central chest pain with further ST segment elevation. A repeat angiogram showed acute intra stent thrombosis with complete occlusion. After restoration of blood flow with thrombus removal, she was started on IV tirofiban.
A few hours later the patient complained of a painful right finger. On examination, there were signs of an acute ischaemic right index finger consistent with a likely embolic event.
Investigations and Treatment
Routine blood tests demonstrate that she exhibited thrombocytosis on routine bloods four days prior to the cardiac event (platelet count of 731), which were a few weeks after she had commenced chemotherapy (Figure 2). Her baseline platelet count was within range (Normal range 150-400) up to the point of commencing chemotherapy.
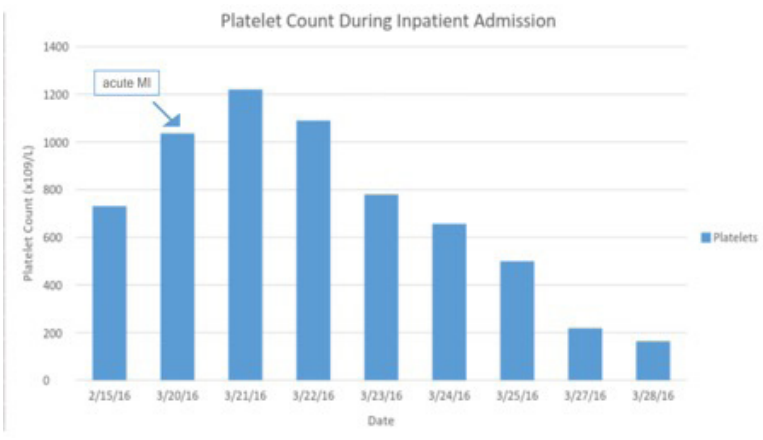
On admission, her blood test confirmed a platelet count of 1300, and the blood film showed marked thrombocytosis and toxic granulation of the neutrophils. A JAK2 mutation screen was negative. It was felt that the thrombocytosis was reactive; various options were considered including a different dual anti-platelet strategy with LMWH, continuation of Tirofiban, initiation of unfractionated heparin or consideration for additional NOAC treatment. After discussion with haematology, the tirofiban infusion was continued for a further 24 hours followed by treatment with low molecular heparin (clexane 1mg/kg/BD) for 6 weeks.
The platelet counts steadily declined over the next few days to a normal range of around 150-400 without any other specific intervention. The patient remained well at review 3 months after presenting with an infarct.
Discussion
Acute stent thrombosis is a rare complication and published literature shows an incidence of between 0.1-0.5% [1]. The common causes of acute stent thrombosis are suboptimal stent deployment, under-sizing of the stent or accidental discontinuation of anti-platelet treatment [2]. In this report, our patient had no identifiable cardiovascular risk factors, and there was no evidence of plaque rupture at the angioplasty. The systemic anti-cancer treatment she was receiving at the time were not known to be associated with increased cardiovascular risk. The recurrent stent thrombosis that occurred in this setting was however likely due to the significant thrombocytosis.
Thrombocytosis can be classified based on its aetiology into reactive and essential thrombocytosis. The underlying cause of the thrombocytosis is critical in determining the appropriate management of the condition. Essential thrombocytosis is a myeloproliferative disorder characterised by hyperplasia of megakaryocytes in the bone marrow. In contrast reactive thrombocytosis is caused secondary to an inflammatory response.
The result of an acute elevation in thrombopoeitin levels and cytokines such as IL-6; a situation commonly found secondary to infection, inflammatory disorders or iron deficiency anaemia. Such thrombocytosis predisposes patients to vascular complications, such as bleeding and thrombosis.
In this case, the aetiology of reactive thrombocytosis is a subject for debate, and may not be solely attributable to being secondary to the cardiac event. The observed thrombocytosis could potentially be explained by the side effect of gemcitabineinduced thrombocytosis. In a Canadian study of 220 patients who received gemcitabine chemotherapy with or without platinum based chemotherapy, a total of 46% of patients developed transient thrombocytosis lasting a median duration of 2 weeks [3]. However, the study concluded that thrombocytosis in these cases were usually benign and did not contribute to pathological vascular and/ or thromboembolic events.
Patients with reactive thrombocytosis do not usually require cytoreductive medication or antiplatelet treatment. However, the present report highlights the risks of thrombosis and thromboembolic events necessitating management with additional antithrombotic therapy in addition to routine dual antiplatelet therapy post MI. The platelet counts normalised to baseline levels, below 400, within two weeks of the event.
Thrombocytosis is a rare cause of myocardial infarction in patients, especially in this case with normal coronaries and no risk factors. However, in patients with myeloproliferative disorders such as essential thrombocytosis, there is a high predisposition to thrombotic and haemorrhagic events associated with significant morbidity and mortality [4]. This is well documented within case reports within the current literature [5-7]. However we are aware that reactive thrombocytosis following myocardial infarction is rare [5,8-10]. Thus, we do not know if the thrombocytosis led to the initial presentation or it was a reactive rise in platelet count secondary to the STEMI.
Learning points
- This case demonstrates the importance of exploring a range of differential diagnoses when investigating the cause of acute coronary syndromes with no significant background CVD risk factors and in cases with acute stent thrombosis with high thrombus burden, above and beyond excluding mechanical or procedural causes for thrombosis such as suboptimal stent deployment. The recognition and appropriate management of other causes, such as underlying the co-existing haematological disorder in our case, will have implications in the antithrombotic management in the peri-infarct setting, where treatment other than standard dual antiplatelet agents may become necessary.
- To our knowledge, this is the first case of reactive thrombocytosis in a patient on systemic anti-cancer treatment presenting as a myocardial infarction. As this case highlights, reactive thrombocytosis secondary to chemotherapy could have potentially harmful consequences, and patients should be consented for this before commencing cancer treatment.
- This case exhibits an example of how multidisciplinary team working could better patient care with safer outcomes. With increasingly complicated treatment regimens for a number of disorders in various medical specialities including Oncology, it is essential for clinicians across specialties participate in regular discussions to formulate the optimal management plans for patients.
Acknowledgments
Written informed consent was obtained from the patient to publish the clinical details and images in this article.
References
- Patel VG, Brayton KM, Tamayo A, et al. Angiographic success and procedural complications in patients undergoing percutaneous coronary chronic total occlusion interventions: a weighted meta-analysis of 18,061 patients from 65 studies. JACC Cardiovascular interventions. 2013; 6: 128-136.
- Nakano M, Yahagi K, Otsuka F, et al. Causes of Early Stent Thrombosis in Patients Presenting With Acute Coronary Syndrome. An Ex Vivo Human Autopsy Study. 2014; 63: 2510-2520.
- Ahmed S, Shahid RK, Bhatt H, et al. Chemotherapy-related thrombocytosis: does it increase the risk of thromboembolism? Oncology. 2012; 82: 327-332.
- Casini A, Fontana P, Lecompte TP. Thrombotic complications of myeloproliferative neoplasms: risk assessment and riskguided management. Journal of thrombosis and haemostasis: JTH. 2013; 11: 1215-1227.
- Ghaffari S, Pourafkari L. Acute myocardial infarction in a patient with post-splenectomy thrombocytosis: a case report and review of literature. Cardiology Journal. 2010; 17: 79-82.
- Nanavati A, Patel N, Burke J. Thrombocytosis and Coronary Occlusion. JACC: Cardiovascular Interventions. 2012; 5: e18-e19.
- Posfai E, Marton I, Borbenyi Z et al. Myocardial infarction as a thrombotic complication of essential thrombocythemia and polycythemia vera. Anatolian Journal of Cardiology. 2016; 16: 397-402.
- Dumrongmongcolgul N, Mankongpaisarnrung Sutamtewagul G, et al. Reactive Thrombocytosis Associated with Acute Myocardial Infarction following STEMI with Percutaneous Coronary Intervention. Case reports in cardiology. 2013; 2013: 707438.
- Wilkerson B and Elkins S. 102 Clinical Significance of Reactive Thrombocytosis after Acute Myocardial Infarction and Subsequent Stent Placement: A Retrospective Chart Review. Journal of Investigative Medicine. 2006; 54: S274-S274.
- Tai YT, Yu YL, Lau CP, et al. Myocardial infarction complicating postsplenectomy thrombocytosis, with early left ventricular mural thrombus formation and cerebral embolism-a case report. Angiology. 1993; 44: 73-77.