Anesthetic Management of a Patient with Kleine-Levin Syndrome: Case Report
Author'(s): Azhar Rehman1*, Asma Abdus Salam2 and Fareena Khan3
1Assistant Professor, Aga Khan University, Karachi, Pakistan.
2Senior Instructor, Aga Khan University, Karachi, Department of Anesthesiology, PW II, Aga Khan University, Karachi, Pakistan.
3Resident, Year-III, Aga Khan University, Karachi, Department of Anesthesiology, PW II, Aga Khan University, Karachi, Pakistan.
*Correspondence:
Dr. Azhar Rehman, Assistant Professor, Aga Khan University,Stadium Road, Karachi, Pakistan, Tel: 03002260187; E-mail: azhar.rehman@aku.edu.
Received: 14 January 2018; Accepted: 16 February 2018
Citation: Azhar Rehman, Asma Abdus Salam, Fareena Khan. Anesthetic Management of a Patient with Kleine-Levin Syndrome: Case Report. Anesth Pain Res. 2018; 2(1): 1-2.
Abstract
Forty one year old female known case of Kleine –Levin Syndrome, admitted for elective total abdominal hysterectomy. There is no literature describing the anaesthesia technique in these patients, we tried to avoid all known factors which could trigger the disease so we used central neuraxial anesthesia in the form of combined spinal-epidural block. Procedure was done successfully without any complication and patient remained pain free postoperatively.
Keywords
Introduction
Kleine- Levin Syndrome (KLS) is a very rare Syndrome and is 80- 90% times more common in males. It was first described in 1925 by Willi Kleine. In 1942 Critchky and Hoffman further explained the symptoms of disease on the basis of cases which they had reported. KLS was first classified in 1990 by the International Classification of sleep disorder (ICSD) [1-4].
The symptoms of KLS are intermittent in nature and are periodic including excessive daytime sleep. When awaken they are apathetic despite a sleep of more than 20 hours and have difficulty in communication and concentration deficit. Other classical symptoms include compulsive hyperphagia and hypersexuality which is seen more in males; all three symptoms are present only in 45% of patients [5].
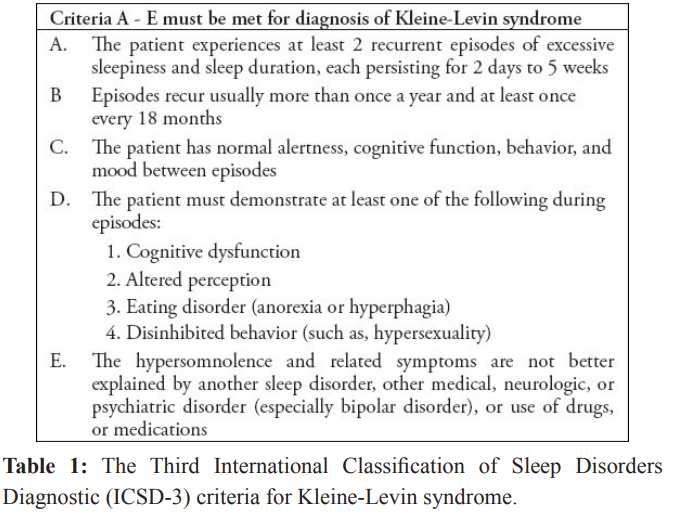
In the initial period of cycle when the symptoms starts, it is difficult to wake up the patient. However at the end of episode patient may appear to be simply resting with eyes closed [6,7]. Symptoms may persist for 1-3 weeks and the cycle usually ends in 60-100 days. The length of the cycle increases with the progress of disease and increasing age. Usually the symptoms trigger after fever, infections, head trauma, dental anesthesia, vaccination, sleep deprivation and alcohol intake [8]. KLS is a diagnosis of exclusion therefore other neurological, medical, metabolic or psychiatric disorders should be ruled out [9] [Table 1].
Investigations in patients with KLS shows normal polysomnography. Electroencephalogram (EEG) findings are positive in 70% of patients during the episode. Serum and cerebrospinal fluid biochemistry is normal. Brain imaging shows normal Magnetic resonance imaging (MRI) and computed tomography (CT) scan. The only investigation that shows positive findings is Fludeoxyglucose- positron emission tomography, scanning shows asymmetric hypometabolism in thalamus and hypothalamus [10].
There is no definitive treatment for KLS but drugs like modafinil, antipsychotics, amantadine and lithium have some role in reducing the duration of symptoms.
Case Report
Forty one year old female known case of Kleine -Levin Syndrome, was diagnosed in 2003 by the neurologist (on the basis of her clinical signs, symptoms and investigations) came to preoperative assessment clinic for her planned elective procedure total abdominal hysterectomy (TAH). Patient was functional class I, the last episode of KLS occurred three months back and lasted for three months. She had three episodes of remission; the longest one was of eight months duration. She does not have any other comorbidity. As we know that all anesthetic agents and narcotics may trigger the disease therefore patient was counseled in detail for combined spinal epidural (CSE) anesthesia.
On the day of procedure anxiolytic was avoided, which is usually given to every patient in our hospital where indicated. In operating room standard monitoring including electrocardiography (ECG), pulse oximetry and non invasive blood pressure were applied and intravenous cannulation was done. After all aseptic measures, central neuraxial anesthesia was achieved by using 18G CSE needle and bupivacaine 0.5% hyperbaric 10 mg was given in spinal space. Epidural catheter was inserted subsequently and secured. After achieving the desired level of sensory block, surgery was started. Epidural infusion was started after one hour at the rate of 10ml/hr 0.1% Bupivacaine. Patient remained comfortable throughout the surgery. Surgery lasted for two hours and it went un eventful. Patient was shifted to post anesthesia care unit where her vitals remained stable. She was assessed for post-operative pain and motor block. Her motor block regressed gradually after 3hrs and she was shifted to the ward. Post-operative pain was managed with epidural infusion of 0.1% Bupivacaine for 48 hrs. After the discontinuation of epidural oral meloxicam was started. She was discharged home on post-operative day 4. On day 7and 14 she visited the clinic her recovery was good with no exacerbation of disease.
Discussion
he anesthetic management of patients with KLS is a real challenge. There is not even a single case report describing the anesthetic management of these patients; although it is a well-known fact that general anesthesia is contra indicated in this disease. Ferguson has mentioned in a case report in which KLS was triggered after dental local anesthesia (Xylocaine) [11]. In our case, as we had no other option, we used local anesthestic agent bupivicaine in CSE. But we otherwise tried to avoid all the triggering factors. To allay anxiety a sound counseling was done preoperatively and she was reassured about her postoperative pain management.
It has also been known that for post-operative pain management, pure or synthetic narcotics should not be used. The perioperative management of KLS is more cumbersome because of a number of aggravating factors which may relapse the disease so we as anesthesiologists have very limited options for the perioperative management of these patients.
In hospitals with limited resources where normally cases are done only under general anesthesia, due to unavailability of the equipment and lack of training in regional anesthesia, the management of KLS and similar syndromes become more difficult and cases may end up in morbidity. With the changing trends in the field of anesthesia we should get expertise in regional anesthesia for better outcome of the patients and should practice safe.
In this case we used Bupivacaine but there are some other medications that have better safety profile in epidural anesthesia such as Ropivacaine but has not yet been used in these patients. We therefore recommend that the use of central neuraxial anesthesia technique with Bupivacaine is safe to provide surgical anesthesia and postoperative analgesia in patients with KLS.
References
1.Critchley M, Hoffman H. The syndrome of periodic somnolence and morbid hunger (Kleine-Levin syndrome) Br Med J. 1942; 1: 137-139.
2.American Academy of Sleep Medicine. International Classification of Sleep Disorders: Diagnostic and Coding Manual. 2nd ed. Westchester, IL: American Academy of Sleep Medicine. 2005.
3.Aurelie K, Sophie L, Marie OH, et al. Feeling unreal: a functional imaging study in patients with Kleine-Levin syndrome. Brain. 2014: 137; 2077-2087.
4.Afolabi-Brown O, Mason II TB. Kleine-Levin Syndrome. Paediatr Respir Rev. 2016.
5.Frenette E, Kushida CA. Primary hypersomnias of central origin. Semin Neurol. 2009; 29: 354-367.
6.Ugoljew A, Kurella B, Nickel B. Sleep polygraphic studies as an objective method for assessing the therapeutic result in a case of periodic hypersomnia (Kleine-Levin syndrome) Nervenarzt. 1991; 62: 292-297.
7.Billiard M, Podesta C. Recurrent hypersomnia following traumatic brain injury. Sleep Med. 2013; 14: 462-465.
8.American Academy of Sleep Medicine. International Classification of Sleep Disorders - Third Edition (ICSD-3) Darien (IL): American Academy of Sleep Medicine. 2014.
9.Shi YT, Tang BS, Jiang H. Kleine-Levin syndrome with brain atrophy. J Clin Neurosci. 2013; 20: 1027-1028.
10.Mignot EJ. A Practical Guide to the Therapy of Narcolepsy and Hyper-somnia Syndromes. Neurotherapeutics. 2012; 9: 739-752.
11.Ferguson BG. Kleine- Levin Syndrome: a case report. J Child Psychol Psychiatry. 1986; 27: 275-278.