Angiographic Pattern of Coronary Artery Disease in Pre-Menopausal Indian Women: A Single Centre Study
Author'(s): Soman Biji1, Rahaman Muneer A2, Rajan Rajesh3 and Vijayaraghavan Govindan2
1Department of Cardiology, Sree Uthram Thirunal Royal Hospital,Trivandrum, Kerala, India.
2Department of Cardiology, Kerala Institute of Medical Sciences,Trivandrum, Kerala, India.
3Department of Cardiology, Amiri Hospital, Kuwait City, Kuwait.
*Correspondence:
Biji Soman, Consultant Cardiologist, Sree Gokulam Medical College & Research Foundation, Trivandrum, India, Tel: +919895873043; E-mail: bijisoman@hotmail.com.
Received: 20 October 2017; Accepted: 11 November 2017
Citation: Soman Biji, Rahaman Muneer A, Rajan Rajesh, et al. Angiographic Pattern of Coronary Artery Disease in Pre-Menopausal Indian Women: A Single Centre Study. Cardiol Vasc Res. 2017; 1(1); 1-5.
Abstract
Background: Coronary Artery Disease (CAD) is increasingly becoming the disease of the young. Not much is known regarding the incidence, degree and pattern of CAD in pre-menopausal Indian women. Our aim was to study the prevalence and pattern of CAD among pre-menopausal women undergoing CAG.
Methods: Data of 100 women who underwent CAG for suspected CAD over 2 years were retrospectively analyzed. They were classified into pre-menopausal group (age ≤ 50 years) and post-menopausal group (age ≥ 60 years). Risk factor profile and coronary angiographic profile of these patients were studied and compared.
Results: The mean age of pre-menopausal women was 45.8 ± 4.2 years and 67.4 ± 6.4 years was the mean age of the post-menopausal women. Hypertension was the commonest risk factor in both the groups, with significantly higher incidence of hypertension in the post-menopausal group (24 vs. 41, p = 0.0029). Greater number of premenopausal women CAD with none of the risk factors, (15 vs. 04, p = 0.0004). There was a greater prevalence of obstructive CAD (31 vs. 15, p<0.0013) among post-menopausal women, especially triple vessel disease (TVD) (3 vs. 15, p = 0.0018). Left anterior descending (LAD) artery is the most commonly affected vessel. Proximal segment was the most frequently affected segment of the coronary artery.
Conclusion: Pre-menopausal women had a higher percentage of angiographically normal epicardial coronaries and non obstructive CAD, and even those who had obstructive CAD; the prevalence of multi vessel disease was much less when compared with the post-menopausal women.
The risk factor profile and pattern of coronary disease in pre-menopausal women is different from the conventional picture.
Keywords
Introduction
More than 33% of adult females have some form of cardiovascular disease [1]. CVD deaths are almost the same as that of cancer, chronic lower respiratory disease, and diabetes mellitus put together [1]. More alarming is the fact that coronary artery disease (CAD) among pre-menopausal women is increasing. Much is not known about the disease pattern and the angiographic profile in this subset of the population. Hence, there is lots of uncertainty and speculation regarding the pattern of the disease in general and the angiographic prevalence and pattern of CAD in pre-menopausal women. Our aim was to compare the angiographic pattern of CAD in pre-menopausal and post-menopausal women undergoing coronary angiography (CAG).
Materials & Methods
The data of 100 women admitted with acute coronary syndrome (ACS) and underwent CAG over a period of 2 years were retrospectively analyzed. The risk factor profile was obtained after reviewing the case records of these patients. Coronary angiograms and angiogram reports were studied to get information about angiographic profiles of these women. They were classified into “pre-menopausal group” (age ≤ 50 years) and “post-menopausal group” (age ≥ 60 years). In this study, obstructive CAD was defined as at least 50% stenosis of luminal diameter of the left main coronary artery (LMCA) or at least 70% stenosis of luminal diameter of at least one of the major epicardial coronary arteries. Non-significant lesion was defined as less than 50% stenosis of luminal diameter of any epicardial artery. Intermediate lesion was defined as 50 – 70 % stenosis of luminal diameter of one of the major epicardial arteries. Depending on the number of major epicardial arteries involved, they are classified as single vessel disease (SVD), double vessel disease (DVD) and triple vessel disease (TVD). Left main disease (LMD) was defined as at least 50% stenosis of luminal diameter of LMCA. The prevalence and pattern of CAD in these women were analyzed. All statistical analyses were performed using Statistica version 8 software. A p-value <0.05 was considered statistically significant.
Results
Of the 100 women who underwent CAG during the study period. There were 50 women in the pre-menopausal group and 50 women in the post-menopausal group. The mean age was 45.8 ± 4.2 years and 67.4 ± 6.4 years for pre-menopausal women and post- menopausal women respectively.
Profiling of the risk factors among the women of both the groups (Table 1) revealed that Hypertension was the commonest risk factor in both the groups, with statistically significant higher incidence of hypertension in the post-menopausal group (24 vs. 41, p=0.0029). While there was no significant difference in the incidence of diabetes mellitus and dyslipidemia in the two groups, there were greater number of pre-menopausal women with none of the above three risk factors, (15 vs. 04, p=0.0004). This signifies that diabetes mellitus affects the Indian women at an younger age than does hypertension or dyslipidemia, and also, that, conventional risk factors do not play as significant a role in the pre-menopausal women, as evidenced by a statistically significant number of women with none of the three conventional risk factors but still having CAD in the pre-menopausal group.
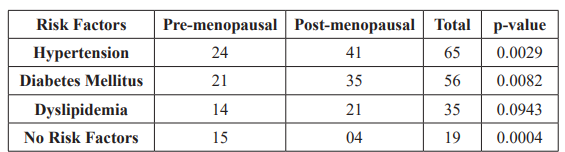
Table1: Risk Factor profile of women undergoing Coronary Angiogram.
The overall angiographic profile of the study population (Table 2) showed normal epicardial coronaries in 31 (31%) women, , non atherosclerotic lesion in 7 (7 %) women, non-significant lesion in 9 (9 %) women, intermediate lesion 7 (7%) and obstructive CAD in 46 (46 %) women. There were 4 (4%) women with LMD, 15 (15 %) women with SVD, 9 (9 %) women with DVD, 18 (18 %) women with TVD.
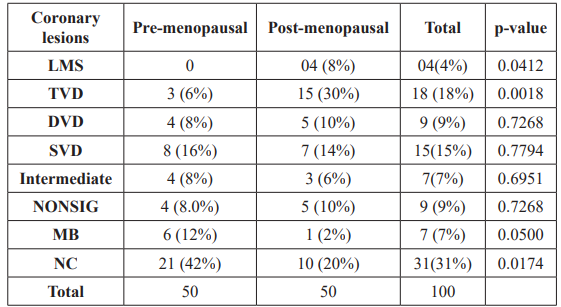
Table2: Angiographic profile of women undergoing coronary angiogram. LMS: Left Mainstem disease, TVD: Triple Vessel Disease, DVD: Double Vessel Disease, SVD: Single Vessel Disease, NONSIG: Nonsignificant disease, MB: Muscle Bridge, NC: Normal Coronaries.
Subgroup analysis revealed that normal epicardial coronaries were significantly common in pre-menopausal women than post-menopausal (21 vs. 10, p=0.0174). There was no statistical difference in the prevalence of non-significant lesion (4 vs. 5, p=0.7268), non atherosclerotic lesion (6 vs. 1 p=0.05) and intermediate lesion (4 vs. 3, p =0.6951) between pre-menopausal women and post-menopausal women. Obstructive CAD was significantly higher among the post-menopausal women than pre-menopausal women (31 vs. 15, p<0.0013). The proportion of women with SVD (8 vs. 7, p=0.78) and DVD (4 vs. 5, p=0.72) was not statistically significant between the two groups. On the other hand, TVD (3 vs. 15, p=0.0018) were more prevalent in post- menopausal group.
The angiographic distribution of CAD in women (Table 3) showed involvement of left anterior descending coronary artery (LAD) in 38 (38%) women, left circumflex coronary artery (LCX) in 34 (34%) women, right coronary artery (RCA) in 28 (28%) women and LMCA in 4 (4%) women. LAD was the most common vessel involved in both pre-menopausal and post-menopausal group. LMCA was the least affected vessel. This same pattern of involvement of the coronary arteries was seen in pre-menopausal women as well as in post-menopausal women, but pre-menopausal women had fewer vessel involved per patient when compared with post-menopausal women (0.64 vs. 1.36, p<0.0001).
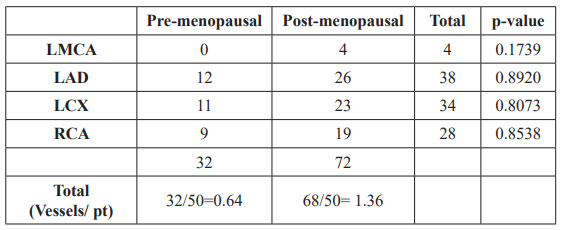
Table 3: Distribution of coronary artery disease in women undergoing coronary angiogram.
LMCA: Left main coronary artery, LAD: Left anterior descending artery,
LCx: Left circumflex artery, RCA: Right coronary artery.
The lesion distribution in the coronary arteries was nearly identical (Table 4). Even though the LAD had the maximum lesions when both the groups were analysed together, sub group analysis revealed that pre-menopausal women had more lesions in the LCx 26 (40%), while the post-menopausal women had a greater number of lesions in LAD 50 (40.3%). There was statistically significant difference in the involvement of the Ramus intermedius (RI) between the two groups, with pre-menopausal women having more frequent involvement (6 vs. 1, p=0.0036).
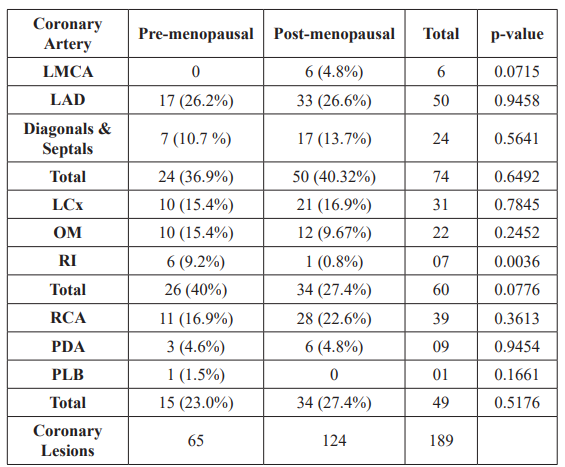
Table 4: Lesion distribution in Coronary arteries among women undergoing coronary angiogram.
LMCA: Left main coronary artery, LAD: Left anterior descending artery, LCx: Left circumflex artery, OM: Obtuse marginal, RI: Ramus intermedius, RCA: Right coronary artery, PDA: Posterior descending artery, PLB: posterolateral branches.
There was no significant difference in the severity of the coronary lesions between the two groups (Table 5). The total numbers of lesions were nearly double in the post-menopausal women, (65 vs. 124, p < 0.0001). 22 (11.6%) of the lesions were insignificant and, 48 (25%) of the lesions were intermediate lesions with a major 119 (63%) of lesions being obstructive lesions. Post-menopausal women had more severe CAD as evidenced by a greater number of total lesions and also more lesions per patient, (1.3 vs. 2.48, p<0.0001).
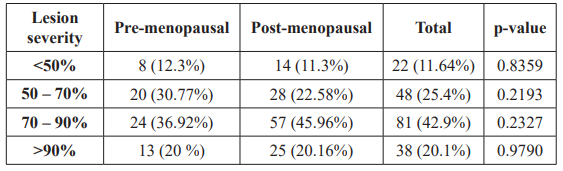
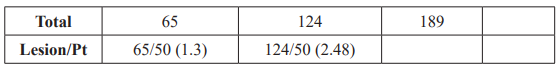
Table 5: Severity of Coronary Artery Lesions among women undergoing coronary angiogram.
There was no statistically significant difference in the segmental involvement pattern in both the groups (Table 6). Proximal segment lesions were the commonest in both the groups and ostioproximal lesion was the least common.
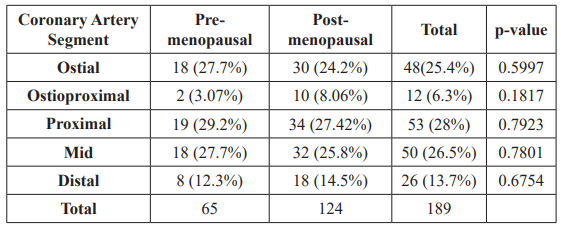
Table 6: Pattern of segment distribution of coronary artery disease among women undergoing coronary angiogram.
Discussion
CAD is no more a disease of the old. CAD is nearing epidemic proportion in India. Even though the incidence has come down to nearly half in the western world, in the last three decades, alarmingly, the rates have doubled in India over the same period of time. In India, the average age of first myocardial infarction (MI) has come down by 20 years. More women than men died because of CAD among Asian Indians [2]. The incidence of CAD among women is on the rise, more young women are undergoing CAG because of the early onset of risk factors [3].
HT and DM along with dyslipidemia are considered the traditional risk factors for CAD. Our study showed that the incidence of HT was higher among post-menopausal women, whereas DM and dyslipidemia were common in both groups, and also the proportion of patients with none of the conventional risk factors and still having CAD was significantly higher in the pre menopausal group signifying that there are factors other than the conventional risk factors contributing to the CAD of the young women.
Multiple studies have revealed that obstructive lesions are more likely among men when compared with women undergoing coronary angiography [4,5]. Greater than 50% of women with absence of obstructive CAD continue to have symptoms and end up having repeat CAG later [6,7].
In our study, 46% of the women had significant CAD. Post menopausal women had a higher incidence of obstructive CAD, especially multi vessel disease [8], while premenopausal women had greater prevalence of angiographically normal epicardial coronaries. Contrary to Dave et al. [9], observation, the prevalence of SVD (15%), DVD (9%) and TVD (18%) were nearly similar in our study group. In our study, 27% of the women had multivessel disease (DVD and TVD). 28% of the premenopausal women had non obstructive CAD and 42% had angiographically normal epicardial coronaries.
It is not rare to find normal or non obstructive CAD during CAG, its more commonly seen in younger, premenopausal women, who may not have the conventional cardiac risk factors [10]. About 10% - 25% of women presenting with acute coronary syndrome have non obstructive CAD [11-14]. Combination of myocardial ischemia and non obstructive coronary arteries are more common among women [15]. Women with symptoms of myocardial ischemia and non obstructive CAD on angiography, were thought to have a low risk of CAD or benign illness [16,17].
In spite of, The National Heart, Lung, and Blood Institute-sponsored Women’s Ischemia Syndrome Evaluation (WISE) study showing relatively poor prognosis among women with non obstructive coronary disease and evidence of myocardial ischemia when compared with those with similar lesion morphology and no myocardial ischemia [18], majority of the patients are offered only reassurance [19].
Stress echocardiograhy is popular investigation for the assessment of myocardial ischemia particularly among younger women because of lack of radiation and it has high levels of sensitivity and specificity [20,21]. Cardiac magnetic resonance (CMR) imaging has shown that women with ischemic symptoms and non obstructive CAD had greater incidence of subendocardial ischemia [22]. Late gadolinium enhancement was also more common in this subset of the population [23]. Abnormalities in flow reserve can be ascertained by gated single-photon emission computed tomography [24], and positron emission tomography [25].
Coronary flow assessment [26], single-photon emission computed tomography (SPECT) [24], or positron emission tomography [25], have shown evidence of vascular dysfunction in more than 50% of women with ischemic symptoms and non obstructive CAD.
Noninvasive tests like stress echocardiography and Perfusion testing with CMR or SPECT imaging should be used in identifying patients at risk, followed by further risk stratification by appropriate invasive testing aimed at identifying the etiology and planning further management to avert adverse cardiac events [10].
Limitations
Ours is a single centre retrospective study and we included only those patients who came to the department with ACS, this is no way represents the true burden of the disease in the population and hence, our results may not be interpreted as the true reflection of the CAD in the population. Intravascular ultrasound (IVUS), optical coherence tomography (OCT) or fractional flow reserve (FFR) was not used in this study.
Conclusion
CAD among women is increasing at an alarming rate; the disturbing factor is that it is affecting the young premenopausal women more than before. As the risk factor profile is different among the premenopausal women, it is imperative to identify the risk factors in these women at the earliest and treat them more aggressively to prevent future adverse cardiovascular events.
Even now, women with symptoms, who have “normal” or nonobstructive coronary angiography are being wrongly reassured. Several studies have shown that these patients continue to have symptoms and are rehospitalised, with majority of them undergoing repeat procedures and later on developing obstructive CAD.
The need of the hour is larger systematic analysis and randomised controlled trials to look into the pathophysiology of the CAD and proper understanding of the risk factor profile of the pre menopausal women and effective treatment options that can alleviate their symptoms and reduce the CAD burden of the society.
References
- Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics-2015 update: a report from the American Heart Circulation. 2015; 131: e29–e322.
- Enas EA, Senthilkumar A, Juturu V, et al. Coronary artery disease in women. Indian Heart 2001; 53: 282-292.
- Adão L, Santos L, Bettencourt Acute coronary syndromes in young women. Rev Port Cardiol. 2004; 23: 69-77.
- Sharaf BL, Pepine CJ, Kerensky RA, et Detailed angiographic analysis of women with suspected ischemic chest pain (pilot phase data from the NHLBI-sponsored Women’s Ischemia Syndrome Evaluation [WISE] Study Angiographic Core Laboratory). Am J Cardiol. 2001; 87: 937-941.
- Kennedy JW, Kilip T, Fisher LD, et al. The clinical spectrum of coronary artery disease and its surgical and medical management, The Coronary Artery Surgery study. Circulation 1982; 66: 16-23.
- Johnson BD, Shaw LJ, Pepine CJ, et al. Persistent chest pain predicts cardiovascular events in women without obstructive coronary artery disease: results from the NIH NHLBI sponsored Women’s Ischaemia Syndrome Evaluation (WISE) Eur Heart J 2006; 27: 1408-1415.
- Shaw LJ, Merz CN, Pepine CJ, et The economic burden of angina in women with suspected ischemic heart disease: results from the National Institutes of Health National Heart, Lung, and Blood Institute sponsored Women’s Ischemia Syndrome Evaluation. Circulation. 2006; 114: 894-904.
- Oomman A, Sathyamurthy I, Ramachandran P. Profile of female patients undergoing coronary angiogram at a tertiary J Assoc Physicians India. 2003; 51: 16-19.
- Dave TH, Wasir HS, Prabhakaran D. Profile of coronary artery disease in Indian women: correlation of clinical, non invasive and coronary angiographic findings. Indian Heart J. 1991; 43: 25-29.
- Raffaele Bugiardini, Noel Bairey Merz Angina With “Normal” Coronary Arteries. A Changing Philosophy. JAMA. 2005; 293: 477-484.
- Hochman JS, Tamis JE, Thompson TD, et Global Use of Strategies to Open Occluded Coronary Arteries in Acute Coronary Syndromes IIb Investigators. Sex, clinical presentation, and outcome in patients with acute coronary syndromes. N Engl J Med. 1999; 341: 226-232.
- Glaser R, Herrmann HC, Murphy SA, et Benefit of an early invasive management strategy in women with acute coronary syndromes. JAMA. 2002; 288: 3124-3129.
- Hochman JS, McCabe CH, Stone PH, et al. Outcome and profile of women and men presenting with acute coronary syndromes: a report from TIMI J Am Coll Cardiol. 1997; 30: 141-148.
- Krumholz HM, Douglas PS, Lauer MS,et Selection of patients for coronary angiography and coronary revascularization early after myocardial infarction: is there evidence for a gender bias? Ann Intern Med. 1992; 116: 785- 790.
- Diver DJ, Bier JD, Ferreira PE, et Clinical and arteriographic characterization of patients with unstable angina without critical coronary arterial narrowing (from the TIMI-IIIA Trial). Am J Cardiol. 1994; 74: 531-537.
- Kemp HG, Kronmal RA, Vlietstra RE, et Seven year survival of patients with normal or near normal coronary arteriograms: a CASS registry study. J Am Coll Cardiol. 1986; 7: 479-483.
- Kaski JC, Rosano GM, Collins P, et al. Cardiac syndrome X: clinical characteristics and left ventricular function. Long- term follow-up J Am Coll Cardiol. 1995; 25: 807-814.
- Johnson BD, Shaw LJ, Buchthal SD, et Prognosis in women with myocardial ischemia in the absence of obstructive coronary disease: results from the National Institutes of Health-National Heart, Lung, and Blood Institute-sponsored Women's Ischemia Syndrome Evaluation (WISE). Circulation. 2004; 109: 2993-2999.
- Panza JA. Myocardial ischemia and the pains of the heart. N Engl J 2002; 346: 1934-1935.
- Kwok Y, Kim C, Grady D, et al. Meta-analysis of exercise testing to detect coronary artery disease in women. Am J 1999; 83: 660-666.
- Kohli P, Gulati M. Exercise stress testing in women: going back to the basics. Circulation 2010; 122: 2570-2580.
- Panting JR, Gatehouse PD, Yang GZ, et Abnormal subendocardial perfusion in cardiac syndrome X detected by cardiovascular magnetic resonance imaging. N Engl J Med. 2002; 346: 1948-1953.
- Reynolds HR, Srichai MB, Iqbal SN, et al. Mechanisms of myocardial infarction in women without angiographically obstructive coronary artery disease. Circulation 2011; 124: 1414–1425.
- Doyle M, Fuisz A, Kortright E, et The impact of myocardial flow reserve on the detection of coronary artery disease by perfusion imaging methods: an NHLBI WISE study. J Cardiovasc Magn Reson. 2003; 5: 475-485.
- Reis SE, Holubkov R, Conrad Smith AJ, et al. Coronary microvascular dysfunction is highly prevalent in women with chest pain in the absence of coronary artery disease: results from the NHLBI WISE study. Am Heart J. 2001; 141: 735-
- Reis SE, Holubkov R, Lee JS, et al. Coronary flow velocity response to adenosine characterizes coronary microvascular function in women with chest pain and no obstructive coronary disease: results from the pilot phase of the Women's Ischemia Syndrome Evaluation (WISE) J Am Coll Cardiol. 1999; 33: 1469-1475.