Assessment and Comparison of The Slippage and Unintentional Opening of Epidural Catheters and Their Connectors
Author'(s): Antonio Gonzalez Fiol, MD1*, Robert Horvath, PhD, MBA2, Sunil Kumar Dhar, Ph.D3 and Alian, Aymen, MD4
1Assistant Professor, Department of Anesthesiology, Yale, New Haven Hospital, New Haven, Connecticut.
2Laboratory Manager Dept. of Material Science and Engineering,President, B.Horvath, LLC, Department of Materials Science and Engineering, Rutgers University, Piscataway, New Jersey
3Professor, Department of Mathematical Sciences, New Jersey Institute of Technology, Newark, New Jersey.
4Associate Professor, Department of Anesthesiology, Yale, New Haven Hospital, New Haven, Connecticut.
*Correspondence:
Antonio Gonzalez Fiol, MD, Assistant Professor, Department of Anesthesiology, Yale, New Haven Hospital, New Haven,Connecticut, 333 Cedar Street, TMP 3, New Haven, CT 06510,Tel: 413-386-9415, Fax: 203-785-6664.
Received: 29 November 2020; Accepted: 22 December 2020
Citation: Fiol AG, Horvath R, Dhar SK, et al. Assessment and Comparison of The Slippage and Unintentional Opening of Epidural Catheters and Their Connectors. Anesth Pain Res. 2020; 4(3): 1-6.
Abstract
The unintended disconnection of epidural catheters from their connector may result in inadequate analgesia and increase risk of infection, among others. In order to provide quality improvement, all factors associated with such disconnections must be evaluated, including both operator expertise and manufacturer flaws. This study was created to evaluate the latter in hopes of providing objective data as to which brand of catheters are more prone to detach from the epidural catheter.
Methods: This study compared both the force needed to dislodge (unintended disengagement) the connector fromthe catheter, and to cause the connector to open (unintended opening). We evaluated three brands of catheters: B- Braun Perifix, Smith Portex, and the Arrow. To assess the aforementioned forces we utilized the Applied Test System (ATS) tensile test apparatus and fixed the catheters to the machinery and exerted a quantitative force until the catheter either slipped or the connecter was forced open. In addition, we evaluate the efficacy of the proposed use of a piece of adhesive to prevent unintentional catheter disconnection. Each catheter type was tested 10 times to assess for variability.
Results: The amount of force needed to cause the unintentional disconnection for the B. Braun Perifix, Smith Portex Epifuse and Arrow catheters was 8.127 Newtons, 8.310 Newtons, and 4.183 Newtons, respectively. The p-values comparing the B. Braun to Smith (p=0.432), B. Braun to Arrow (p<0.0001), and Smith to Arrow (p<0.0001). The amount of force needed to cause the catheter connector to open for the B. Braun Perifix, Smith Portex Epifuse and Arrow catheters was 29.251 Newtons, 32.518 Newtons, and 4.403 Newtons, respectively. The p-values comparing the connector opening of B. Braun to Smith (p=0.0021), B. Braun to Arrow (p<0.0001), and Smith to Arrow (p<0.0001).
Conclusions: When comparing all three catheter types, the mechanical integrity of the Arrow appears be inferior to both the B. Braun and Smith Portex catheter for both disconnection and connector opening. No significant difference was noted between B. Braun and the Smith catheters when assessing catheter-connector disconnection. The Smith Portex catheter proved to be the strongest catheter when assessing connector opening forces. The B-Braun and the Smith catheter benefited from the use of adhesive when assessing opening forces, whereas the B-Braun showed no benefit when gaging disconnection forces. The use of the SnaplockTM adaptor is highly recommended when using the Arrow catheter.
Keywords
Introduction
With the increased use of epidural catheters in perioperative pain management, and in the peripartum period, there has been an increased recognition of unintended epidural catheter disconnection [1-4]. Some authors consider this incident to be the most common, yet under reported complication of epidural analgesia used for the postoperative and labor pain control [2,4]. Its actual incidence is unknown. At least one group has estimated a 5% incidence during a three month audit in their surgical population [3]. Unintended epidural catheter disconnections may result in patient discomfort and potential morbidity [3-6].
Epidural connector disengagement from its catheter will result in the inability to use the catheter for provision of analgesia which may lead to patient dissatisfaction and the exposed catheter may increase morbidity. Bacterial contamination of the epidural space or central nervous system may ensue secondary to disconnection [3-6]. When managing an intrathecal catheter, the integrity of the connector with the catheter is of utmost importance, at least one case report document the loss of cerebrospinal fluid, secondary to a catheter-connector disengagement [7]. Given the morbidity associated with an exposed catheter secondary to unintentional disconnection, in the anticoagulated patients, anesthesiologists must weigh the benefits of removing a catheter outside of guideline recommendations against the potential risk of epidural space contamination. The morbidity associated with the unintended and or untimely epidural catheter disconnections highlights the need to understand the strengths and mechanical flaws associated with some of the epidural catheter connectors currently on the market. Ideally a disconnection-resistant connector should be utilized.
In an effort to determine the catheter with the greatest strength and resistance to disconnection, we studied the force needed to cause an unintentional disconnection between the catheter-connector bonding and connector opening forces in three brands of epidural catheters available at our institution. The use of an adhesive around the connector-catheter junction has been suggested to decrease the incidence of unintentional disconnections [4]. We tested the effects of the latter over the forces involved for unintentional disconnect and opening of the catheter-connector bonding. Our primary outcomes were determining the amount of force needed to cause a disconnection of the epidural catheter from its connector (unintentional disconnection) or to cause the connector to open (unintentional opening), between three leading brands in the neuraxial anesthesia market. The secondary outcomes were to test if the proposed use of and adhesive protects against epidural catheter disconnections (unintentional connector opening and disconnect). We hypothesize that the forces needed to cause the catheter connector to unintentionally disengage from its connector are similar among the three studied brands, and that the use of adhesive would result in the need of higher forces to cause an unintentional disconnect or opening of the connector-catheter bonding.
Methods
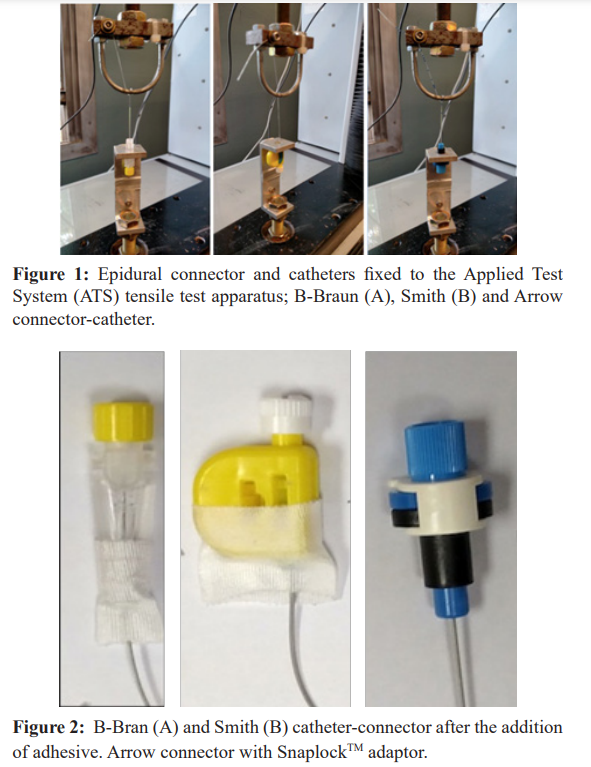
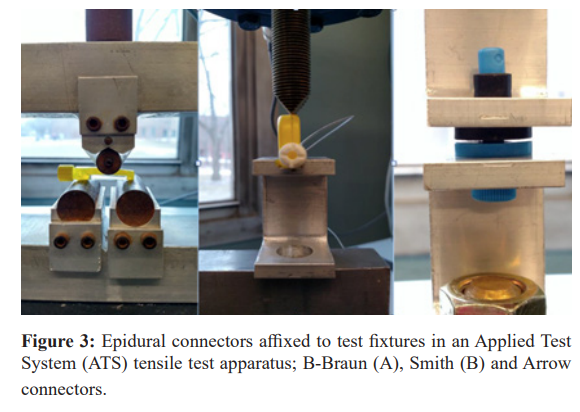
In order to test the bonding forces between connector and catheter (unintentional disconnection), three brands of flexible epidural catheters (polyurethane, FlexTip Plus®, open tip catheter, uniport [Arrow International, Reading, PA]; pebax nylon, Duraflex®, closed tip, multiport [Smiths Medical, St. Paul, MN]; polyamide nylon, Perifix® FX Springwound, closed tip, multiport [B. Braun Medical, Melsungen GA, Germany]) were fully inserted into the connectors and secured. The integrity of the connection was tested by injecting saline through the catheter. The connector and the catheter were then fixed to opposing specially designed tensile test fixtures (Figure 1A-C) that were installed in an Applied Test System (ATS) tensile test apparatus. The fixtures were designed making use of a curved attachment point for the catheter anchoring and specially designed connector anchors to pull the catheter from the connector assembly at a rate of 200mm/min, consistent with guidelines from ASTM D638 “Tensile Testing of Plastics”. Force was applied to the catheter (measured in Newtons), and gradually increased. The peak force at which the catheter completely slips from the connector was recorded. This was conducted ten times for each brand of catheter to ensure that the results were reproducible and not incidental. This procedure was then replicated after adhesive was applied around the Smith and B-Braun catheter- connector. For the analysis of the Arrow catheter, the SnaplockTM adaptor was used (Figures 2a-c).
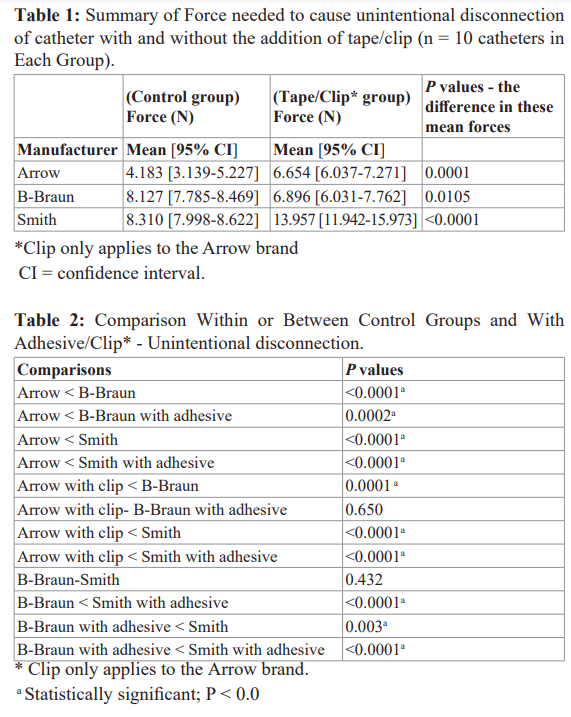
During the second portion of this study we examined the compressive force required to open the connector device. The epidural connectors were affixed to opposing specially designed test fixtures installed in an ATS tensile test apparatus (Figure 3a- c). The fixtures were designed making use of various geometries to best apply a normal force to connectors in a method considered typical to a potential unintentional opening failure. The assembly was injected with saline prior to testing. A load was applied at a rate of 200mm/min consistent with guidelines from ASTM D638 “Tensile Testing of Plastics”. The tensile load was applied to the central axis of the connector; the lower fixture remained stationary. All the samples were positioned in a test fixture and the load required to open the connector was measured ten times for each catheter type. The above-mentioned procedure was repeated after adhesive was applied around the Smith and B-Braun catheter- connector. For the Arrow catheter, the SnaplockTM adaptor was used.
All the measurements/tests were performed by an independent laboratory in the Department of Materials Science and Engineering at Rutgers University, Piscataway, NJ.
Statistical Analysis
In our previous experience with tensile strength of epidural catheters [10], we had already conducted our pilot study with 10 catheters per group and brand. Therefore, the same sample size (total of thirty observations) was used for our pilot studies in this research. A sample size determination study was made using power analysis involving the test of equal means under unequal variances (weighted least square method) due to the results from the pilot study summary statistics. The pilot data based population parameters for true mean and variance for unintentional opening for the brands B-Braun, Smith, and Arrow, are as follows. The means are given by 29.251, 32.518, and 4.403, and the variances by 10.30743222, 1.908928889, and 0.321379, respectively. These mean parameters being so far apart and the individual standard deviations being so small yields only 2 data points per brand for a power of at least 0.999, i.e., a total of six observations, with alpha = 0.05. However, the pilot data based population parameters for true mean and variance for unintentional disconnection for the brands B-Braun, Smith, and Arrow, are as follows. The means are given by 8.127, 8.31, and 4.183, and the variances by 0.290756667, 0.242733333, and 2.710867778, respectively. These mean parameters relatively speaking are not so far apart as compared to the unintentional opening but still one of the means is twice the other and the individual standard deviations are more close to one another but unequal, therefore four data points per brand yields a power of at least 0.999, i.e., a total of twelve observations, with alpha = 0.05. Thus, putting the two power analyses together, our results suggested a sample size of 4 per brand (i.e., a total of twelve observations) with a power > 0.999 for both the equality of mean tests, with each alpha = 0.05. Since, this power analysis was conducted based on the pilot studies with ten catheters per brand (i.e., a total of thirty observations) although in posterity total of twelve would have sufficed, going with a sample size that would give almost a guaranteed power with a sample size of ten catheters per brand (i.e., a total of thirty observations), similar to the initial pilot study made much more sense and was implemented.
Comparisons were made by 2-way ANOVA, using a 3 (number of brands) x 2 (control group versus experimental group- catheters plus tape/SnaplockTM adaptor) factor ANOVA, where each group had n = 10. This analysis was repeated for slippage and unintentional opening which included the unintentional disconnection without adhesive (control) versus the unintentional disconnection with tape group, as well as the unintentional opening without tape versus the unintentional opening with tape. Statistical analysis was performed using SAS system 9.4 for Windows (SAS Institute Inc., Cary, NC). There were no direct pairwise tests such as t-tests planned or implemented. Although, p-values < 0.05 was considered statistically significant, p-values in the two 2-way ANOVA multiple, whenever significance in multiple comparison was found p-values < 10-4 =0.0001 So with six comparison, a Bonferroni type correction would maintain the overall familywise error rate of type I error at much below 0.05.
Results
Unintentional Disconnection
The mean force required to cause catheter disconnection for the B. Braun, Smith and Arrow catheters (control groups) expressed in Newtons (N) was 8.127, 8.310 and 4.183, respectively (Table 1). A Statistical difference was noted when comparing the Arrow against the B-Braun (P <0.0001) and Smith catheters (P <0.0001) (Table 2). No statistical difference was noted between B. Braun to the Smith catheters control groups (p-value 0.431).The addition of adhesive to the Smith catheter, resulted in an increase in the force needed to cause disengagement when compared to its control group (13.957 N, P < 0.0001). This force proved to be statistically superior to those of the Arrow and B-Braun control group catheters (P< 0.0001 and P<0.0001 respectively), Arrow with SnaplockTM adaptor (6.654 N, P<0.0001), and B-Braun with adhesive (6.897N, P<0.0001).
On the contrary, the B-Braun catheter with adhesive showed a decrease in the force required for disconnection (6.897 N, P= 0.0105). This decrease resulted in a statistically significant difference when compared to the Arrow and Smith control groups (P = 0.0002 and P =0.003 respectively), whereas no difference was noted when compared to the Arrow with SnaplockTM adaptor (P= 0.650). The use of the commercially available Arrow SnaplockTM adaptor increased the force needed for disengagement when compared to its control group (P = 0.0001). Despite this increase in force, this catheter proved to be inferior to the B-Braun (P = 0.0001), Smith and Smith with adhesive (P < 0.0001 and P < 0.0001 respectively) when assessing catheter-connector disconnection.
Of note, all the catheters tested (n=60) for unintentional catheter- connector disconnection dislodged from their connector. That is, none of the catheters tested fractured when tension was applied as described in the methods section.
When assessing the forces expressed as the mean in Newtons (N) needed to cause unintentional connector opening, the order was Smith (32.518) > B. Braun (29.251) > Arrow (4.403). The Smith catheter was statistically superior to the Arrow and B-Braun catheters (P<0.0001 and 0.0021 respectively). Whereas the B-Braun catheter showed to be superior to the Arrow catheter (P<0.0001). (Table 3) When measuring the impact of the adhesive over the catheter-connector, a significant increase in the force required to open the connector systems was noted. The force required to open the connector with adhesive/SnaplockTM adaptor was Smith (111.816 N)> Arrow with SnaplockTM adaptor (98.100 N) > B-Braun with adhesive (43.297 N). When comparing the force needed to open the B-Braun and Smith connectors with adhesive to their respective control group, the former showed statistically significant superiority (P < 0.0001 and P < 0.0001). The addition of the SnaplockTM adaptor to the Arrow connector also conferred strength to this connector (P < 0.0001).
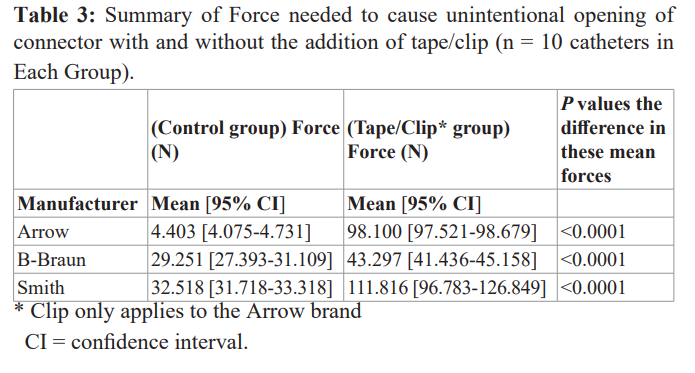
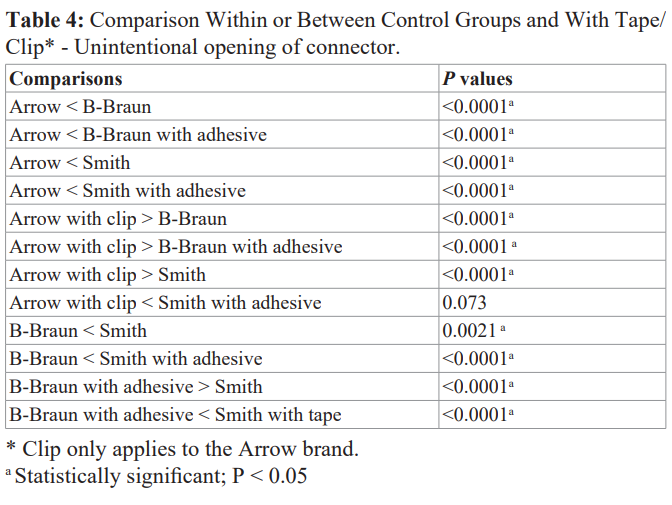
When comparing between brands, the Smith catheter with adhesive showed superior strength when compared to the Arrow (P< 0.0001), and the B-Braun control group and with adhesive (P < 0.0001 and P< 0.0001 respectively). The addition of the Snaplock adaptorTM to the Arrow connector conferred superiority over the B-Braun (P < 0.0001), B-Braun with adhesive (P < 0.0001) and Smith (P < 0.0001) connectors. Similarly, the use of adhesive over the B-Braun connector conferred a statistically significant advantage over the Arrow (P < 0.0001) and Smith (P < 0.0001) control groups. (Table 4) No statistical difference was noted when comparing the Smith with adhesive to the Arrow with snaplock adaptor (P = 0.73).
Discussion
With the advent of Enhanced Recovery after Surgery (ERAS), the use of perioperative epidurals is likely to increase. The analgesic benefits aimed by the ERAS protocols include decrease pain scores and opioid consumption [8]. To achieve these goals and to avoid morbidity, the integrity of the epidural catheter-connector is essential. Hence, we evaluated the force needed to cause unintentional disconnection of the catheter-connector bonding by applying tension on the system which would clinically resemble the tension created by patient movement. We also evaluated the external force that would lead to opening the connector, all of which were specifically designed for each connector. Lastly, we evaluated a clinician-engineered alternative proposed by Galvin et al.[4]; the use of a piece of adhesive attached around the catheter- connector bonding- to avoid untimely disconnection. Limited studies have attempted to delineate between equipment failure and operator expertise [3,5]. However, even with careful practitioner technique, catheter dysfunction may occur; thus, we designed this study to evaluate the reliability of the equipment we regularly use.
Our study demonstrates that under ideal conditions the B-Braun and Smith catheters connectors are equivalent regarding the force needed to cause an unintentional catheter-connector disconnection. The Arrow catheter showed to have the weakest catheter-connector bonding. During our unintentional disconnection evaluation, we noted that none of the catheters fractured when tension was applied, they all slipped out of the connector. We speculate that the tension of these flexible catheters results in thinning of the catheter which facilitates the catheter dislodging from its connector.
A previous study, by Richardson et al. [5], compared two Smith type of connectors (Tuohy Borst and EpifuseTM). They reported disconnection forces ranging from 11.4-16.6 Newtons for the Tuohy Borst and the EpifuseTM respectively, which are higher than the forces we describe. The difference between our results relies in the methodology used to measure the force of disconnection. Richardson et al. used an initial load of 5N for 2 min and then increased progressively increased it by 15 N.min-1, whereas we applied a load at a rate of 200mm/min. These technical differences alienate comparisons between these studies.
The patient dissatisfaction and morbidity associated with the untimely epidural disconnection has led some authors to propose alternatives to secure the catheter-connector bonding. These include the use of cyanoacrylate ester (“super glue”) [9], or securing the epidural catheter into the connector with a piece of adhesive4 among others. Hence, we were inclined to evaluate the impact of the addition of adhesive and the SnaplockTM adaptor as we thought this would be an easy and safe clinical alternative to utilize. Our results suggest that the simple addition of adhesive or SnaplockTM adaptor increased the forces needed for disconnection from a range of 4.183-8.310 N to 6.654-13.957N.
The addition of adhesive to the Smith catheter resulted in an increase in the force needed to cause unintentional disconnection. When evaluating the effects of the commercially available SnaplockTM adaptor, an increase in force needed to cause disconnection was recorded. On the contrary, the B-Braun catheter showed a reduction in the force needed for disconnection. Clinically speaking, the Smith and Arrow catheter benefited from the use of adhesive and the SnaplockTM adaptor respectively, whereas the B-Braun catheter did not benefit from the use of adhesive. The force needed to disconnect the Arrow catheter-connector without the SnaplockTM adaptor was noted to be 50-70% less than that of its competitors with or without the use of adhesive. The addition of the SnaplockTM adaptor decreased this difference to approximately 20% when compared to the B-Braun and Smith control group. Potentially, the use of adhesive may also provide a last check point, increasing the detection of human errors upon initial catheter-connector connection.
Besides catheter-connector disconnection secondary to tension or pulling of the catheter, we evaluated the forces needed to open the connectors. Our study demonstrates that these forces fluctuated from 4.403-32.518 N. The Arrow connector showed to require the least amount of force to open the connector, whereas the Smith connector was the strongest. Clinically, we think it would be difficult to reproduce an external force to open the Smith connector, as this force would require to be applied with a wedge shape object. The addition of adhesive to the B-Braun and Smith catheter significantly increased the forces needed to unintentionally open these catheter connectors; an increase in force of 48% and 243% respectively, was noted. In the case of the Arrow catheter, the addition of the SnaplockTM adaptor significantly increased the opening force by a factor of approximately 22. Hence, when evaluating connector opening forces, all catheters studied benefited from the use of a piece of adhesive or the SnaplockTM adaptor.
There are few limitations to our study. Although our study for unintentional disconnections was designed to resemble the movement of a patient leading to catheter tension, we cannot assure that patient movement would resemble a load of 200mm/ min. It is possible that the actual tension may be higher. We did not measure the force needed cause a disconnection between the filter and connector, as previously described by Doyle et al. [3]. Our study was performed under ideal conditions, using new and undamaged catheters/connectors. When measuring the forces needed to cause connector opening, we cannot assure that there are other angles or vectors of force that may cause connector opening. Besides, we did not account for human errors upon catheter- connector assembly. Lastly, our power analysis was performed to detect differences between the means of the control groups for both unintentional disconnection and opening. It is possible that more catheters would be needed to detect a difference between the means of the control groups and the catheters with the addition of adhesive.
In conclusion, there appears to be a discrepancy in the strength of the various epidural catheter-connector bonding utilized at our institution for the management of perioperative pain. When comparing all three catheter types, the Arrow brand happens to be inferior to both the B. Braun and Smith catheters when gaging unintentional disconnection and opening by approximately 50% and 85% respectively. The use of the SnaplockTM adaptor significantly improve the mechanical properties of this catheter brand, reducing this difference to 20% for unintentional disconnection and improving its strength by a factor of 22 for connector opening. The B-Braun and Smith catheter were comparable when assessing unintentional disconnection forces. The Smith catheter showed to have the best catheter-connector bonding after a piece of adhesive was used. The latter brand showed to be superior when unintentional opening forces were evaluated. All connectors benefited from the addition of a piece of adhesive when analyzing unintentional opening forces. Given the importance to maintain the integrity of the epidural catheter-connector, manufacturers of the leading brand should design epidural catheter adaptors to aim at decreasing the amount of tension and at the same time improving catheter-connector bonding (i.e Statlock® epidural stabilization device).
Financial disclosures: Departmentally funded.
*A portion of this work was presented at the 2015 American Society of Regional Anesthesia, Las Vegas, Nevada.
References
1.Philip A, Bourne TM. Epifuse™ failure causing epidural disconnection. Anaesthesia. 2012; 67: 306-307.
2.Lubenow TR, Ivankovich AD. Postoperative epidural analgesia. Crit Care Nurs Clin North Am. 1991; 3: 25-34.
3.Doyle A, Santhirapala R, Stimpson J, et al. A comparison of two epidural catheter connectors. Int J Obstet Anesth. 2011; 20: 34-37.
4.Gavelin RJ, Patterson KW. Epidural catheter disconnections.Can J Anesth. 1993; 40: 468-468.
5.Richardson PB, Turner MW, Wilkes AR. Epidural catheter connectors: a laboratory-based comparison of the Portex Tuohy-Borst and EpiFuse™ designs. Anaesthesia. 2012; 67: 1119-1124.
6.Langevin PB, Gravenstein N, Langevin SO, et al. Epidural Catheter Reconnection Safe and Unsafe Practice. Anesthesiology. 1996; 85: 883-888.
7.Cohen S, Stricker P, Sakr A. Cerebrospinal fluid leak after disconnection of an intrathecal catheter adapter placed after accidental dural puncture. Reg Anesth Pain Med. 2005; 30: 591.
8.Miller TE, Thacker JK, et al. Reduced Length of Hospital Stay in Colorectal Surgery after Implementation of an Enhanced Recovery Protocol. Anesth Analg. 2014; 118: 1052-1061.
9.Aldrete JA. Securing epidural catheters to Tuohy connectors. Anesthesiology. 1995; 82: 320.
10.Gonzalez Fiol A, Horvath R, Schoenberg C, et al. Comparison of Changes in Tensile Strength in Three Different Flexible Epidural Catheters Under Various Conditions. Anesth Analg. 2016; 123: 233-237.