Assessment of Attitudes towards People Living with HIV/Aids in North Central Nigeria
Author'(s): Chiwa Musa Dalah*
Department of Mathematics & Statistics, Yobe State University, Damaturu, Nigeria.
*Correspondence:
Chiwa Musa Dalah, Department of Mathematics & Statistics,Yobe State University, Damaturu, Nigeria.
Received: 22 December 2020; Accepted: 17 January 2021
Citation: Dalah CM. Assessment of Attitudes towards People Living with HIV/Aids in North Central Nigeria. Clin Immunol Res. 2021; 5(1): 1-7.
Abstract
Previous researches has established that awareness and knowledge of HIV/AIDS in Northcentral Nigeria is high, but still people living with HIV/AIDS may face some sort of negative attitudes from family member and non-family members. This work has assessed the level of attitudes (stigmatization and discrimination) faced by people living with HIV in Northcentral Nigeria. HIV-related stigma refers to negative beliefs, feelings and attitudes towards people living with HIV/AIDS, their families, people who work with them (HIV service providers), and members of groups that have been heavily impacted by HIV/AIDS, such as gay and bisexual men, homeless people, street youth, and mentally ill people while HIV discrimination refers to the unfair and unjust treatment of someone based on their real or perceived HIV status. North central Nigeria consists of six states and the Federal capital territory Abuja. The states are Benue, Plateau, Kwara, Nasarawa, Niger, and Kogi. Secondary data from federal ministry of health is used for the assessment.
Keywords
Introduction
Attitudes (Stigma and discrimination) associated with HIV relate to racism, derogatory perceptions, and violence towards people living with HIV and AIDS. According to UNAIDS [1,2], 35% of countries with available data estimate that more than 50% of individuals report discriminatory attitudes towards people living with HIV. Stigma and discrimination continue to be faced by those most at risk for HIV (key affected populations) based on their actual or perceived health status, race, socioeconomic status, age, sex, sexual orientation or gender identity, or other reasons. Stigma and discrimination manifest themselves in many ways. Please refer to Strangle A.L, et al. [3] for a systematic review of Stigma and discriminatory reduction strategies. Human rights violations may occur in health care settings, restricting people from taking health services, or enjoying quality health care. Family, acquaintances, and the broader population are shunned by some people living with HIV, and other primary customers are encouraged. In contrast, others face poor treatment in educational and work settings, erosion of their rights, and psychological damage.
The Stigma Index of People Living with HIV records the experiences of people living with HIV. As of 2015, the HIV Stigma Index was being used by more than 70 countries, or more than 1,400 persons living with HIV were trained as interviewers, and more than 70,000 people with HIV were interviewed. Huffington
[4] statistics, which were obtained from 50 countries in 2017, suggest that approximately Stigma and discrimination also make individuals vulnerable to precautionary guidelines for HIV. One of the eight people living with HIV is denied health services due to Stigma and racism. Fear of Stigma and prejudice is the key reason people are reluctant to get screened, reveal their HIV status, and prescribe antiretroviral drugs, referring to UNAIDS research [5,6] and the World Health Organization (WHO) [7,8] (ARVs). One analysis from the Well project [9] found that respondents with elevated prejudice levels were more than four significantly more likely to report inadequate care access. The leads to the rise of the global HIV epidemic and a higher number of deaths associated with AIDS. A reluctance to take an HIV test means that more people are diagnosed late when the infection may have already escalated to AIDS. The treatment less effective, increasing the likelihood of transmitting HIV to others and causing early death.
In the United Kingdom (UK), many individuals diagnosed with HIV are diagnosed at a late stage of infection, defined as a CD4 count below 350 within three months of diagnosis, according to the World Health Organization (WHO) report [8]. Although the late diagnosis of HIV in the UK declines from 56% in 2005 to 39% in 2015, this figure remains unacceptably high.
The PLHIV Stigma Index [10] in South Africa discusses the Stigma that prevented many young women from participating in an HIV prevention trial using vaginal gels and pills to help them remain HIV-free. Many indicated that they could be afraid that using these products would trigger them to be wrongly considered as having HIV. Furthermore, the fear of isolation and persecution were known as living with HIV will lead them to adapt to activities that placed them at higher risk of getting the virus.
The epidemic of fear, marginalization, and oppression has weakened individuals, societies, and societies' willingness to support them and provide support and encouragement to those affected. The initiatives to curb the infection, in no small way, hinder us. It complicates testing decisions, status disclosure, and the opportunity to share preventive activities, including family planning resources.
Forms of HIV stigma and discrimination
HIV and AIDS-related stigma can lead to discrimination, for example, when people living with HIV are prohibited from travelling, using healthcare facilities or seeking employment.
Self-stigma/internalized stigma
Self-stigma, or internalized stigma, has an equally damaging effect on the mental wellbeing of people living with HIV or from key affected populations. This fear of discrimination breaks down confidence to seek help and medical care. Self-stigma and fear of a negative community reaction can hinder efforts to address the HIV epidemic by continuing the wall of silence and shame surrounding the virus. Negative self-judgement resulting in shame, worthlessness and blame represents an important but neglected aspect of living with HIV. Self-stigma affected a person's ability to live positively, limits meaningful self-agency, quality of life, adherence to treatment and access to health services. In Zimbabwe, Trócaire and ZNNP+ designed, implemented and evaluated a 12-week pilot programme to support people living with HIV to work through self-stigmatising beliefs. After the 12 weeks, participants reported profound shifts in their lives. The majority of participants (61%) reported a reduction in self- stigma, depression (78%) and fears around disclosure (52%), and increased feelings of satisfaction (52%) and daily activity (70%). Evidence suggests people from key affected populations are also disproportionally affected by self-stigma. For example, a study of men in China who have sex with men found that depression experienced by participants due to feelings of self-stigma around homosexuality directly affected HIV testing uptake. Similarly, a study of men in Tijuana, Mexico who have sex with men found that self-stigma was strongly associated with never having tested for HIV, while testing for HIV was associated with identifying as being homosexual or gay and being more ‘out’ about having sex with men. In countries that are hostile to men who have sex with men and other key populations, innovative strategies are needed to engage individuals in HIV testing and care programmes without exacerbating experiences of stigma and discrimination.
Governmental stigma
A country’s discriminatory laws, rules and policies regarding HIV can alienate and exclude people living with HIV, reinforcing the stigma surrounding HIV and AIDS. In 2014, 64% of countries reporting to UNAIDS had some form of legislation in place to protect people living with HIV from discrimination. While, conversely, 72 countries have HIV-specific laws that prosecute people living with HIV for a range of offences. Criminalization of key affected populations remains widespread with 60% of countries reporting laws, regulations or policies that present obstacles to providing effective HIV prevention, treatment, care and support. As of 2016, 73 countries criminalised same sex activity, and injecting drugs use is widely criminalised, leading to high incarceration levels among people who use drugs. More than 100 countries criminalize sex work or aspects of sex work. Even in countries where sex work is at least partially legal the law rarely protects sex workers and many are at risk of discrimination, abuse and violence from both state and non-state actors such as law enforcement, partners, family members and their clients. For example, some 15,000 sex workers in China were detained in so- called custody and education centres in 2013. Laws that criminalize HIV non-disclosure, exposure and transmission perpetuate stigma and deter people from HIV testing and puts the responsibility of HIV prevention solely on the partner living with HIV. In May 2015, the Australian state of Victoria repealed the country’s only HIV- specific law criminalizing the intentional transmission of HIV. The repealed law - Section 19A of the Crimes Act 1958 - carried a maximum penalty of 25 years imprisonment, even more than the maximum for manslaughter (which is 20 years). The legislation to repeal the law was developed through the collaboration of several stakeholders, including legal, public health and human rights experts and representatives of people living with HIV. It was seen as a major step forward for the rights of people living with HIV.
Restrictions on Entry Travel and Stay
As of September 2015, 35 countries have laws that restrict the entry, stay and residence of people living with HIV. In 2015, Lithuania became the most recent country to remove such restrictions. As of 2015, 17 countries will deport individuals once their HIV positive status is discovered, five have a complete entry ban on people living with HIV and four require a person to be able to prove they are HIV negative before being granted entry. Deportation of people living with HIV has potentially life-threatening consequences if they have been taking HIV treatment and are deported to a country that has limited treatment provision. Alternatively, people living with HIV may face deportation to a country where they would be subject to even further discrimination - a practice that could contravene international human rights law.
Healthcare Stigma
Healthcare professionals can medically assist someone infected or affected by HIV, and also provide life-saving information on how to prevent it. However, HIV-related discrimination in healthcare remains an issue and is particularly prevalent in some countries. It can take many forms, including mandatory HIV testing without consent or appropriate counselling. Health providers may minimise contact with, or care of, patients living with HIV, delay or deny treatment, demand additional payment for services and isolate people living with HIV from other patients. For women living with HIV, denial of sexual and reproductive health and rights services can be devastating. For example, 37.7% of women living with HIV surveyed in 2012 in a six-country study in the Asia–Pacific region reported being subjected to involuntary sterilization. Healthcare workers may violate a patient’s privacy and confidentiality, including disclosure of a person’s HIV status to family members or hospital employees without authorization. Studies by WHO in India, Indonesia, the Philippines and Thailand found that 34% of respondents reported breaches of confidentiality by health workers. People from key affected populations may face additional discrimination in healthcare settings. Discriminatory attitudes held by health providers may also lead them to make judgements about a person’s HIV status, behaviour, sexual orientation or gender identity, leading individuals to be treated without respect or dignity. These views are often fueled by ignorance about HIV transmission routes among healthcare professionals. In 2012, half of all people living with HIV in Thailand were starting treatment very late and had CD4 counts under 100. HIV stigma was identified as a major barrier to service uptake so health authorities set a target to cut HIV-related stigma and discrimination by 50% by 2016. The Ministry of Public Health found that over 80% of healthcare workers had at least one negative attitude to HIV, while roughly 20% knew colleagues who were unwilling to provide services to people living with HIV or provided them substandard services. More than half of respondents reported using unnecessary personal protection measures such as wearing gloves when interacting with people living with HIV. 25% of people living with HIV surveyed said that they avoided seeking healthcare for fear of disclosure or poor treatment, while a third had their status disclosed without their consent. In response to these findings, the Ministry of Public Health, in collaboration with civil society and international partners developed initiatives to sensitize healthcare workers in both clinical and non-clinical settings. Early results in 2014 indicated that improving the attitude of healthcare workers doesn’t just improve care for people living with HIV but has wider societal benefits as they are seen as role models. As of 2017, Thailand had collected data from 22 provinces. The Thai Ministry of Public Health is rolling out an accelerated system-wide stigma reduction programme, in collaboration with civil society and concerned communities.
A study of health providers in urban health facilities in India found 55-80% of providers displayed a willingness to prohibit women living with HIV from having children, endorsed mandatory testing for female sex workers (94-97%) and stated that people who acquired HIV through sex or drugs "got what they deserved" (50-83%). These experiences may leave people living with HIV and people from key affected populations too afraid to seek out healthcare services, or be prevented from accessing them – for instance, if a nurse refuses to treat a sex worker after finding out about their occupation. It also prevents many people from key affected populations being honest with healthcare workers if they’re a sex worker, have same-sex relations, or inject drugs, meaning they are less likely to get services that could help them.
Employment Stigma
In the workplace, people living with HIV may suffer stigma from their co-workers and employers, such as social isolation and ridicule, or experience discriminatory practices, such as termination or refusal of employment. Evidence from the People Living with HIV Stigma Index suggests that, in many countries, HIV-related stigma and discrimination are as frequently or more frequently a cause of unemployment or a denial of work opportunity as ill health. Key findings from people living with HIV in nine countries across four regions in 2012 found that, as a result of their HIV status, between 8% (Estonia) and 45% (Nigeria) of respondents had lost their job or source of income; between 5% (Mexico) and 27% (Nigeria) were refused the opportunity to work, and between 4% (Estonia) and 28% (Kenya) had the nature of their work changed or had been refused promotion. In addition, 8% of respondents in Estonia to 54% in Malaysia reported discriminatory reactions from employers once they were aware of the employee’s HIV status. Similarly, 5% in Estonia to 54% in Malaysia reported discriminatory reactions from co-workers who became aware of their colleague’s HIV status. It is always in the back of your mind, if I get a job, should I tell my employer about my HIV status? There is a fear of how they will react to it. It may cost you your job; it may make you so uncomfortable it changes relationships. Yet you would want to be able to explain about why you are absent, and going to the doctors.
By reducing stigma in the workplace (via HIV and AIDS education, offering HIV testing, and contributing towards the cost of ARVs) employees are less likely to take days off work, and be more productive in their jobs. This ensures people living with HIV are able to continue working.
Community and Household Level Stigma
Community-level stigma and discrimination towards people living with HIV can force people to leave their home and change their daily activities. In many contexts, women and girls often fear stigma and rejection from their families, not only because they stand to lose their social place of belonging, but also because they could lose their shelter, their children, and their ability to survive. The isolation that social rejection brings can lead to low self-esteem, depression, and even thoughts or acts of suicide. The International Center for Research on Women (ICRW) reports that in Bangladesh more than half of women living with HIV have experienced stigma from a friend or neighbour and one in five feel suicidal. In the Dominican Republic, six out of ten women were living with HIV fear being the subject of gossip, while in Ethiopia, more than half of all women living with HIV report having low self-esteem. They [my family] were embarrassed and didn’t want to talk to me. My mother essentially said, ‘Good luck, you’re on your own.’ - Shana Cozad from Tulsa, USA, on her family’s reaction after she tested positive for HIV. A survey of married HIV-positive women (15–29 years) in India found 88% of respondents experienced stigma and discrimination from their family and community. Women with older husbands and from household’s with lower economic status were significantly more likely to experience stigma and discrimination from their husbands’ family as well as from friends and neighbours.
Stigma and discrimination can also take particular forms within community groups such as key affected populations. For example, studies have shown that within some lesbian, gay, bisexual, transgender and intersex (LGBTI) communities there is segregation between HIV-positive and HIV-negative people, where people associate predominately with those of the same status.
Ending HIV Stigma And Discrimination
To end HIV stigma and discrimination is very necessary so that people living with HIV/AIDS can feel free within the community. The use of specific programmes that emphasise the rights of people living with HIV is a well-documented way of eradicating stigma. As well as being made aware of their rights, people living with HIV can be empowered in order to take action if these rights are violated. Ultimately, adopting a human rights approach to HIV and AIDS is in the public’s interest. Stigma blocks access to HIV testing and treatment services, making onwards transmission more likely. The removal of barriers to these services is key to ending the global HIV epidemic.
In March 2016, UNAIDS and WHO’s Global Health Workforce Alliance launched the Agenda for Zero Discrimination in Healthcare. This works towards a world where everyone,
everywhere, is able to receive the healthcare they need with no discrimination, in line with The UN Political Declaration on Ending AIDS. Zero discrimination is also at the heart of the UNAIDS vision, and one of the targets of its Fast-Track response. This focuses on addressing discrimination in healthcare, workplace and education settings. Although Ghana’s Constitution protects all citizens from discrimination in employment, education and housing and ensures their right to privacy, there is ambiguity in the way these provisions apply to people living with HIV and to key affected populations.
Methodology
Study Design
In this study, secondary data from the Federal Ministry of health survey on NARSHS Plus carried out in 2012 were used. The data are tabulated according to various parameters and reasons/ facts which really need for analysis. The results are presented in tables and chart for easy understanding.
Main Results
Percentage Distribution of Respondents who have Heard of AIDs According to Attitude towards HIV Infected Family Members by State; FMoH, Nigeria, 2012.
From table 1 and figure 1, it is clear that the attitude of people towards family members who have been infected with HIV/AIDS is positively high in most of the states in north central Nigeria; this may be due to high level of education in the region.
Percentage Distribution of Respondents who have Heard of AIDs According to Attitude towards HIV Infected Family Members for Northcentral Nigeria; FMoH, Nigeria, 2012.
Table 2 and figure 2, has shown that the attitude of people to family members who have been infected with HIV/AIDS is generally high in Northcentral Nigeria.
From table 3 and figure 3, it is clear that the attitude to non- family members infected by HIV is relatively high in most of the states of
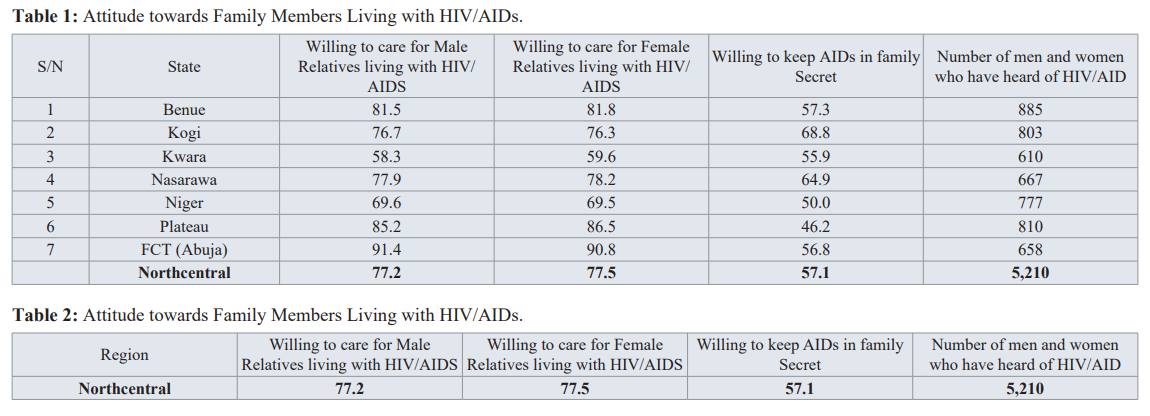
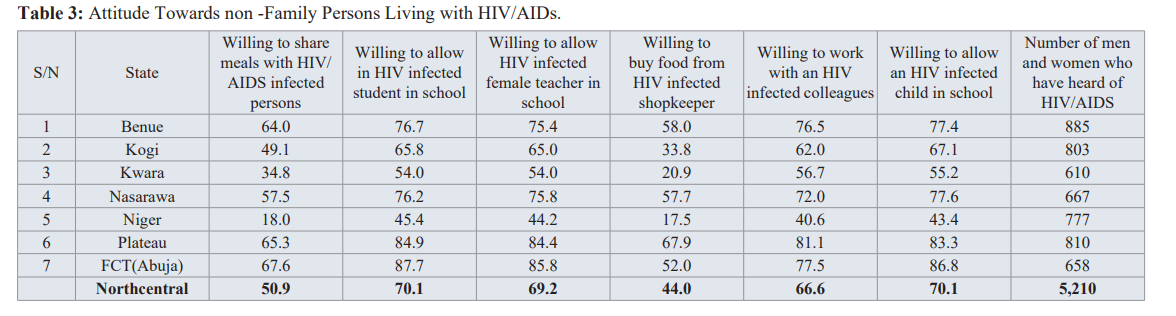
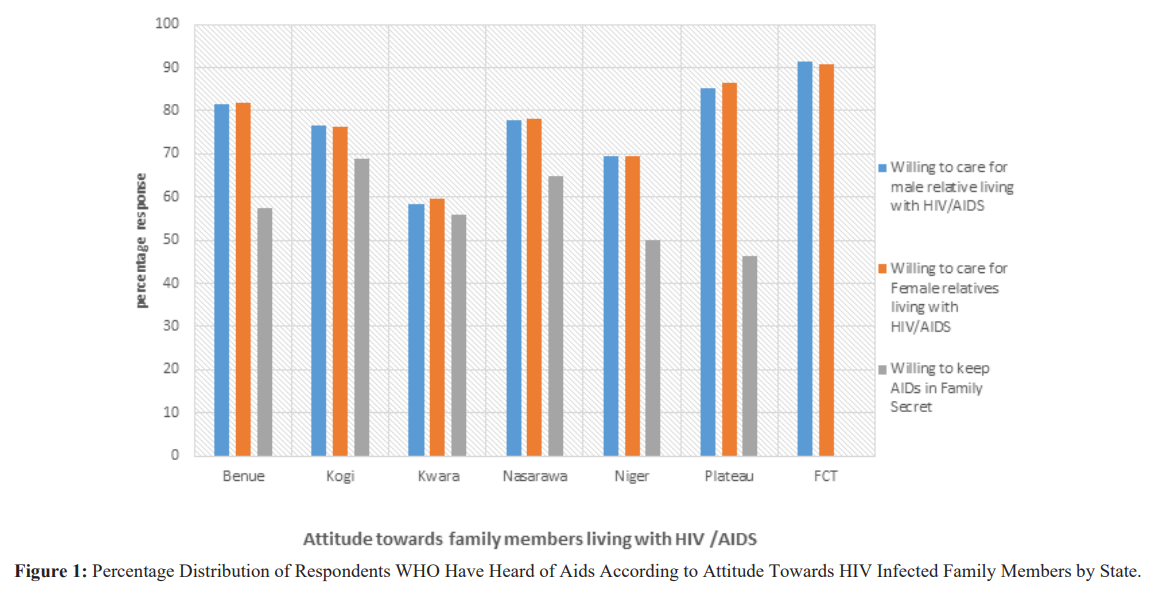
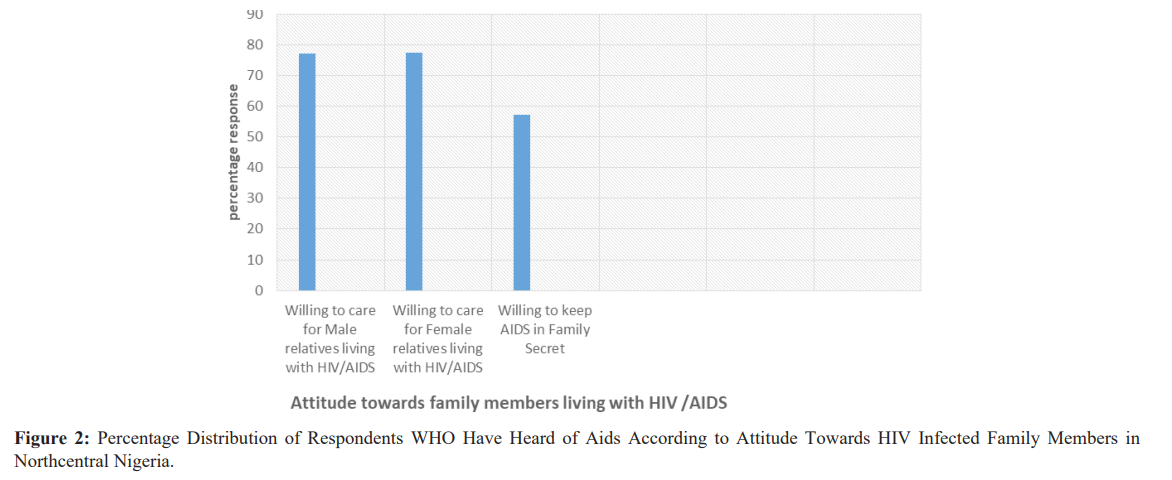
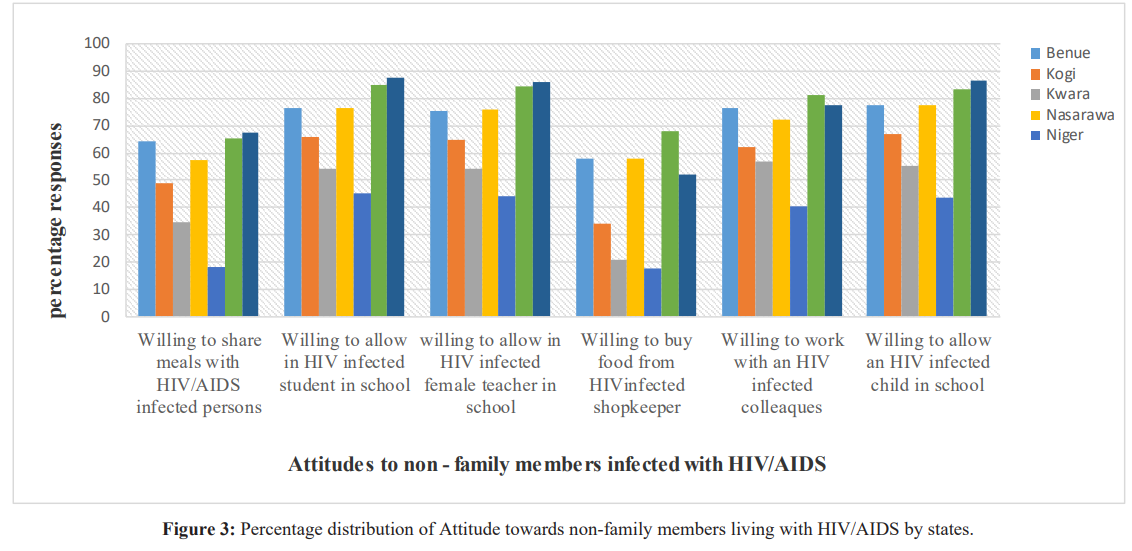
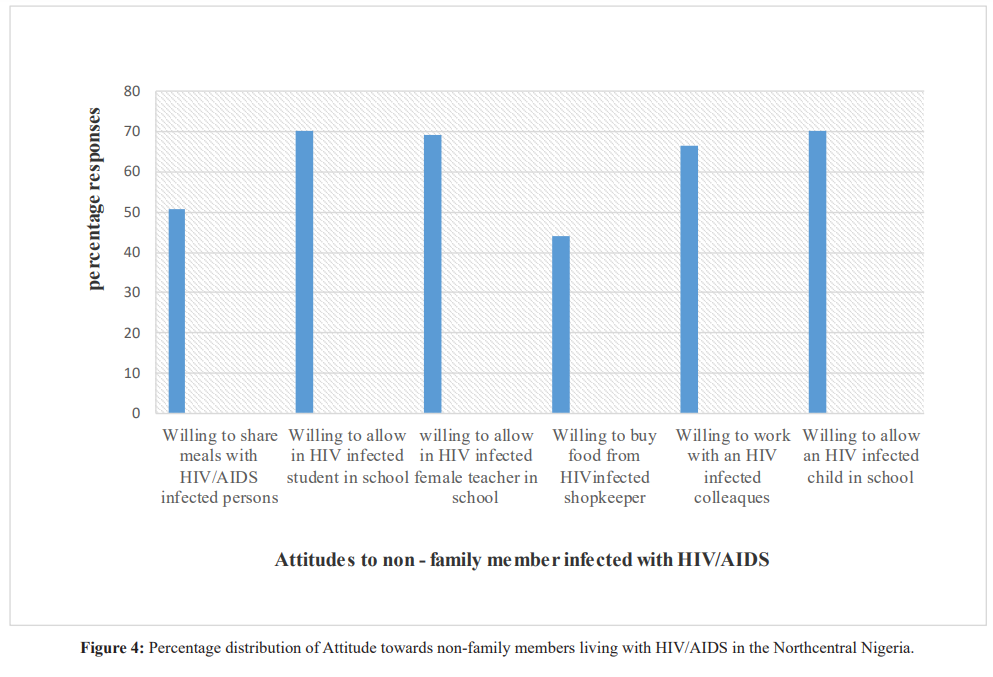
Table 4 and figure 4, has shown that the attitude of people towards non-family members who have been infected with HIV/ AIDS is generally high in Northcentral Nigeria. However, more enlightment is needed for improvement.
Conclusion
The study has indicated that the attitude of people to family members and non-family members infected with HIV/AIDS is positively high among people of Northcentral Nigeria. Virtually all the variables used in the analysis were significantly associated with positive attitudes to people living with HIV/AIDS as shown in the tables and figures. Most people are ready and willing to associate with people infected by HIV/AIDS, however much more enlightment is still needed for improvement.
Recommendation
The analysis has shown that the attitude to people living with HIV/ AIDS in Northcentral Nigeria is positively high, but much more need to be done to end HIV stigma and discrimination. These can include the use of specific programmes that emphasize the rights of people living with HIV, well-documented way of eradicating stigma, as well as being made aware of their rights. People living with HIV can be empowered in order to take action if these rights are violated. Ultimately, adopting a human rights approach to HIV and AIDS is in the public’s interest. Stigma blocks access to HIV testing and treatment services, making onwards transmission more likely. The removal of barriers to these services is key to ending the global HIV epidemic.
In March 2016, UNAIDS and WHO’s Global Health Workforce Alliance launched the Agenda for Zero Discrimination in Healthcare. This works towards a world where everyone, everywhere, is able to receive the healthcare they need with no discrimination, in line with The UN Political Declaration on Ending AIDS. Zero discrimination is also at the heart of the UNAIDS vision, and one of the targets of its Fast-Track response. This focuses on addressing discrimination in healthcare, workplace and education settings.
References
- UNAIDS. On the Fast-Track to end AIDS by 2030: Focus on location and population. UNAIDS. 2015.
- UNAIDS. Agenda for zero discrimination in health-care settings. UNAIDS. 2017.
- Anne L Stangl, Jennifer K Lloyd, Laura M Brady, et al. A systematic review of interventions to reduce HIV-related stigma and discrimination from 2002 to 2013: how far have we come? JIAS. 2013; 16: 18734.
- Huffington Post. Giving Power to Couples to End the AIDS Epidemic. 2012.
- UNAIDS. Feature story: Ghana-addressing the barrier of stigma and discrimination for women. 2017.
- UNAIDS. Feature story: HIV prevention among key populations. 2016.
- World Health Organization. Global HIV/AIDS Response: Epidemic update and health sector progress towards Universal Access: Progress report 2011 and UNAIDS. 2011. Guidance note: Reduction of HIV-related stigma and discrimination.
- World Health Organization. Guideline on when to start antiretroviral therapy and on pre-exposure prophylaxis for HIV. 2015.
- The Well Project. Stigma and Discrimination Against Women Living with HIV. 2016.
- PLHIV Stigma Index. We are the change: Dealing with self- stigma and HIV/AIDS: An experience from Zimbabwe. 2015.