Assessment of Suboptimal Bowel Preparation is Highly Variable among Physicians in The Same Practice and Not Associated with Their Adenoma Detection Rates
Author'(s): Susan Lou, MD1,2, Allison Levy, MD1, Aasma Shaukat, MD, MPH2, Michael Kuskowski, PhD2, Shahnaz Sultan, MD, MHSc2, Michael Levitt, MD2, and Ashish Malhotra, MS, MD2
1University of Minnesota, Minneapolis, MN, USA.
2Minneapolis Veterans Affairs Medical Center, Minneapolis, MN, USA.
*Correspondence:
Susan Lou, MD, CHQ, One Veterans Drive, 111-D, Tel: 6124674100; Fax Number: 6127252248.
Received: 15 July 2020 Accepted: 02 August 2020
Citation: Lou S, Levy A, Shaukat A, et al. Assessment of Suboptimal Bowel Preparation is Highly Variable among Physicians in The Same Practice and Not Associated with Their Adenoma Detection Rates. Gastroint Hepatol Dig Dis. 2020; 3(2): 1-5.
Abstract
Introduction: Suboptimal colonic preparation adversely impacts the adenoma detection rate (ADR) and increases healthcare costs. Though a low threshold for categorizing the preparation as inadequate increases repeat colonoscopies, such fastidiousness could result in a higher quality colonoscopy. Our objectives were: 1) To examine the variability among colonoscopists in their bowel prep ratings and 2) To assess the correlation between suboptimal prep rate (SPR) and ADR.
Methods: We conducted a retrospective analysis of all outpatient colonoscopies performed from 2013-2015 at the Minneapolis Veterans Affairs Medical Center. Data were coded by indication for colonoscopy and bowel prep grading (Aronchick Scale). Suboptimal bowel prep was defined as the sum of fair and poor prep grades. Suboptimal prep rates (SPR) per year were calculated for each endoscopist. A random sample of 50 screening colonoscopies/year with adequate prep was used to calculate each endoscopist’s ADR
Results: There were 7125 colonoscopies performed by 10 endoscopists during the study period. Results showed large variability of SPR amongst endoscopists, ranging from 5% to 38% (p<0.001, chi-square). Logistic mixed model regression revealed that SPR (for each provider) was not a significant predictor of adenoma detection (OR=1.012 [95% CI: 0. 99-1. 03]; p=0.29).
Discussion: The study demonstrates consistent major differences between individual endoscopists regarding the frequency of grading colonic preps as suboptimal. Based on ADR, strict interpretation of the adequacy of the prep did not translate into a more effective colonoscopy. Thus, training about what constitutes an adequate prep could reduce unnecessary repeat colonoscopies.
Keywords
Introduction
Colonoscopy is the preferred method for detection and prevention of colorectal carcinoma [1]. While the ultimate indicator of an effective colonoscopy is the absence of interval cancers, this outcome is rare and takes years to manifest. Thus, the adenoma detection rate (ADR), as defined by the proportion of colonoscopies with at least one adenoma detected, has become widely employed as the primary quality indicator for colonoscopy [2]. ADR is associated with clinical outcomes with lower ADR correlated with higher interval cancer rates [1-4].
There are multiple factors that influence the ADR, including both endoscopist and patient characteristics [5]. A wide variability remains in the ADR of the individual endoscopist after adjusting for patient variables [6], and the individual endoscopist remains an important predictor of ADR [7]. Furthermore, even after adjusting for variables such as endoscopist area of specialty, level of experience, withdrawal technique, there remains variability of ADR suggesting that other factors are at play [2,5,8].
A meta-analysis of five repeat-colonoscopy studies [9] showed that inadequate bowel cleansing lowered the diagnostic yield of colonoscopy, with adenoma miss rates ranging from 27-56% for colonoscopies with poor, fair, or suboptimal preparation respectively. Such studies highlight the fact that inadequate bowel preparation substantially lowers the adenoma detection, and the effectiveness of colonoscopy as a screening modality. Additionally, endoscopists have been noted to differ in their grading of bowel preparations, despite uniform instructions on the specific criteria for grading prep quality. It could be hypothesized that endoscopists who have a higher rate of grading bowel preparation as fair or poor, as defined by their suboptimal prep rate (SPR), may perform a more meticulous, clinically important endoscopy as reflected in ADR. However, studies assessing this relationship have yielded diverse results. Thomas-Gibson [10] found that endoscopists with a higher ADR were more likely to be critical of the quality of bowel preparation (and thus have a higher SPR) when performing screening flexible sigmoidoscopies. Similarly, Ezaz [11] found a significant relationship between ADR and personality traits, with higher ADR associated with endoscopists who were more meticulous (self-described as more compulsive or thorough as well as those who felt rushed with longer withdrawal times). This suggests that more fastidious endoscopists, defined as those with a higher level of meticulousness and attention to detail, correlate with higher ADR. However, Mahadev [12] found no correlation between an endoscopist’s ADR and SPR when performing screening colonoscopies. The aim of our study was to examine individual variability in bowel prep ratings and to assess the correlation between suboptimal prep rate (SPR) and ADR.
Methods
We performed a retrospective analysis of all outpatient screening colonoscopies (n=7,125) performed by a total of ten providers during the 3-year period of January 1, 2013 and December 31, 2015 at the Minneapolis Veterans Affairs (VA) Medical Center. Patients in our practice were randomly allocated to each provider, i.e., there were no systematic differences in the type of patient assigned to each endoscopist. Each endoscopist performed a minimum of 250 colonoscopies during the study period. All patients were given the same prep (split prep with 1 gallon of Golytely plus 1 bottle of magnesium citrate if no underlying kidney disease) and the same prep instructions. Each endoscopist performed a minimum of 100 colonoscopies per year during the study period. From this database, patients were included if they were >=50 years old, the procedure was performed for screening, the quality of the bowel preparation was noted in the report, and the pathology report was available if tissue samples were obtained. Patients were excluded if they were of inpatient status or had an ileostomy or colostomy.
The Minneapolis VA endoscopy database was utilized to identify indications for colonoscopy, bowel prep rating, final reports, and the corresponding pathology.
Indications for colonoscopy were coded into one of five categories:
(1) Screening, (2) High risk screening, (3) Diagnostic, (4) IBD surveillance, (5) Therapeutic. Any colonoscopy that was not “true screening” was excluded, including those with family risk factors, inflammatory bowel disease, or symptoms requiring diagnosis. All patients received the same bowel prep instructions and regimen. Bowel prep was categorized into three general categories including "good/adequate", "fair", or "poor". Suboptimal bowel preps were defined as those rated as “fair,” “poor,” or “unsatisfactory.”
Suboptimal prep rates were calculated for each physician per year, as defined by the sum of the provider’s suboptimal rated colonoscopies (fair plus poor prep grades) divided by the provider’s total number of colonoscopies performed. Using a random sample of approximately 50 screening colonoscopies of at least adequate bowel prep rating, each provider’s ADRs were calculated. Additionally, secondary quality indicators were measured: 1) ADR-Plus Rate as defined by the number of adenomas detected beyond the first one detected per colonoscopy; 2) Adenomas per Colonoscopy (APC) as defined by total number of adenomas divided by total number of colonoscopies; 3) Adenomas per Positive Participant (APP) as defined by total adenomas divided by # of colonoscopies with at least one adenoma found.
Variability between providers in SPR (averaged across all three years) was assessed using a chi-square test. Year-to-year within- provider variability in SPR was assessed using a Cochran- Armitage chi-square test for trend. To examine the relationship between SPR and the presence/occurrence of adenoma, logistic mixed-effects regression models were estimated separately for adenoma, serrated adenoma, right-sided adenoma, and advanced adenoma. Since each provider contributed multiple observations of prep quality to the data analysis, mixed effects regression models were used to account for the effects of clustering of preps within provider when examining the relationship between SPR and ADR. Spearman correlation coefficients were calculated to examine the relationship between SPR and ADR across providers.
To examine the relationship between SPR and the detection of multiple adenomas per procedure (an outcome variable measured by the total number of adenomas detected in each procedure), a negative binomial mixed-effects regression model was estimated. To assess the relationship between SPR and detection of multiple adenomas in a procedure, Spearman correlation coefficients were also computed for SPR.
Results
There were 7125 coloscopies performed by 10 endoscopists during the three-year study period. Table 1 shows baseline characteristics of the patients and the endoscopists. The majority of patients were male (97%), and the mean age of patients was 62 years. The mean age of patients did not vary significantly between providers.
Among the ten providers, the mean procedure volume during the study period was 713 colonoscopies. The most commonly selected bowel preparation rating was adequate or better (the sum of adequate, good, and excellent preparation ratings). The detection of multiple specific subtype adenomas in a single procedure was rare in this sample and therefore did not permit statistical modeling of adenoma subtypes.
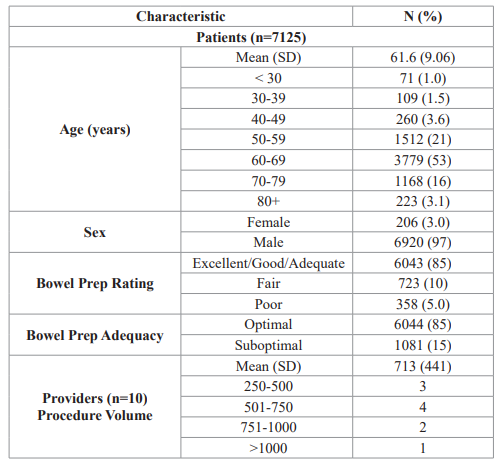
Table 1: Patient and Provider Characteristics.

Figure 1: Suboptimal Prep Rate for Each Physician Per Year.
Figure 1 shows that variability of SPR per year amongst the endoscopists ranged from 5% to 38% (p<0. 001, chi-square). These differences tended to be consistent over 3 years. Year-to-year variability in SPR within providers was statistically significant for four of the ten providers (p<0.05, chi-square).
Each colored line in this graph represents a gastroenterologist. The Y-axis is the rate of suboptimal prep and the X-axis is the year. The graph demonstrates differences between physicians’ grading of bowel prep ranging from the highest suboptimal prep rate of 38% to the lowest of 5% over these 3 years. It also shows that physicians are consistent for the most part from year to year. Physicians are randomly assigned to endoscopy shifts and cannot choose patients.
Table 2 shows the SPR by provider. As compared with Provider 8 (who had the lowest SPR at 5.44%), all providers, with the exception of physicians 0 and 40, had significantly increased odds of reporting a suboptimal prep quality. There was substantial variability in frequency of providers’ suboptimal prep quality rates with odds ratios ranging from 1.18 to 9.90 (as compared with Provider 8).
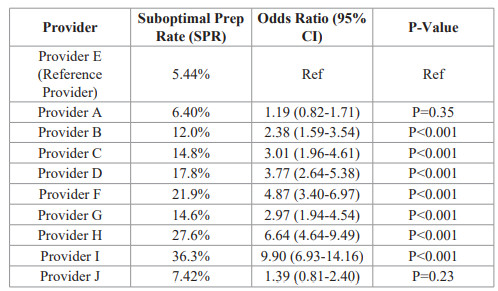
Table 2: Variability of Suboptimal Prep Rates by Providers.
This table demonstrates that nearly every provider had significantly increased odds of suboptimal prep quality as compared to the reference Provider 8 (who had the lowest SPR at 5.44%). Providers 0 and 40 did not significantly differ from Provider 8. There is a lot of variability in providers’ suboptimal prep quality rates with odds ratios ranging from 1.18 to 9.90 (versus Provider 8).
Table 3 demonstrates that there were significantly higher odds of suboptimal prep quality when the indication for colonoscopy was surveillance as compared to screening.
We also found a wide individual variation in ADR, ranging from 21.0% to 47.1%. A Spearman correlation analysis was performed, which demonstrated no significant correlation between SPR and ADR (r=0.31, p=0.38). SPR was not associated with APC (Adenomas Per Colonoscopy) or Adenoma per Positive Participant. SPR versus APC (all years combined) rho=0.15, df=8, p=0.68. SPR versus APP (all years combined) rho=0.25, df=8, p=0.51.
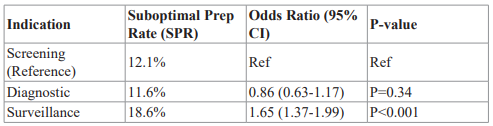
Table 3: Variability of Suboptimal Prep Rates by Indication for Colonoscopy.
This table demonstrates that there are significantly higher odds of suboptimal prep quality when the indication is for surveillance as compared to screening.
Discussion
Thus, after identifying the first polyp, endoscopists might give less attention to inspection of the remainder of the colon [15]. Multiple groups have studied the implementation of measures other than the ADR to distinguish between the effectiveness of endoscopists [9,16]. These measures include: 1) ADR-Plus Rate as defined by the number of adenomas detected beyond the first one detected per colonoscopy; 2) Adenomas per Colonoscopy (APC) as defined by total number of adenomas divided by total number of colonoscopies; and 3) Adenomas per Positive Participant (APP) as defined by total adenomas divided by # of colonoscopies with at least one adenoma found. In our study, we were unable to demonstrate a significant correlation between the SPR and any of the above metrics.
Since we could find no consistent differences between types of patients or patients’ prep to explain the differences in bowel prep ratings among the various experienced gastroenterologists, it is unlikely that differences in SPR were driven by differences in patient characteristics. Rather, it appears that an endoscopist’s risk aversive behavior may play a major role in the grading of bowel preparation since patients with suboptimal bowel prep require repeat endoscopy within one year.
The current study examined the variability of bowel prep grading among endoscopists and assessed its correlation with adenoma detection during colonoscopy. Several key findings deserve emphasis. First, despite similar patients, prep type and prep instructions, there was relatively enormous inter-physician variability in the frequency with which the colonic preparation was deemed to be suboptimal. As shown in Figure 1 and Table 4, over the three years of the study, the percentage of preps perceived to be suboptimal ranged from a low of 5.4% for one of the 10 endoscopists to a high of 36.3% for the most fastidious endoscopist. These differences remained consistent over a 3-year study period. Second, individual endoscopist’ SPR remained relatively constant over the 3-year study period indicating minimal intra-physician variability. Lastly, SPR did not correlate with any adenoma detection indicator (ADR, APC or APP).
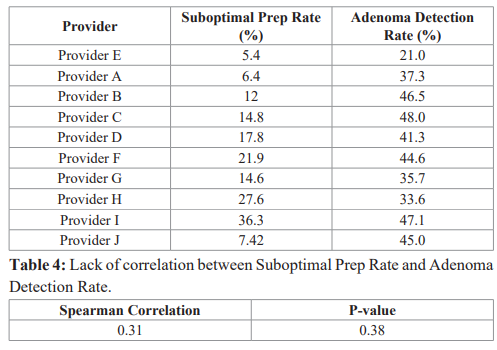
A Spearman correlation analysis was performed, which demonstrates that there was no significant correlation between suboptimal prep rate and adenoma detection rate.
Many endoscopists with high ADRs (>40%) have relatively high adenoma miss rates (AMR) ranging from 21-24% as demonstrated by studies utilizing back-to-back colonoscopies [13,14]. A possible explanation for this phenomenon is that the ADR quality metric rewards the “one and done” strategy of colonoscopy, giving the same credit for one versus more than one adenoma found.
Few prior studies have highlighted significant physician variability in prep grading. It remains to be determined if such variability emanates from differences in physician personality traits, education, experience or technique. For example, a more obsessive-compulsive endoscopist may be less likely to accept suboptimal views due to factors such as bowel spasm, inadequate insufflation, or depth of insertion. On the other hand, a less critical physician may be reluctant to call bowel prep “suboptimal” if it means that patient’s exam would need to be repeated at a shorter interval. Furthermore, the study highlights that the training for colonoscopy should not only emphasize hand-skills technique, but also should focus on the judgment processes and attitudes of endoscopists, which are a quintessential part of any clinical skill.
A fastidious colonic cleansing requirement is a very expensive practice in that a suboptimal prep report requires a repeat colonoscopy. In a review of ten randomly selected colonoscopy reports from the endoscopist with the highest SPR, ten out of the ten reports requested a repeat colonoscopy at a shorter time interval ranging from “next available” to six months. At the extremes in our study, an endoscopist rating 36% of colonoscopies preps inadequate versus one with 6% rating necessitates the performance of 30% more colonoscopies. Hypothetically extrapolated to the 17 million colonoscopies performed in the U.S. each year (https// ncbi.nim.nih.gov) at an average cost of $1,500 per colonoscopy, 30% additional colonoscopies entails an expenditure of roughly 8 billion dollars. In addition, about 5 million patients would be subjected to the potential complications, expenditure of time, and discomfort of a second colonoscopy.
Thus, it is apparent that meticulous grading of the colon prep should be avoided unless it can be demonstrated that such an appraisal leads to a more effective colonoscopy, i.e., fewer missed clinically significant lesions that subsequently present as interval cancers
The most widely accepted surrogate indicator of a well-performed colonoscopy is the ADR and, in our study, there was no significant correlation between a colonoscopist’s SPR and ADR, a result consistent with the study of Mahadev et. al, which also utilized a retrospective, single center design analyzing bowel prep rating and ADR from screening colonoscopies.
In conclusion, we found that there were wide differences in provider SPR, as well as a wide variation in ADR. Our analysis did not show that the SPR and ADR correlate. Given these data, it would seem that a stricter interpretation of the adequacy of the prep does not necessarily translate into a more effective colonoscopy. However, limitations of our study are that it is single center, retrospective, and was performed using the Aronchik score versus the Boston bowel prep score. In addition, a relatively small number of screening colonoscopies was used to calculate adenoma detection quality metrics. Further study is needed to assess the correlation between SPR and adenoma detection. To the extent that scrupulous attention to prep quality does not improve the effectiveness of the colonoscopy, training directed to what constitutes an adequate prep would reduce unnecessary repeat colonoscopies – an outcome that would be of benefit to both the individual patient and the finances of the health care system.
References
- Rex DK, Johnson David A, Anderson Joseph C, et American College of Gastroenterology guidelines for colorectal cancer screening 2009. Am J Gastroenterol. 2009; 104: 739-750.
- Rex DK, Schoenfeld Philip S, Cohen Jonathan, et al. Quality indicators for Gastrointestinal Endoscopy. 2015; 81: 31-53.
- Fayad NF, Kahi Colonoscopy quality assessment. Gastrointest Endosc Clin N Am. 2015; 25: 373-386.
- Corley DA, Jean-Jacques Gonvers, Jean-Jacques Gonvers. Adenoma detection rate and risk of colorectal cancer and N Engl J Med. 2014; 370: 1298-1306.
- Malhotra A, Shaukat A, What is the criterion for high- performing colonoscopists? Being meticulous! Gastrointest 2015; 82: 130-132.
- Tariq H, Muhammad Umar Kamal, Binita Sapkota, et al. Evaluation of the combined effect of factors influencing bowel preparation and adenoma detection rates in patients undergoing colonoscopy. BMJ open gastroenterology. 2019; 6: e000254-e000254.
- Chen SC, Rex DK. Endoscopist can be more powerful than age and male gender in predicting adenoma detection at Am J Gastroenterol. 2007; 102: 856-861.
- Adler A, Karl Wegscheider, David Lieberman, et al. Factors determining the quality of screening A prospective study on adenoma detection rates, from 12,134 examinations (Berlin colonoscopy project 3, BECOP-3). Gut. 2013; 62: 236-241.
- Sulz MC, Arne Kröger, Meher Prakash, et Meta-Analysis of the Effect of Bowel Preparation on Adenoma Detection: Early Adenomas Affected Stronger than Advanced Adenomas. PloS one. 2016; 11: e0154149-e0154149.
- Thomas-Gibson S, Rogers A, Cooper S, et Judgement of the quality of bowel preparation at screening flexible sigmoidoscopy is associated with variability in adenoma detection rates. Endoscopy. 2006; 38: 456-460.
- Ezaz G, Leffler DA, Beach S, et Association Between Endoscopist Personality and Rate of Adenoma Detection. Clinical Gastroenterology and Hepatology. 2019; 17: 1571-1579.
- Mahadev S, Green PH, Lebwohl Rates of Suboptimal Preparation for Colonoscopy Differ Markedly Between Providers: Impact on Adenoma Detection Rates. J Clin Gastroenterol. 2015. 49: 746-750.
- Heresbach D, Barrioz T, Lapalus MG, et al. Miss rate for colorectal neoplastic polyps: a prospective multicenter study of back-to-back video colonoscopies. Endoscopy. 2008; 40: 284-290.
- Munroe CA, Philip Lee, Andrew Copland, et al. A tandem colonoscopy study of adenoma miss rates during endoscopic training: a venture into uncharted territory. Gastrointestinal 2012; 75: 561-567.
- Wang HS, Joseph Pisegna, Rusha Modi, et Adenoma detection rate is necessary but insufficient for distinguishing high versus low endoscopist performance. Gastrointestinal Endoscopy. 2013; 77: 71-78.
- Froehlich F, Vincent Wietlisbach, Jean-Jacques Gonvers, et al. Impact of colonic cleansing on quality and diagnostic yield of colonoscopy: the European Panel of Appropriateness of Gastrointestinal Endoscopy European multicenter study. Gastrointestinal 2005. 61: 378-384.