Cardiovascular Risk, Statin Use and Electrocardiogram in HIV Patients
Author(s): Roberto Ramos Barbosa1*, Ana Luísa Pimenta Suzano1, Beatriz Castro Torres1, Carolina Rios Andreão1,Lucas Crespo de Barros1, Rodolfo Costa Sylvestre1, Camila Magioni Figueira2, Ramona Dutra Uliana1,Carolina Rocio Oliveira Santos1 and Luiz Fernando Machado Barbosa1
1Escola Superior de Ciências da Santa Casa de Misericórdia de Vitória (EMESCAM), Brazil.
2Centro Universitário Multivix.
*Correspondence:
Roberto Ramos Barbosa, Av. N. S. da Penha, 2190, Santa Luiza, CEP 29045-402, Vitória, ES, Cardiology Department, Tel: +55(27) 99961-4907.
Received: 15 Apr 2024; Accepted: 20 May 2024; Published: 29 May 2024
Citation: Barbosa BR, Suzano ALP, Torres BC. Cardiovascular Risk, Statin Use and Electrocardiogram in HIV Patients. Cardiol Vasc Res. 2024; 8(1): 1-5.
Abstract
Introduction: Non-infectious complications became more frequent in patients living with the Human Immunodeficiency Virus (HIV). Dyslipidemia is common and represents an important cardiovascular risk factor in this population. Therefore, cardiovascular diseases represent one of the main causes of HIV morbidity and mortality.
Objective: This study aimed to assess cardiovascular risk and electrocardiographic changes in outpatients living with HIV.
Methods: We performed a single-center cross-sectional study that included HIV patients who were at least 30 years old and had HIV diagnosis for more than one year. Patients were on regular follow-up in a tertiary center in Brazil. Cardiovascular risk was assessed using the Global Risk Score (GRS), as recommended by Brazilian guidelines. Cardiovascular risk factors, lipid profile, statin use and resting electrocardiogram were also analyzed.
Results: 92 patients were included, with an average age of 48.9 years. 54 (58.7%) were male, 28 (30.4%) had hypertension, 10 (10.9%) had type 2 diabetes mellitus, 9 (9.8%) were current smokers, and 25 (27.2%) had a previous diagnosis of dyslipidemia. Average LDL-cholesterol level was 120.2 ± 40.6 mg/dl. Eleven patients (11.9%) were on statin therapy. High cardiovascular risk was identified in 28 patients (30.4%) and only seven of those (25.0%) were on statin therapy. Serum LDL-cholesterol higher than or equal to 130 mg/dl was found in 31 patients (33.7%), and only seven of those (22.6%) were on statin therapy. ECG changes were found in 21.7%, mostly due to conduction disturbances (17.4%).
Conclusion: We found a high prevalence of HIV outpatients with high cardiovascular risk. Only one in every four patients with this characteristic was on statin therapy. Cardiovascular risk is one of the main concerns in the HIV population, once antiretroviral therapy succeeds to reduce mortality attributed to opportunistic infections.
Keywords
Introduction
Approximately 920,000 people live with the human immunodeficiency virus (HIV) in Brazil. Of these, 77% are on antiretroviral therapy (ART), and 94% of patients on treatment do not transmit HIV sexually as they have reached an undetectable viral load [1]. ART is considered a cornerstone intervention to control HIV transmission. The introduction of ART determined an important advance in the effective control of infection, restoration of immunity and reduction of HIV-related morbidity and mortality [2,3]. As a consequence, HIV infection is now considered a chronic disease.
Non-infectious complications became more frequent and are relevant for debating [2]. The benefits of ART, especially protease inhibitors, are accompanied by metabolic disorders as side effects. The most frequent is dyslipidemia, with an increase of cholesterol, triglycerides and low-density lipoprotein (LDL), but reduction of high-density lipoprotein (HDL) levels [4]. Hypercholesterolemia that is secondary to treatment with protease inhibitors may vary from 33 to 82%, while 43 to 66% of this population has secondary hypertriglyceridemia [5].
In such a context, cardiovascular diseases represent one of the main causes of HIV morbidity and mortality. HIV-infected patients have higher risk of myocardial infarction and sudden death than the general population. Besides, people with HIV infection have cardiovascular events approximately 10 years before the general population [6]. The electrocardiogram (ECG) is a widely available, low-cost, non-invasive test that can be used to detect manifestations of cardiovascular disease. Therefore, resting electrocardiographic changes may represent a warning for increased cardiovascular risk in special populations [7].
It is paramount to assess and reduce cardiovascular risk in HIV patients. Knowing the local data is important to create focused protocols and improve efforts on reducing modifiable risk factors [8]. Thus, the objective of this study is to evaluate the lipid levels in HIV-infected patients, their cardiovascular risk stratification, prevalence of statin use, and resting ECG changes.
Methods
Study Design
This is a cross-sectional observational study with quantitative analysis, based on data collected from medical records of the Infectious Diseases outpatient clinic in a tertiary center in Brazil, between September 2021 and January 2022.
Population
Patients were consecutively included if they were at least 30 years of age and had HIV infection diagnosed for more than one year. In these patients, a resting electrocardiogram was performed on the day of their inclusion in the study and the lipidogram was collected, or the most recent one was recorded, if it had been performed within the past six months. Patients who were not currently on ART, either by medical advice or by their own decision, were excluded. We also excluded patients with a past history of any atherosclerotic disease (stroke, coronary artery disease, myocardial infarction, carotid stenosis or peripheral artery disease).
Variables Analyzed
The clinical variables collected from the electronic medical records were: gender, age, previous cardiac diagnosis, duration of diagnosis of HIV infection, presence of arterial hypertension, diabetes, dyslipidemia, current smoking, use of statins and fibrates, and lipid profile (total cholesterol, triglycerides, HDL- cholesterol, LDL-cholesterol). Cardiovascular risk was calculated using the Global Risk Score (GRS) directly on the website of the calculator for risk stratification of the Brazilian Society of Cardiology (http://departamentos.cardiol.br/sbc-da/2015/ CALCULADORAER2017/index.html).
Current statin therapy was assessed according to cardiovascular risk groups. Besides, the group of patients with serum LDL- cholesterol higher than or equal to 130 mg/dl was analyzed for current statin use, independently of cardiovascular risk group.
ECGs were analyzed by two experienced cardiologists (LFMB and RRB). Only printed ECGs were considered for analysis, and no electronic tools were used for this purpose. The following electrocardiographic data were analyzed on the resting ECG of included patients: PR interval, QRS duration, QT interval, QT corrected interval (QTc) by Bazett's formula, conduction disturbances (bundle branch blocks or hemiblocks), rhythm disturbances (arrhythmias other than premature complexes), alterations suggestive of myocardial ischemia (ST segment and T wave alterations) and signs of left ventricular hypertrophy (compatible height and pattern of QRS complexes). The numeric results found for each variable were summed and the average between experts was adopted for all ECG variables; disturbances found as “present or absent” had to be confirmed by both experts. Prolonged QTc interval was considered as a QTc interval greater than 450 ms for male and greater than 470 ms for female subjects.
Statistical Analysis
Comparisons were made between male and female group for the presence of cardiovascular risk factors. ECG analyses were also compared between these groups.
The Pearson Chi-Square test, Fisher test and t-student test were used for comparisons. The analyses were performed using Statistical Package for the Social Sciences (SPSS) software, version 23.0. P-values < 0.05 were considered as statistically significant.
Ethical Aspects
The study complied with the ethical precepts of the Declaration of Helsinki, as recommended by the National Health Council resolution 466/2012 of the Ministry of Health of Brazil. All participants understood and signed the Free and Informed Consent Term before inclusion in the study. The study was approved by the Research Ethics Committee of the institution, CAAE number 01964918.6.0000.5065.
Results
A total of 105 outpatients were screened; 98 patients were on ART and were included in the study. Six patients were excluded - four did not accept to do an ECG at the time of inclusion, and two had a previous history of atherosclerotic disease (one stroke and one coronary artery disease). Thus, the study sample consisted of 92 patients, with an average age of 48.9 ± 11.8 years, of whom 54 (58.7%) were male. Hypertension was found in 28 patients (30.4%), dyslipidemia in 25 (27.2%), diabetes mellitus in 10 (10.8%), and current smoking in 9 (9.8%). The prevalence of cardiovascular risk factors according to gender is shown in table 1. Of this sample, 17 patients (18.5%) were aged less than 40 years. One patient (1.9%) had a past history of atrial flutter. The average time of diagnosis of HIV-infection was 13.6 ± 6.7 years.

The average total cholesterol value was 189.9 ± 43.3 mg/dL, HDL-cholesterol 46.7 ± 12.3 mg/dL, LDL-cholesterol 120.2 ± 40.6 mg/dL and triglycerides 142.1 ± 84.2 mg/dL. Cardiovascular risk classification was performed in 90 patients (97.8%), since two patients had no laboratory tests for lipid levels. Twenty-eight patients (31.1%) were classified as having high cardiovascular risk, 31 (34.4%) as intermediate cardiovascular risk and 31 (34.4%) as low cardiovascular risk.
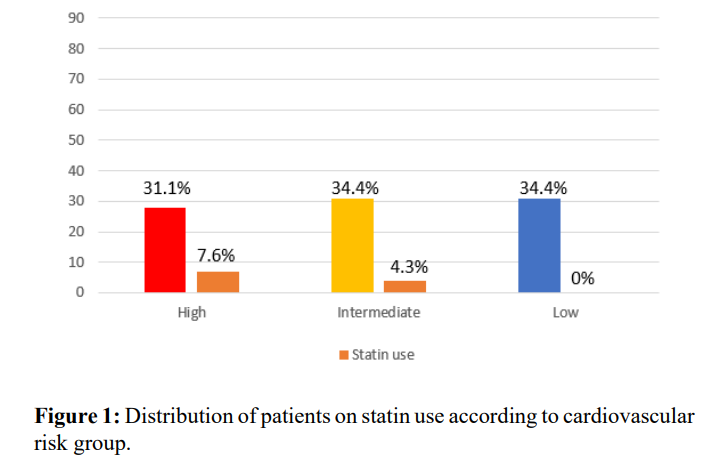
Eleven patients (11.9%) were on current statin therapy. Seven of those had high cardiovascular risk and four had intermediate cardiovascular risk. Distribution of statin use according to cardiovascular risk groups is represented in Figure 1. Amongst the 31 patients (33.6%) who had LDL-cholesterol higher than or equal to 130 mg/dL, only seven (22.5% of those) were using statins. Nine patients in the total sample (9.8%) were currently taking fibrates.
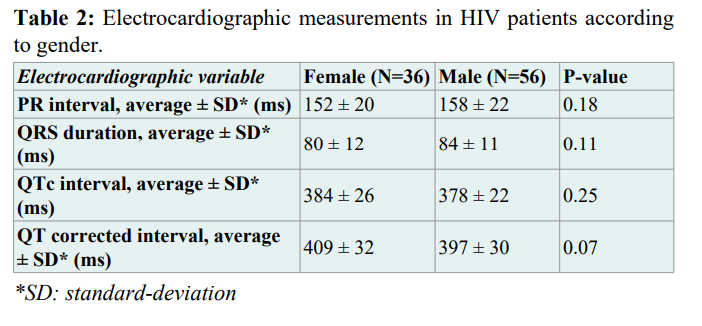
The analysis of the ECGs showed an average PR interval of 156 ± 18 ms, QRS duration of 83 ± 12 ms, QT interval of 380 ± 24 ms and QTc interval of 401 ± 30 ms. There were no significant differences between male and female patients regarding these electrocardiographic measurements, as shown in Table 2. One patient (1.1%) had prolonged QTc interval (this subject was a male). One patient (1.1%) had heart rhythm disturbance (atrial fibrillation), 16 patients (17.4%) had conduction disturbances, and two patients (2.2%) had resting ECG alterations suggestive of myocardial ischemia. None had ECG findings of left ventricular hypertrophy.
Discussion
In this observational single-center study, we identified a large group of outpatients with HIV infection classified as high cardiovascular risk. This result is similar to that found in a cohort of hospitalized patients in Brazil [9]. However, that study used a different risk score. The GRS is used to assess the risk of myocardial infarction, stroke, peripheral vascular insufficiency and heart failure in 10 years, and is validated for the Brazilian population [10]. Interventions and preventive actions, such as statin therapy, initially rely upon conventional risk stratification. Different scores may vary considerably for cardiovascular risk assessment and confound therapeutic strategies, especially in unusual populations.
Other than the traditional cardiovascular risk factors, obesity, alcohol consumption, stress, depression, low vegetable and fruit intake and physical inactivity are suggested as relevant for the proper calculation of cardiovascular risk. Inflammatory markers, such as C-reactive protein and homocysteine, may also play a role on the incidence of cardiovascular events and prediction of risk [11]. These findings strongly motivate studies in special populations, in whom traditional risk calculators may underestimate cardiovascular risk. HIV-infected patients represent one of these groups, as well as patients with chronic inflammatory diseases.
Cardiovascular prevention in HIV-infected people is mainly based on the same recommendations for those not infected by the virus. However, cardiovascular risk calculation may underestimate their risk, because of the association between ART and atherosclerosis [12]. Our poor results on statin use in HIV-infected outpatients show that cardiovascular risk equations derived from an HIV population could be useful and provide early and appropriate guidance [13]. Moreover, medical staff should offer special attention to the cardiovascular health status of such patients.
It is known that HIV-patients must undergo screening for dyslipidemia due to the interaction of this condition with HIV infection and the use of ART. Reducing LDL-cholesterol levels with lipid-lowering therapy for patients with HIV can reduce cardiovascular risk by approximately 20 to 30% [14]. In our study, a significant number of patients with severe dyslipidemia and with high cardiovascular risk were not using statins. The lack of blood lipid control, along with the presence of other risk factors, results in increased predisposition for the development of cardiovascular disease [15]. This has been one of the greatest challenges in medical care for HIV-infected patients.
The resting ECG may vary significantly in HIV patients due to a number of reasons. In this cohort, we showed no differences between male and female subjects concerning PR interval, QRS duration and QT interval. Overall ECG analyses showed normal findings in most patients. Most abnormalities derived from conduction disturbances. ART itself is not directly associated with electrocardiographic changes, although these patients commonly use other medications that are capable of it. Finally, our ECG findings were very similar to that described for other populations, including non-HIV patients [16].
Despite its relevance, this study has limitations, since the analysis was based on patients from one tertiary hospital, which may not be the reality of several Brazilian centers. The ECGs were analyzed without electronic tools. These could be able to minimize measurement errors. Furthermore, assessing prospective data on the evolution of these patients, although important, was not the aim of this study. Despite this, the high prevalence of patients with high and intermediate cardiovascular risk is in accordance with other studies on the same topic. This raises awareness for the risk of future cardiovascular events and the capacity of the public health system in developing countries to properly treat this population.
Conclusion
Almost one third of outpatients living with HIV infection presented high cardiovascular risk, and less than one fourth of those were on current statin therapy. ECG alterations were uncommon and did not differ between female and male groups. These data are important since cardiovascular diseases are one of the leading causes of death in this population, requiring specific actions to prevent adverse cardiac events.
Authors contribution
Study conception and design: Roberto Ramos Barbosa, Luiz Fernando Machado Barbosa.
Data collection: Ana Luísa Pimenta Suzano, Beatriz Castro Torres,
Carolina Rios Andreão, Carolina Rocio Oliveira Santos. Statistical analysis: Roberto Ramos Barbosa, Lucas Crespo de Barros, Rodolfo Costa Sylvestre.
Manuscript writing: Roberto Ramos Barbosa, Ana Luísa Pimenta Suzano, Beatriz Castro Torres, Carolina Rios Andreão, Camila Magioni Figueira.
Major revision: Lucas Crespo de Barros, Rodolfo Costa Sylvestre, Roberto Ramos Barbosa, Luiz Fernando Machado Barbosa.
References
- Brazilian Ministry of Health. [Protocolo clínico e diretrizes terapêuticas para a atenção integral às pessoas com infecções sexualmente transmissíveis (IST)] [Article in Portuguese]. Brasília. Secretaria de Vigilância em Saúde, Departamento de Doenças de Condições Crônicas e Infecções Sexualmente Transmissíveis. 2022.
- Aberg JA. Cardiovascular complications in HIV management: past, present, and future. J Acquir Immune Defic Syndr. 2009; 50: 54-64.
- Chan D, Gracey D, Bailey M, et al. Screening and management of cardiovascular disease in Australian adults with HIV infection. Sex Health. 2013; 10: 495-501.
- Grand M, Bia D, Diaz A. Cardiovascular Risk Assessment in People Living With HIV: A Systematic Review and Meta- Analysis of Real-Life Data. Curr HIV Res. 2020; 18: 5-18.
- Yu PC, Calderaro D, Lima EM, et al. Hypolipidemic therapy under special conditions: acquired immune deficiency syndrome. Arq Bras Cardiol. 2005; 85: 58-61.
- Feinstein MJ, Hsue PY, Benjamin LA, et al. Characteristics, Prevention, and Management of Cardiovascular Disease in People Living With HIV: A Scientific Statement From the American Heart Association. Circulation. 2019; 140: e98-e124.
- Cardoso E, Martins IS, Fornari L, et al. Electrocardiographic abnormalities and cardiovascular risk factors for ischemic heart disease in an adult population from São Paulo, Brazil. Rev Assoc Medica Bras. Set 2002; 48: 231-236.
- Fragkou PC, Moschopoulos CD, Dimopoulou D, et al. Cardiovascular disease and risk assessment in people living with HIV: Current practices and novel perspectives. Hellenic J Cardiol. 2023; 71: 42-54.
- Azevedo TD, Moreira ML, Nucera AP. Cardiovascular Risk Estimation by the ASCVD Risk Estimator Application in a University Hospital. Int J Cardiovasc Sci. 2018; 31: 492-498.
- Sofogianni A, Stalikas N, Antza C, et al. Cardiovascular Risk Prediction Models and Scores in the Era of Personalized Medicine. J Pers Med. 2022; 12: 1180.
- Triant VA, Perez J, Regan S, et al. Cardiovascular Risk Prediction Functions Underestimate Risk in HIV Infection. Circulation. 2018; 137: 2203-2214.
- Friis-Møller N, Thiébaut R, Reiss P, et al. Predicting the risk of cardiovascular disease in HIV-infected patients: the data collection on adverse effects of anti-HIV drugs study. Eur J Cardiovasc Prev Rehabil. 2010; 17: 491-501.
- Thompson MA, Horberg MA, Agwu AL, et al. Primary Care Guidance for Persons With Human Immunodeficiency Virus: 2020 Update by the HIV Medicine Association of the Infectious Diseases Society of America. Clin Infect Dis. 2021; 73: e3572-e3605.
- Pawlos A, Broncel M, Jablonowska E, et al. Cardiovascular risk and response to lipid lowering therapy in patients with HIV infection according to different recommendations. PLoS One. 2020; 15: e0244675.
- Liang Y, Ketchum NS, Turner BJ, et al. Cardiovascular Risk Assessment Varies Widely by Calculator and Race/Ethnicity in a Majority Latinx Cohort Living with HIV. J Immigr Minor Health. 2020; 22: 323-335.
- Sebold FGJ, Schuelter-Trevisol F, Nakashima L, et al. Electrocardiographic changes in adults living in a southern Brazilian city: A population-based study. Rev Port Cardiol. 2015; 34: 745-751.