Catheter Directed Thrombolytic Therapy for Massive Pulmonary Embolism in Nigeria: Case Report
Author(s): Edafe EA1,2*, MBBS, FMCP, FWACP, and Odia OJ2, MBBS, FMCP, FWACP, FRCP
1Bayelsa Specialist Hospital, Yenagoa, Nigeria.
2University of Port Harcourt Teaching Hospital, Port Harcourt, Nigeria.
*Correspondence:
Edafe EA, Bayelsa Specialist Hospital, Yenagoa, Nigeria, University of Port Harcourt Teaching Hospital, Port Harcourt, Nigeria.
Received: 08 August 2019; Accepted: 25 August 2019
Citation: Edafe EA, Odia OJ. Catheter Directed Thrombolytic Therapy for Massive Pulmonary Embolism in Nigeria: Case Report. Cardiol Vasc Res. 2019; 3(4); 1-4.
Abstract
Massive pulmonary embolism (PE) is not uncommon in Nigeria. The clinical syndrome may be followed with a subtle clinical signs and symptoms. In the case of massive PE the severity of the clinical presentation typically makes the picture more obvious. We the report a first case of catheter directed thrombolytic therapy (CDTT) with alteplase in Nigeria.
Keywords
Introduction
Acute pulmonary embolism (APE) is a sudden obstruction with clot in the main pulmonary artery or its branches. It is the third leading cause of cardiovascular mortality, accounting for 5% to 10% of in-hospital deaths in the Western world [1]. At least one quarter of patients at risk of venous thrombo-embolism in Africa are not receiving prophylaxis [2]. The prevalence of pulmonary embolism (PE) in medical patients varied between 0.14% and 61.5%, with a mortality rate of PE between 40% and 69.5% [2].
The case-fatality rate after surgery was 60% [2]. Management of APE is guided by the acuity and severity of clinical presentation. Systemic anticoagulation is the standard of care in acute massive PE, and treatment is escalated on the basis of the clinical presentation and characteristics of patients that may stratify them at high risk of mortality.
Massive PE definition is in association with sustained hemodynamic instability, whereas sub-massive PE is without hemodynamic instability but with abnormal right ventricular (RV) function or evidence of myocardial necrosis [4]. Treatment options include systemic thrombolysis, catheter-directed or surgical thromboembolectomy. The use of CDTT in the treatment of massive pulmonary has not been done in Nigeria. We report the first case of catheter directed thrombolytic therapy [CDTT] for the treatment of massive pulmonary embolism in Nigeria.
Case Presentation
A 47-year-old man living with hypertension, type 2 Diabetes Mellitus and dyslipidemia for the 6 years. He had deep vein thrombosis (DVT) in march 2014, DVT and APE in June 2016. He was treated medically and was on warfarin for 7 months. He stopped anticoagulation in January 2017. He presented to us with 1-week history of chest pain and dyspnea. Pain was sudden, in the anterior chest, lasting for about 25 minutes and is recurrent. Patient has pain more than 5 times a day. Pain is not positioned depended and non-radiating. There was associated intermittent dyspnea. No history of cough, no vomiting, no leg pain or swelling. Patient has a family history of DVT and pulmonary embolism. The immediate elder brother had DVT and PE in 2010. The younger sister had recurrent DVT in 2008, 2009 and 2014.
Examination at presentation showed middle aged man in respiratory distress (respiratory rate was 44cpm), not pale anicteric, no digital clubbing, no leg edema, oxygen saturation was 76%. His weight and height were 98kg and 171cm. The pulse rate was 104bpm, BP was 80/50 mmHg, JVP was elevated at 9cmh30, Heart sounds S1, S2, S3. Bibasal crepitation in the lower lung zones. The abdominal and the neurologic examination were

essentially normal. The investigations results were as follows: D-dimer=2450nmol/l, troponin I =2.4 ug/l [<0.35ug/l], Na =138mmol/l, K =4.2mmol/l, Cl=110mmol/l, Hb=13.8g/dl.
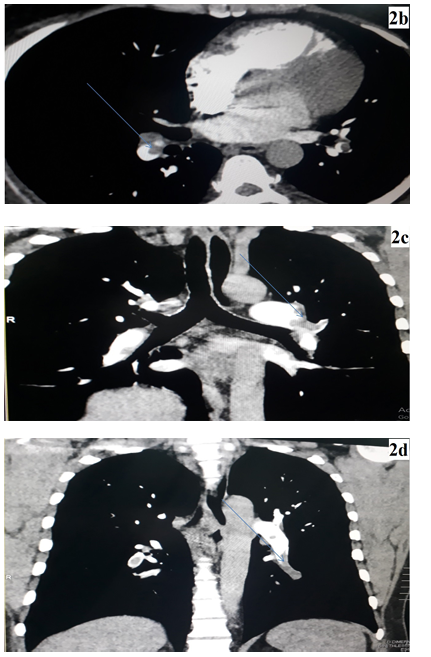
Figure 3 shows the CT angiographic report. a, b, and c and d showed the areas of filling defects in the pulmonary artery branches.
Procedure
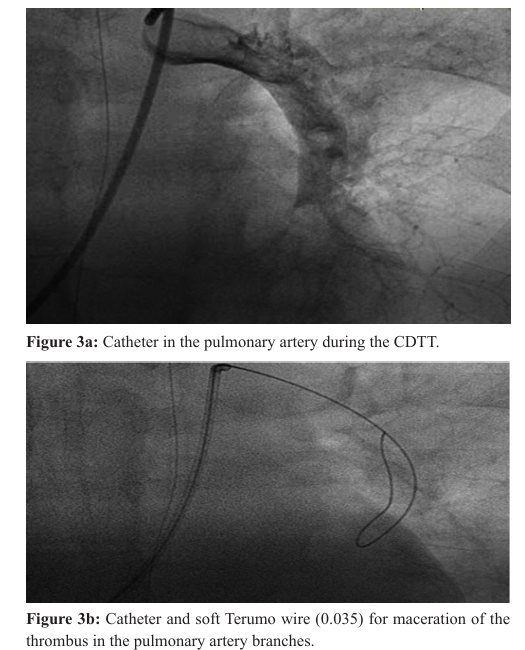
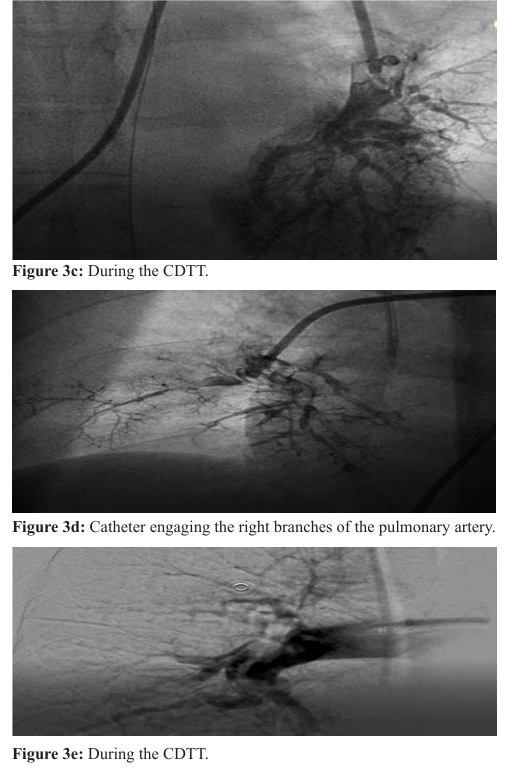
Informed consent was taken from patient and was taken to the cath lab. Access was through the right femoral vein with 8Fs health. Terumo (0.35) and 3.5 JR catheter were passed to the pulmonary artery. The main pulmonary BP was 78 mmHg and oxygen saturation was 76%. The catheter was directed to various left and right branches of the pulmonary artery with soft terumo macerating the clots. Alteplase was infused at various branches of the pulmonary artery branches up to 50mg over 40 minutes while the catheter and the terumo wire were being used to macerate the During the procedure, the saturation increased from 76% to 97% and the mean pulmonary artery pressure dropped to 48mmHg while on table. There was no complication. Patient was transferred to the intensive care unit. Subcut enoxaparin 80 mg (0.8ml) 12 hourly for 4 days and oral dabigantran 150 mg twice daily. The patient oxygen saturation on room air was between 94-97% on the first day post procedure and this improved to 98-100% on the 3day. He discharged home on the 4th day after oxygen saturation was persistent between 97-100% on room air at rest and after 6 minutes work. He continues his metformin, approval and dabigantran (150 mg twice daily). His follow up has been stable and adherence on his medication.
Discussion
Massive PE which is a life threatening condition and defined as PE in the presence of (a) Arterial hypotension (systolic blood pressure <90 mm Hg or a decrease of >40 mm Hg) for more than 15 minutes or requiring inotropic support, which is not caused by a new-onset arrhythmia (b) Cardiogenic shock (oliguria, lactic acidosis, cool extremities, or altered level of consciousness) (c) Circulatory collapse, in patients with syncope or undergoing cardiopulmonary resuscitation. This patient has hypoxia, chest pain, dyspnea and cardiogenic shock. Using the modified Geniva score, our patient has a score of 3 [previous DVT and a heart rate of 104bpm]. The primary cause of death in patients with massive PE is low cardiac output. Our patient was in cardiogenic shock.
Massive PE has higher mortality. Mortality from PE in patients with medical illnesses PE was associated with a mortality rate between 40% and 69.5% [3,4]. Bahloul et al. reported the highest mortality rate associated with PE; this was 69.5% in patients with acute exacerbation of COPD [4]. Amar et al. reported a mortality rate of 40% associated with PE in patients with tuberculosis [3].
Catheter-directed thrombectomy is a therapeutic strategy that can be used for the treatment of acute massive PE. It is usually performed in patients with acute massive PE, in whom thrombolysis is contraindicated or has failed, and in whom surgical intervention is not available or contraindicated [5]. In Nigeria, the treatment of acute pulmonary embolism has been use of enoxaparin, warfarin of new oral anticoagulants. Surgical intervention for massive pulmonary embolism is very limited in Nigeria. The role of CDTT in Nigeria has not been done since the procedure was invented some decades ago. Our case was the first case of CDTT in Nigeria.
The principal aim of catheter-directed thrombectomy is to achieve rapid debulking of a large central occlusive thrombus to reduce the afterload and strain on the RV, thereby increasing pulmonary and systemic perfusion. However, the fragmentation process redistributes the thrombus into multiple smaller branches further downstream. The hemodynamic consequence of multiple smaller thrombi in a large volume of the peripheral arterial tree is believed to be less significant than that of a central thrombus in the main pulmonary artery.[6] Furthermore, by breaking up the large central thrombus into smaller fragments, it increases the surface area for exposure of the fibrinolytic agent or intrinsic thrombolytic enzymes to cause thrombus dissolution [7].
Conclusion
Catheter directed thrombolytic therapy is life-saving in patient with massive pulmonary embolism. Various techniques are available and is operator dependent. Patient received less amount of the alteplase and he improved.
References
- Kahn SR, Houweling AH, Granton J, et al. Long-term outcomes after pulmonary embolism: current knowledge and future research. Blood Coagul Fibrinolysis. 2014; 25: 407415.
- Celestine D, Agbor VN, Tankeu AT. Epidemiology of venous thromboembolism in Africa: a systematic review. Journal of Thrombosis and Haemostasis. 2017; 15: 1-13.
- Amar BJ, Dahri B, Aouina H, Bouacha H. venous thromboembolism in patients with acute tuberculosis. Rev Pneumol Clin. 2015; 71: 327-334.
- Bahloul M, Chaari A, Tounsi A, et al. Incidence and impact outcome of pulmonary embolism in critically ill patients with severe exacerbation of chronic obstructive pulmonary diseases. Clin Respir J. 2015; 9: 270-277.
- Torbicki A, Perrier A, Konstantinides S, et al, ESC Committee for Practice Guidelines (CPG). Guidelines on the diagnosis and management of acute pulmonary embolism: the Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC).Heart J. 2008; 29: 2276-2315.
- Girard P, Simonneau G. Catheter fragmentation of pulmonary J Vasc Interv Radiol. 2012; 23: 167-179.