Cephalic Vein Aneurysm: Report of a Case and Review of The Literature
Author'(s): José Aderval Aragão1*, Iapunira Catarina Sant’Anna Aragão2 , Felipe Matheus Sant’Anna Aragão2 and Francisco Prado Reis3
1Associate Professor, Department of Morphology, Federal University of Sergipe (UFS), and Titular Professor of the Medical School, Tiradentes University (UNIT), Aracaju, Sergipe, Brazil.
2Medical Student, University Center of Volta Redonda (UNIFOA), Volta Redonda, Rio de Janeiro, Brazil.
3Titular Professor, Medical School of Tiradentes University (UNIT), Aracaju, Sergipe, Brazil.
*Correspondence:
José Aderval Aragão, Titular Professor, Medical School of Tiradentes University (UNIT), Rua Aloisio Campos 500, Bairro Atalaia, Aracaju, Sergipe, Brazil, CEP: 49035-020, Tel: 79 - 99191-6767.
Received: 16 August 2020; Accepted: 09 September 2020
Citation: Aragão JA, Aragão ICS, Aragão FMS, et al. Cephalic Vein Aneurysm: Report of a Case and Review of The Literature. Cardiol Vasc Res. 2020; 4(4): 1-4.
Abstract
True aneurysms of the cephalic vein are extremely rare and its clinical manifestations are little known. A case of a cephalic vein aneurysm in a 58-year-old woman, with no history of local trauma or injury, is presented. Clinical examination and ultrasonic imaging confirmed the aneurysm. Histological examination revealed an irregular thickness of the venous wall, showing hematic thrombus within its lumen and papillomatous hyperplasia of endothelial cells. After the cephalic vein aneurysm was exposed, the proximal and distal stumps of the cephalic vein were isolated and ligated, and the aneurysm was resected
Keywords
Introduction
Venous aneurysms are rare entities, especially in the upper extremities, which is why they are poorly documented in the literature [1,2]. Its etiology may involve several factors, which may be associated with trauma, inflammation, congenital weakness, degenerative changes in the venous wall, endophlebohypertrophy and endophleboesclerosis processes, in addition to dialysis arteriovenous fistula [2,3]. In this article, we report a case of cephalic vein aneurysm at the height of the elbow fold of 2.0 cm in maximum diameter and review of the literature.
Case report
A 58-year-old female patient arrived at the office complaining of a superficial compressive mass in the fold of her right elbow about two years ago, bluish, painless, non-pulsatile, without thrill or murmur (Figure 1), which decreased in size and disappeared with the elevation of the arm and refilled when the arm was pending, with no history of injury, trauma, use of venous medications and which had been progressively increasing in the last six months. The radial and ulnar pulses were present and there were no signs of venous congestion from another pathology in her right arm.
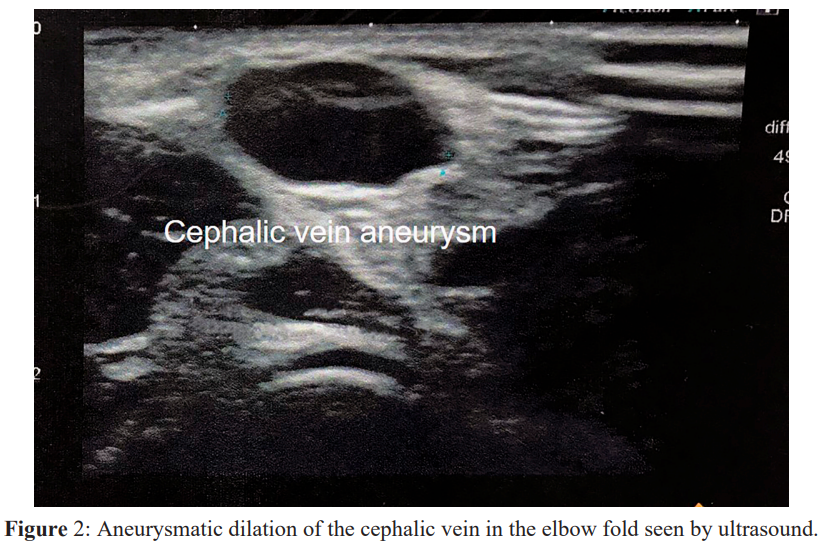
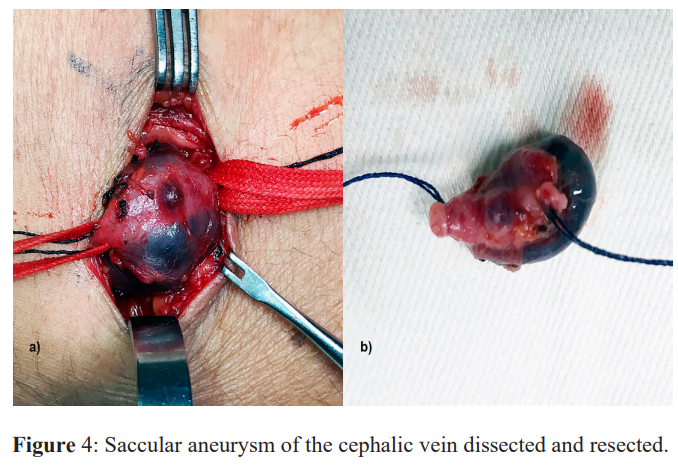
Subsequently, a venous duplex scan examination of the right upper limb was performed, where an aneurysmatic dilation of the cephalic vein with a thrombus at the height of the elbow crease of 2.0 cm in maximum diameter was observed (Figure 2). The patient was operated under local anesthesia with sedation. A longitudinal S-shaped incision was made in the elbow crease covering the skin and subcutaneous tissue (Figure 3). The venous aneurysm was carefully dissected (Figure 4a) and resected (Figure 4b) after ligation of the stumps of the proximal and distal ends of the cephalic vein. The aneurysm was sent for histopathological analysis and the patient was discharged on the first postoperative day. So far without complications, after two years of follow-up.
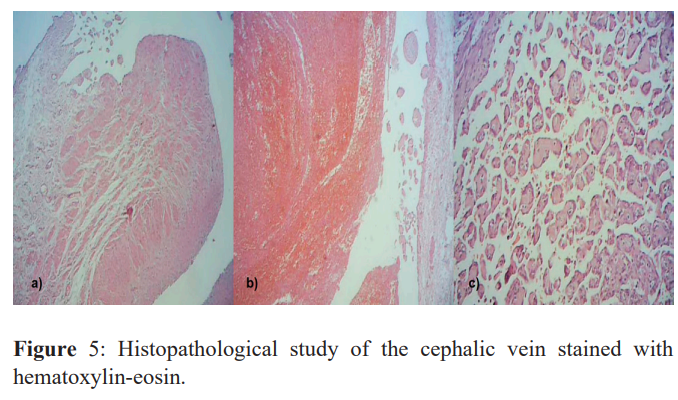
Histological examination revealed an irregular thickness of the venous wall (Figure 5a), showing hematic thrombus within its lumen (Figure 5b) and papillomatous hyperplasia of endothelial cells (Figure 5c).


Discussion
Cephalic vein aneurysms are clinical entities that do not appear to follow a pattern of presentation, and may vary between ages 12 to 67 years, in both sexes, according to literature reports [1,3-11]. In addition, the location of the cephalic vein involvement also seems to be variable, being found on the wrist, [5,6,11] forearm, [1,7,8] arm, [3,4,10] and even on the shoulder [9]. However, in our report, an unusual location of involvement was observed, at the height of the elbow.
Aneurysm diameters ranging from 1 to 7 cm have been reported in the literature, [1,3-11] and these variations are compatible with our finding, which was 2.0 cm in diameter. Regarding the clinical spectrum of symptoms, patients presented from asymptomatic, [1,7,8,11] with local discomfort, [5,9] edema, [3,10] paresthesia, [6,9] local pain, [4,6] pigmented purpura, [4] to pulmonary thromboembolism symptoms, with the venous aneurysm as a source of embolic load [10]. The physical examination was similar in all cases, with the majority of findings being of a palpable, compressible, non-pulsatile mass, with a reduction in size after the elevation of the affected limb.
The exam most commonly used to diagnose venous aneurysms is ultrasound with venous doppler, however depending on the clinical picture other diagnostic methods can be used such as venography, computed tomography angiography and magnetic resonance [1,3,5,7-11]. Regarding therapy, standard surgery is done through a longitudinal incision with resection of the aneurysm and ligation of the stumps [1,3-11]. There are still new techniques with endovascular procedures, however these still have an undefined role in the management of these injuries [12]. In our case, the treatment performed was surgical resection of the venous aneurysm with ligation of the proximal and distal stumps of the cephalic vein.
In our report, histopathological analysis revealed venous wall of irregular thickness, showing hematic thrombus within its lumen and papillomatous hyperplasia of endothelial cells. In the literature, it was possible to observe other histopathological presentations such as thinning of the inner and middle layers of the vein, with moderate chronic inflammatory infiltrate and blood deposits in the middle and outer layers, and incipient replacement of the outer layer with fibrous acellular tissue [5]; fragmentation of the elastic tissue and loss of the smooth muscle cells along with focal areas of endothelial denudation [6]; localized structural alteration with endoflebosclerosis of the vein wall, without the presence of clots [7]; flattened layer of endothelial cells and a considerable decrease in the number and size of the muscle and elastic fibers, however, all three layers of the normal vein wall were present [8]. In the study by Kobata et al [4], a histopathological aspect was found, which they consider as a new clinical entity called a dissecting venous aneurysm, with the following characteristics: complete loss and focal dissection of the medial and adventitious elastic fibers in the varied diluted aneurysmatic wall, without inflammatory focus.
Conclusion
Venous aneurysms and, especially, cephalic vein aneurysms are rare clinical entities and of uncertain etiopathogenesis, with few reports in the literature. Despite the rarity and the asymptomatic course in most cases, correct management is essential, not only for aesthetic purposes, but also to avoid possible complications, with pulmonary thromboembolism being the most feared of them. The initial diagnostic method can be done through doppler venous ultrasonography, as it is a test of good accuracy for diagnosis and of low cost, and surgical treatment has the gold standard of open surgery with aneurysmal resection and ligation of the stumps, since endovascular techniques still have an undefined role in correcting this pathology.
References
- Goto Y, Sakurada T, Nanjo H, et al. Venous aneurysm of the cephalic vein: report of a case. Surg Today. 1998; 28: 964-966.
- Schatz IJ, Fine G. Venous aneurysms. N Engl J Med. 1962;266: 1310-1312.
- Sótonyi P, Hidi L, Csobay-Novák C, et al. Giant cephalic vein aneurysm in a kidney transplant recipient with a brachiocephalic fistula and recurrent stenosis of the left brachiocephalic vein. J Vasc Surg Venous Lymphat Disord. 2018; 6: 244-245.
- Kobata T, Yamada S, Mizutani KI, et al. A Surgical Case of Venous Aneurysm of the Cephalic Vein with Unique Clinicopathological Findings for Venous Dissection: A Possible New Entity. Open J Cardiovasc Surg. 2018; 10: 1179065218785126.
- Antonopoulos CN, Liverakou E, Stamou C, et al. A Case of a Large Cephalic Vein Aneurysm. Ann Vasc Surg. 2019; 61: 472.e5-472.e8.
- Cakici M, Ersoy O, Ince I, et al. Unusual localization of a primary superficial venous aneurysm: a case report. Phlebology. 2014; 29: 267-268.
- Ekim H, Gelen T, Karpuzoglu G. Multiple aneurysms of the cephalic vein. A case report. Angiology. 1995; 46: 265-267.
- Faraj W, Selmo F, Hindi M, et al. Cephalic vein aneurysm.Ann Vasc Surg. 2007; 21: 804-806.
- Pierre-Louis WS, Tikhtman R, Bonta A, et al. Primary axillary venous aneurysm in a Young patient presenting with cardiac arrest. J Vasc Surg Cases Innov Tech. 2019; 5: 375-378.
- Wallace JR, Baril DT, Chaer RA. Upper extremity venous aneurysm as a source of pulmonar emboli. Ann Vasc Surg. 2013; 27: 240.e5-8.
- Wang ED, Li Z, Goldstein RY, et al. Venous aneurysms of the wrist. J Hand Surg Am. 2001; 26: 951-955.
- Teter KA, Maldonado TM, Adelman MA. A systematic review of venous aneurysms by anatomic location. J Vasc Surg Venous Lymphat Disord. 2018; 6: 408-413.