Circumcision of Male Children in the Community Service Project: The Characteristics and Prospective Follow up Study
Author'(s): Besut Daryanto*, Kurnia Penta Seputra, Reza Amorga and Hamdan Yuwafi Naim
Department of Urology, Faculty of Medicine Universities Brawijaya-Saiful Anwar General Hospital, Malang, East Java,Indonesia
*Correspondence:
Besut Daryanto, Department of Urology, Faculty of Medicine Universities Brawijaya-Saiful Anwar General Hospital, Malang, East Java, Indonesia.
Received: 15 March 2021; Accepted: 01 May 2021
Citation: Daryanto B, Seputra KP, Amorga R, et al. Circumcision of Male Children in the Community Service Project: The Characteristics and Prospective Follow up Study. Cancer Sci Res. 2021; 4(2): 1-3.
Abstract
Background & Objectives: Circumcision is a procedure that involves removing the prepuce, the fold of skin covering the head of the penis. Various medical and non-medical conditions are known indications for circumcision. Various medical benefits and complications are also known to be associated with circumcision. This study aims to provide an epidemiological characteristics of the indications and complications of circumcision.
Materials and Methods: This research is a prospective follow up study conducted in the context of a community service project on November 28th-29th, 2020. Circumcision was carried out according to medical and non-medical indications. Circumcision is performed by means of the dorsumcision technique. The operators were urology residents, surgery resident, and urologists.
Results: There were a total of 49 participants registered in this circumcision activity, but 5 people had not passed pre-screening conditions, so they were excluded. There were 44 participants who underwent circumcision with a mean age of 10.3 years, a BMI of 19.9 and a penis length of 5.26 cm. 14 participants (31.8%) did not experience phimosis, while the rest had phimosis to varying degrees. There were 6 participants who experienced bleeding after circumcision and 5 participants who experienced delayed wound healing at 1 week post-procedure monitoring. In the second week after the procedure, all participants experienced no symptoms of complications.
Conclusion: Effective and safe circumcision is performed by medical and non-medical indications. There are no long-term complications associated with circumcision.
Keywords
Introduction
Circumcision is a medical procedure that aims to remove the prepuce, the fold of skin covering the head of the penis. Etymologically, circumcision is formed from 2 words, namely circum, which means to rotate, and caedre, which means to cut. The act of circumcision has various implications that evolve. Traditionally, circumcision has been carried out concerning cultural identity and religious teachings since thousands of years ago. In the medical field, circumcision is useful to make it easier to maintain penile hygiene and reduce the risk of infection [1]. However, circumcision is still experiencing pros and cons, especially those related to complications from circumcision and penile sensitivity [2]. Globally, around 37 -39% of the male population has undergone circumcision, predominantly in Muslim and Jewish countries, which is about 62.1% [3,4].
Circumcision can be performed with various indications, both medically and non-medically. Non-medical indications are more common in circumcision, namely those related to religion and belief, without any medical reasons. Several medical indications for circumcision can be classified into preventive or curative measures. Circumcision with preventive aims includes preventing urinary tract infections, penile carcinoma, and HIV transmission. Circumcision is known to reduce the incidence of urinary tract infections, especially in children under 1 year of age. Circumcision also significantly reduced the incidence of penile carcinoma, up to only 0.1% in men who were circumcised. In adolescence and adulthood, circumcision is useful for reducing the incidence of heterosexual intercourse which has an impact on reducing HIV transmission [3,5].
Curative circumcision is indicated in several conditions, such as phimosis, paraphimosis, balanitis, and balanoposthitis. Physiological phimosis, which is non-retractile skin of the tip of the penis without any other pathological conditions, is not an indication of circumcision. Phimosis accompanied by signs of inflammation or scarring is classified as pathological phimosis which is an absolute indication of circumcision [2]. Some conditions to the contrary are contraindications to circumcision, either directly related to the penis or systemic conditions. Direct contraindications to the penis include hypospadias, epispadias, buried penis, and webbed penis, while systemic conditions that are contraindicated are the condition of premature babies and the presence of hemorrhagic diathesis [5].
Objective
This study aims to provide an epidemiological characteristics of the indications and complications of circumcision performed in a community project.
Material and Methods
This research is a prospective study in the the community service project for the act of mass circumcision on November 28th- 29th, 2020. The circumcision technique used in this study is the dorsumcision technique performed by professional medical personnel. All male children who have never experienced circumcision can be the subject of this study. Subjects with complicating conditions such as penile abnormalities (hypospadias, epispadias, webbed penis) and impaired coagulation function were excluded from this study and referred to hospital.
In this study, each research subject will be recorded for basic characteristics such as age, weight, height, penis length, and the presence of phimosis. After the circumcision procedure, monitoring of all patients for complications that may occur, such as bleeding and infection. Patient evaluation is done every week until 1 month after the procedure. All basic characteristics and monitoring data will be analyzed prospectively.
Result
Forty nine subjects who agreed to participate in this study, there were 5 subjects with complicated conditions, consist of 3 subjects with hypospadias, 1 subject with a penile webbed, and 1 subject with positive Covid-19. Forty four subjects included in this study, the mean of subjects was at school age with ideal BMIs, as shown in Table 1. The mean penis length varied with age, but overall it was within normal limits.
Phimosis conditions are found in many subjects of this study. As shown in Table 1, there were only 14 subjects (31.82%) who did not experience phimosis. The degree of phimosis used in this study was based on the Kikiros classification, from grade 1 to grade 5. All subjects had normal testicular positions.
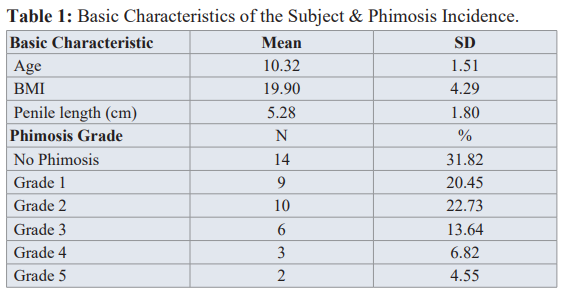
The complications from circumcision that appeared in this study consisted of early complications and further complications. Figure 1 An early complication of this study was bleeding in 6 (13.63%) subjects. All bleeding can be managed after the procedure and does not require further treatment in the hospital.
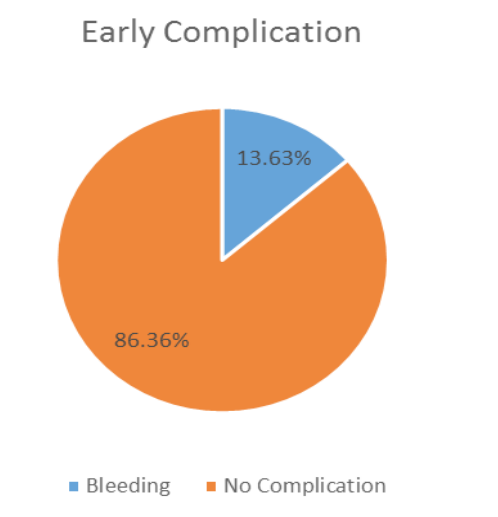
Figure 1: Early Complication of Circumcision.
From the evaluation of wound conditions in the first week after circumcision, there were 9 subjects with wounds that had not fully healed. The wounds are not completely dry and some are still bleeding serum from the wounds. At the second-week follow-up evaluation after circumcision, all subjects had experienced optimal wound healing. There were no other early or further complications in the subjects of this study. that the bleeding is mild. Infection is also an early complication that often occurs from several epidemiological studies of circumcision, but with the development of aseptic circumcision techniques, the condition of infection can be prevented [8].
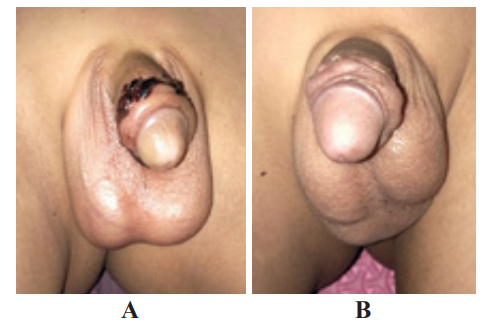
Figure 2: A. 1st week follow up after procedure. B. 4th weeks follow up after procedure. Results of Variables Correlation Analysis.
Discussion
The circumcision in this study uses the dorsumcision technique, mainly performed on boys of school age. This technique is used for children at the age after passing through the infancy period. In neonates and infants, circumcision techniques can be performed with the help of a Gomco clamp and Plastibell device which causes necrosis and detachment of prepuce tissue. The main medical indication for circumcision is phimosis, especially of a pathological nature. In the neonatal period, physiological phimosis is caused by natural adhesions between the glans penis and prepuce. At the age of 3-4 years as the penis grows, an accumulation of epithelial debris or smegma forms between the glans penis and prepuce which releases these natural adhesions [6].
In this study, 30 participants experienced phimosis out of a total of 44 participants (68.18%) with a mean age of participants in the range of 10 years. This condition is slightly higher than in some previous studies. The Canadian circumcision study in 202 participants reported phimosis results in 46.5% of participants [4]. There are 2 Japanese circumcision studies that described an increase in prepuce retraction from 0% in children aged 6 months to 38.4% in children aged 3 years and 62.9% in children aged 11-15 years [6]. This can be caused by the awareness of the community participants who took part in the circumcision project because they experienced symptoms and some other target participants who were in normal conditions without phimosis had experienced previous circumcision. The degree of phimosis obtained in the subjects of this study varied and most of them had low-grade phimosis which was not pathological.Complications from circumcision are rare, with the early adverse event rate from circumcision reaching 6% (range 2-14%) of the
10 previous prospective studies [7]. The most common early complication is bleeding, but it is often mild and can stop with pressure [3]. In this study, 6 participants (13.64%) experienced mild bleeding after the procedure, according to the prevalence of the previous study. This bleeding can be carried over at the circumcision site and does not require further treatment in the hospital, indicating Further complications from circumcision that can occur include obstructed wound healing. In this study, almost all participants had experienced a good wound healing process in the first week, only 9 people still had wounds that had not completely healed. In the second week after the procedure, all participants had achieved good wound healing. This is in accordance with several previous studies from Sokal et al. (2014) and Ma et al. (2018) who reported that circumcision wound healing until the penis is back in optimal condition takes up to 20 days with the dorsumcision technique. Various other circumcision techniques provide differences in the duration of the procedure and the pain that occurs during the procedure, but they do not significantly affect the wound healing interval [9,10].
Conclusion
Circumcision can be performed on medical or non-medical indications, with phimosis being the main medical indication. Early and advanced complications are rare and usually mild. Dorsumcision is a safe method for circumcision especially in public service setting.
References
- https://www.who.int/hiv/pub/malecircumcision/neonatal_ pdf
- Malone P, Steinbrecher H. Medical aspects of male circumcision. BMJ. 2007; 335: 1206-1290.
- Prabhakaran S, Ljuhar D, Coleman R, et al. Circumcision in the paediatric patient A review of indications, technique and complications. J Paediatr Child 2018; 54: 1299-1307.
- Brian J Morris, Richard G Wamai, Esther B Henebeng, et al. Estimation of country-specific and global prevalence of male Population health metrics. BioMed Central. 2016. 14: 4.
- Satyagraha P, Daryanto B, Seputra KP. Penerbit Mizwar. 2020.
- Hayashi Y, Kojima Y, Mizuno K, et al. Prepuce phimosis paraphimosis and circumcision. Scientific World Journal. 2011; 11: 289-301.
- Weiss HA, Larke N, Halperin D, et Complications of circumcision in male neonates infants and children a systematic review. BMC Urol. 2010; 10: 2.
- Krill AJ, Palmer LS, Palmer Complications of circumcision.Scientific World Journal. 2011; 11: 2458-2468.
- Sokal DC, Li PS, Zulu R, et al. Randomized controlled trial of the shang ring versus conventional surgical techniques for adult male circumcision safety and acceptability. J Acquir Immune Defic Syndr. 2014; 65: 447-455.
- Ma Q, Fang L, Yin W, et al. Chinese Shang Ring Male Circumcision A Review. Urol Int. 2018; 100: 127-133.