Clinical Characteristic of Inflammatory Bowel Disease Diagnosed in Kurdistan Center for Gastroenterology and Hepatology (Kcgh) – Asulaimaiyah-Iraqi Kurdistan-Iraq
Author'(s): Mohamed Abdulrahman Mohamed Alshekhani1*, Bakhtyar Faiq Salim2, Dr. Zana Nasraddin Mohialdeen3, and Bnar Jamal Hama Amin4
1College of Medicine, University of Sulaimani, Iraq.
2Gastroenterology and hepatology; MBChB, MD, College of Medicine, University of Sulaimani, Iraq.
3Assistant Professor in General Surgery, Sulaimanyah Polytechnic University, Department of Anaesthesia, Iraq.
4Sulaimani DOH, MOH, Iraq.
*Correspondence:
Mohamed Abdulrahman Mohamed Alshekhani, College of Medicine, University of Sulaimani, Iraq.
Received: 20 November 2020 Accepted: 02 December 2020
Citation: Alshekhani MAM, Salim BF, Mohialdeen ZN, et al. Clinical Characteristic of Inflammatory Bowel Disease Diagnosed in Kurdistan Center for Gastroenterology and Hepatology (Kcgh) – Asulaimaiyah-Iraqi Kurdistan-Iraq. Gastroint Hepatol Dig Dis. 2020; 3(2): 1-7.
Abstract
Background: Inflammatory bowel disease is comprised of two major disorders: ulcerative colitis and Crohn's disease, most patients have distinct features of either Crohn disease or ulcerative colitis, but approximately 5% to 10% have features of both diseases known as indeterminate colitis The incidence of inflammatory bowel disease varies widely between populations.
Objectives: The aim of the study to identify the clinical characteristic of patients diagnosed as inflammatory bowel disease in KCGH center in Slemani city.
Patients and Methods: This cross-sectional study was conducted in Kurdistan center of gastrointestinal and hepatobiliary disease in Sulaimani city during 16 months from Sep. 2013 to Feb. 2015, during this period we included 74 newly diagnosed patients in whom the diagnosis of UC and CD was confirmed by clinical, laboratory, endoscopic and histological examination, all patients were subjected to full history, clinical examination findings, endoscopic feature and histopathological findings. Data of all patients were entered into statistical package for social sciences software for Windows, version 18.
Results: In total, 74 new cases of IBD [75.7% ulcerative colitis 21.6% chron’s disease, 2.7% indeterminate were identified during a 16 months period from sep./2013; mean age 35±14 years, young age groups (20-39 years) were more prevalent, Females (52.7%) were more than males (47.3%), No significant differences were observed between UC patients and Chron’s patients regarding age and gender (p>0.05), There was a significant association between bleeding per rectum and ulcerative colitis patients (p<0.001). Abdominal pain was significantly associated with Chron’s patients (0.03). Among ulcerative colitis patients, proctitis was the main type (39.3%) while in patients with Chron’s, iliocolonic involvement was predominant (50%).
Conclusions: The rate of Chron’s has increased significantly in comparison to other studies done in Iraq and near countries; IBD most commonly present in 20- 39 year, unlike most of the western studies there was no second peak in old age group, although the number of elderly was too small in this study, to draw a solid conclusion.
Keywords
Introduction
Inflammatory bowel disease (IBD) is comprised of two major disorders: ulcerative colitis (UC) and Crohn's disease (CD), most patients have distinct features of either Crohn's disease or ulcerative colitis, but approximately 5% to 10% have features of both diseases (known as indeterminate colitis) [1].
Ulcerative colitis — Ulcerative colitis is a chronic inflammatory condition characterized by relapsing and remitting episodes of inflammation limited to the mucosal layer of the colon. It almost invariably involves the rectum and may extend proximally and continuously to involve other portions of the colon. [1]Crohn's disease — Crohn's disease is characterized by transmural inflammation and by skip lesions. The transmural inflammatory nature of Crohn's disease often leads to fibrosis and obstructive clinical presentations that are not typically seen in ulcerative colitis. The transmural inflammation can also result in sinus tracts that burrow through and penetrate the serosa, giving rise to micro- perforations and fistulae [1,2]. IBD in developing countries like ours had been characterized by the predominance of the occurrence of ulcerative colitis in far excess compared to Crohn's disease but in recent years there have been reports of increased prevalence of Chrons disease in these countries in parallel with westernization of lifestyles specialty dietary habits [3-5]. The aim of the study to identify a clinical characteristic of patients diagnosed as Inflammatory bowel disease (IBD) in KCGH center in Slemani city; clinical subtyping namely UC, CD or IC, gender differences and clinical presentations.
Patient and Methods
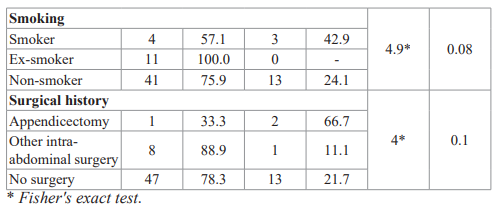
This cross-sectional study was done in Kurdistan center of gastrointestinal and hepatobiliary disease (KCGH) in Sulaimani city for 16 months from Sep./ 2013 to Feb./ 2015. During this period 74 patients were diagnosed in whom the diagnosis of UC and CD was confirmed by clinical, laboratory, endoscopic and histologic examination. The patients were subjected to full history, clinical examination findings; questionnaire contains the patient demographic data, clinical feature and family history of IBD. All patients asked about drugs like (NSAIDs, oral contraceptive pill, Antibiotics) that are known to have an association with IBD [18- 20,23]; also asked about surgical history like (appendicectomy and other intraabdominal surgery) that are known to have an association with IBD [47]. Data of all patients were entered into a computerized software, and a database was made, then transferred into a statistical package for social sciences (SPSS) software for Windows, version 18, US. Descriptive statistics were presented as mean ± standard deviation for continuous variables, and as frequencies (number) and percentages for categorical variables. Chi-square was used to compare frequencies and percentages in between any two groups and Fisher's exact test was used if more than 20% expected variables were less than 5. The level of significance of ≤ 0.05 was considered significant. Finally, the results were presented in tables and or figure with an appropriate explanation for each table or figure according to the findings.
Results
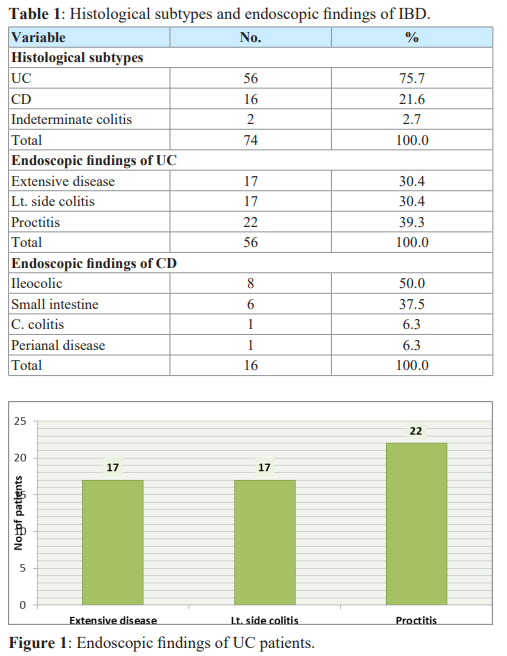
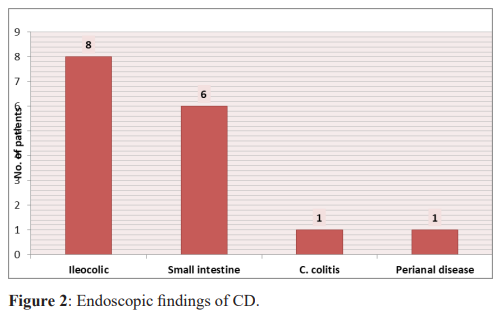
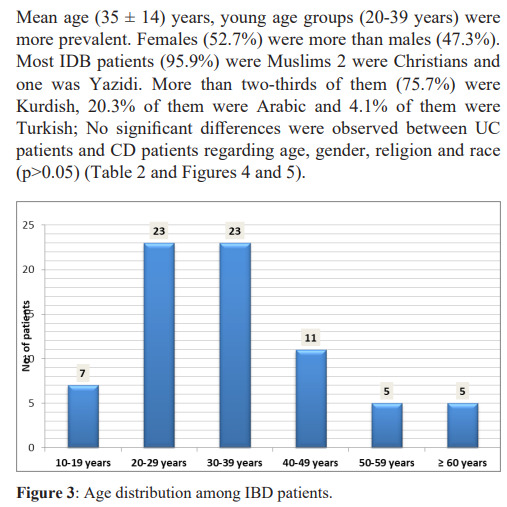
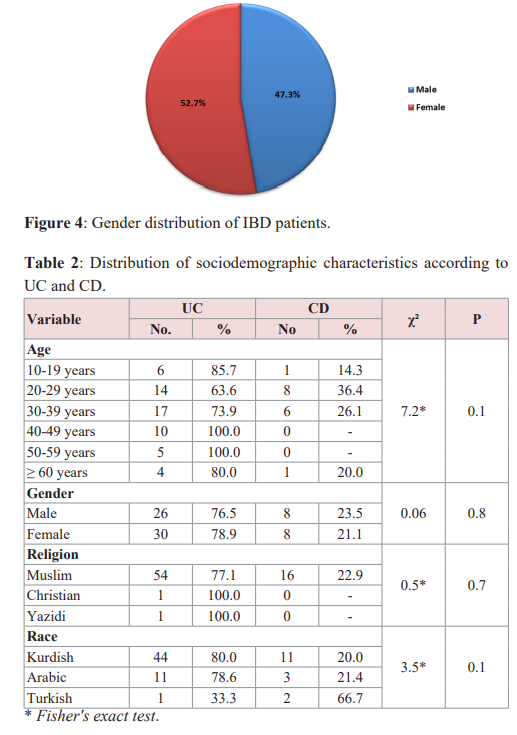
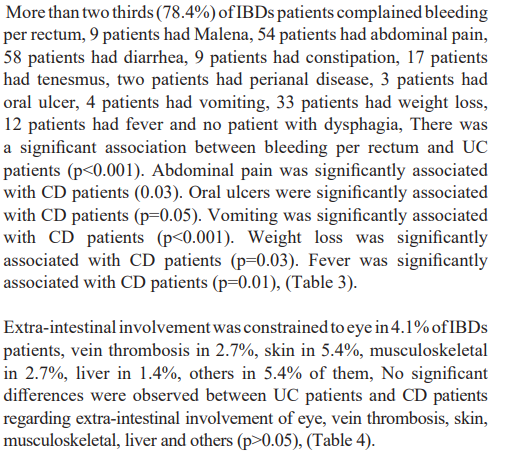
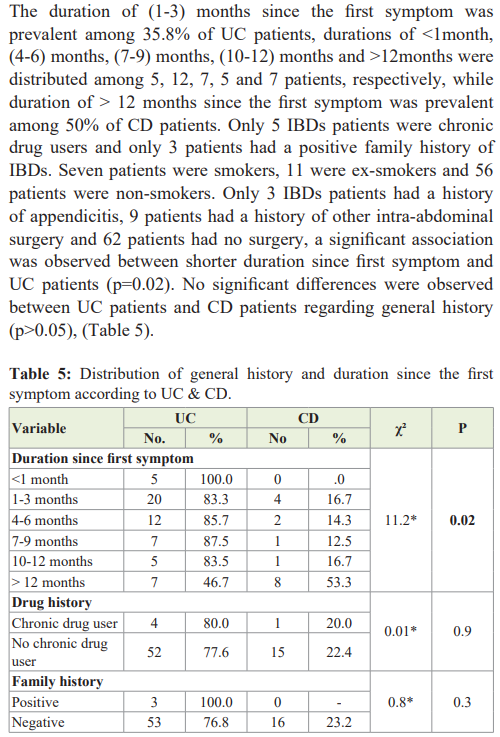
A total of seventy-four patients with inflammatory bowel diseases (IBDs) were included in the present study, Histological examination revealed that 75.7% of IBDs patients were Ulcerative Colitis, 21.6% of them were Crohns disease and 2.7% of them were indeterminate colitis. The endoscopic findings of UC revealed that 17 patients had extensive disease, 17 patients had left-sided colitis and 22 patients had proctitis. Endoscopic findings of Crohn's disease revealed that 50% of them were ileocolonic, 37.5% small intestine, 6.3% C. colitis and 6.3% of them perianal disease (Table 1 and Figures 1-3).
Discussions
UC and CD are chronic inflammatory bowel diseases whose pathogenesis and pathologic state remain to be clearly defined. Knowledge of various incidence and prevalence rates, as well as clinical features of IBD in different geographic areas or races, may provide insight into possible risk factors and mechanisms that contribute to the occurrence of IBD [50].
In this study peak age of onset for IBD is 35 year which correlate with study conducted by Amira et al. [63] 35.5 year in Iraq, yang SK et al. [51] 35 year in Korea and by Leong et al. [52] 34 year in China, while it is lower in study done by Morita N et al. [53] 24 year in Japan. The ratio of male to female patients was (0.9/1), which show a slight female gender predominance for IBD that is exactly similar to 2 studies done by Amira et al. [63] in Iraq and Vahedi et al. [54] in Iran (0.9/1), it is also comparable to a large study done by Rubin et al. [67]. In the United Kingdom (0.87/1) but differ from a study done by Fallahi et al. [55] in Iran in which male patients are predominant and the ratio was (1.5/1). We did not find a second peak in the elderly mentioned by previously mentioned studies, although the number in this age group was too small to draw a solid conclusion, the same with the Amira et al. study [63].
The presence of rectal inflammation in UC makes bleeding the most consistent presenting feature and this may be gross [28], in the present study bleeding per rectum is the most common presenting feature and it is significantly associated with UC (p<0.001) which is compatible with two studies done by Aghazadeh et al. [56] and Vahedi et al. [54 ] in Iran, but in contrast to a study done by Park et al. [57] in Korea in which diarrhea is a most common clinical presentation. The presentation of CD is determined by the side, extent, severity, and complications of intestinal and extra- intestinal disease, Chronic diarrhea is the most common presenting complaint and abdominal pain and weight loss are present in over 60% of patients at diagnosis [37] ; in this study, presence of abdominal pain as a first common presenting feature, it is significantly associated with CD (p<0.03) and diarrhea as a second common presenting feature, this is comparable to two studies done by Vahedi et al. [54] in Iran and Park et al. [57] in Korea.
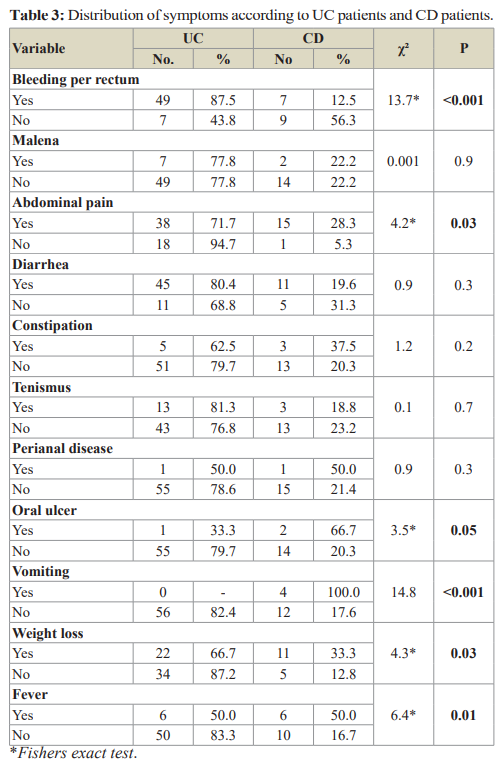
In this study, 11 (14.9%) patients develop extraintestinal manifestations concomitantly with GI symptoms, 7 patients have single organ involvement while 4 of them have 2 organ involvement; skin involvement is the most common type (5.4%), while eye, musculoskeletal, deep vein thrombosis and liver (primary sclerosing cholangitis and transaminitis) are present in (4.1%), (2.7%), (2.7%) and (1.4%) respectively; it is hard to compare with other studies because of two reasons, first: only symptomatic extra-intestinal manifestations that are present concomitantly with GI symptoms are diagnosed and documented, second: development of these features needs long term to follow up and some of these do not follow the disease activity.
In the present study family history for UC is 4.1% which is higher than a study done by Wang et al. [58] (2.1%) in China and lower than other study done by Vahide et al. [54] (10.2%) in Iran; there is no family history for our CD patients, this is compatible with a study done by Thia et al. [59] (0%) in Singapore but differ from most of other study, Needless to say, we should bear in mind geographical differences or even different interactions between genetic and environmental factors and small number of patient in our study explain these variations.
Smoking is associated with an increased risk of Crohn’s disease, In contrast, current smoking is not a risk factor for and may be protective of the development of ulcerative colitis [13]; Our data support the hypothesis of smoking in UC. However, it is hard to draw any firm conclusion regarding CD since the sample size is small and the smoking habits of the general population is not known.
Among IBD patients, the prevalence of UC is (75.7%) and CD (21.6%), this is slightly higher for CD in a study done by Amira et al. [63] in which (82%) for UC and (17%) for CD done in Iraq; our study differ from reports in other part of the world in which UC more than (90%) and CD prevalence less than (10%) like Wiercinska et al. [68] in Poland, Ishibashi et al. [69] in Japan and Wang et al. [54] in china; while reports in some European countries show that CD is more prevalent than middle east countries like Lactose et al. [70] in Croatia in which CD (61%) and Wierska et al. [71] in Romania (34.5%) for CD. Ulcerative proctitis is the most common form of UC accounting (40-50%) of cases while left side colitis second most common. [26]; in this study proctitis is the most common form (39.3%) while left-sided colitis and extensive disease are equal (30.4%) in which extensive disease is increasing, this is explained by the fact that all cases included in his study are diagnosed in our tertiary center. this is compatible with a study done by Amira et al. [63] in Iraq and Abdul-Baqi et al. [60] in Lebanon in which proctitis(31.4%) and (52.3%) respectively, while differ from two studies done by Jiang et al. [61] in china in which left side colitis are the most common type and Fujimoto et al. [62] in Japan in which extensive disease is the commonest type.
Among CD patients in our study, illiocolonic type is the most common (50%) and small intestinal type is second most common (37.5%), this is comparable to study done by Amira et al. [63] in Iraq in which illiocolonic (43.7%) and small intestinal disease is second common; illiocolonic disease also commonest type in two other studies done by Abdul- Baqi et al. [60] in Lebanon and Vahedi et al. [54] in Iran, in contrast to a study done by Aghazadeh et al. [56] in Iran in which small intestinal disease is the most common type (43.7%).
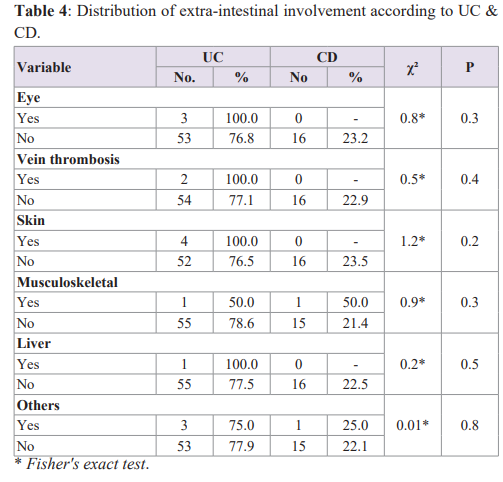
Patients with Crohn's disease have a longer mean time to diagnosis than patients with UC, and as many as 25% of patients have a delay in diagnosis of over 2 years from the onset of symptoms [64]. In this study, the time for diagnosis since the first symptom is more for CD than UC probably because of the diversity of symptoms. Meantime for diagnosis of UC is 6 months, this time is lower in comparison to a study done by Masnadi Shirazi et al. [65] in Iran (14 months) and higher than a study done by Vjess et al. [66] in Denmark (4.5 month). This time for CD in our study 16 month which is higher in comparison to the two previously mentioned studies (Masnadi Shirazi and Vjess) in which the meantime was (12 and 11 months) respectively.
Conclusion
- The rate of CD has increased significantly in comparison to other studies done in Iraq and near countries.
- IBD most commonly present in 20- 39 year and unlike western trends, there is no second peak in the old age group.
- Meantime for diagnosis of CD is more than UC like most of the eastern and western studies.
Recommendations
- Extra- intestinal manifestations should be looked for and diagnosed with the diagnosis of IBD because a significant number of patients had these manifestations concomitantly with GI symptoms.
- The diagnosis of CD delay in comparison to the UC, for the future it is important to search for other modality like serology, radiology or stool calprotectin and not only depend on current
- It is important to have another study in our center to assess and estimate factors that exactly lead to a delay in the diagnosis of CD in our country in comparison to other countries.
References
- Gasche C, Scholmerich J, Brynskov J, et al. A simple classification of Crohn's disease: report of the Working Party for the World Congresses of Gastroenterology, Vienna 1998. Inflamm Bowel Dis. 2000; 6: 8-15.
- Silverberg MS, Satsangi J, Ahmad T, et al. Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: Report of a Working Party of the 2005 Montreal World Congress of Gastroenterology. Can J Gastroenterol. 2005; 19: 5A-36A.
- Gilat T, Grossman A, Fireman Z, et al. Inflammatory bowel dis-ease in In: McConnell R, Rozen R, Langman M, Gilat
- (eds). The Genetics and Epidemiology of Inflammatory Bowel Disease. New York: Karger. 1986.
- Calkins BM, Lilienfeld AM, Garland CF, et al. Trends in the incidence rates of ulcerative colitis and Crohn's disease. Dig Dis Sci. 1984; 29: 913-920.
- Sedlack RE, Nobrega FR, Kurland LT, et al. Inflammatory colon disease in Rochester, Minnesota, 1935–1964. Gastroentero-logy. 1972; 62: 935-941.
- Miller DS, Keighley AC, Langman Changing patterns in epidemiology of Crohn's disease. Lancet. 1974; 2: 691- 693.
- Beaugerie L, Seksik P, Nion-Larmurier I, et al. Predictors of Crohn's disease. Gastroenterology. 2006; 130: 650-656.
- Bruce R. Bacon. Inflammatory bowel disease. Int HARRISON'S principle of INTERNAL MEDICINE, 18th edition. 2012; 295: 2477.
- Logan RF, Edmond M, Somerville KW, et al. Smoking and ulcerative colitis. Br Med J (Clin Res Ed). 1984; 288: 751.
- Sutherland LR, Ramcharan S, Bryant H, et al. Effect of cigarette smoking on the recurrence of Crohn's disease. Gastroenterology. 1990; 98: 1123-1128.
- Cosnes J, Beaugerie L, Carbonnel F, et Smoking cessation and the course of Crohn's disease: an intervention study. Gastroenterology. 2001; 120: 1093-1099.
- Boyko EJ, Perera DR, Koepsell TD, et Effects of cigarette smoking on the clinical course of ulcerative colitis. Scand J Gastroenterol. 1988; 23: 1147-1152.
- Harries AD, Jones L, Heatley RV, et al. Smoking habits and inflammatory bowel disease: effect on nutrition. Br Med J (Clin Res Ed). 1982; 284: 1161.
- Sandborn WJ, Tremaine WJ, Offord KP, et al. Transdermal nicotine for mildly to moderately active ulcerative A randomized, double-blind, placebo-controlled trial. Ann Intern Med. 1997; 126: 364-371.
- Pullan RD, Rhodes J, Ganesh S, et al. Transdermal nicotine for active ulcerative colitis. N Engl J Med. 1994; 330: 811-
- Glassman MS, Newman LJ, Berezin S, et Cow's milk protein sensitivity during infancy in patients with inflammatory bowel disease. Am J Gastroenterol. 1990; 85: 838-840.
- Kaser A, Sebastian Zeissig, Richard Blumberg. Inflammatory bowel disease. Annu Rev Immunol. 2010; 28: 573-621.
- Wurzelmann JI, Lyles CM, Sandler Childhood infections and the risk of inflammatory bowel disease. Dig Dis Sci. 1994; 39: 555-560.
- Virta L, Auvinen A, Helenius H, et Association of repeated exposure to antibiotics with the development of pediatric Crohn's disease--a nationwide, register-based finnish case- control study. Am J Epidemiol. 2012; 175: 775-784.
- Ananthakrishnan AN, Higuchi LM, Huang ES, et Aspirin, nonsteroidal anti-inflammatory drug use, and risk for Crohn disease and ulcerative colitis: a cohort study. Ann Intern Med. 2012; 156: 350-359.
- Felder JB, Korelitz BI, Rajapakse R, et al. Effects of nonsteroidal anti-inflammatory drugs on inflammatory bowel disease: a case-control study. Am J Gastroenterol. 2000; 95: 1949-1954.
- Bonner GF, Fakhri A, Vennamaneni SR. A long-term cohort study of nonsteroidal anti-inflammatory drug use and disease activity in outpatients with inflammatory bowel disease. Inflamm Bowel Dis. 2004; 10: 751-757.
- Mahadevan U, Loftus EV Jr, Tremaine WJ, et al. Safety of selective cyclooxygenase-2 inhibitors in inflammatory bowel disease. Am J Gastroenterol. 2002; 97: 910-914.
- Sandborn WJ, Stenson WF, Brynskov J, et al. Safety of celecoxib in patients with ulcerative colitis in remission: a randomized, placebo-controlled, pilot study. Clin Gastroenterol Hepatol. 2006; 4: 203-211.
- http://emedicine.medscape.com/article/179037-overview
- Brian R. Walker. Inflammatory bowel disease. Davidson's Principles and Practice of Medicine, 22 2014; 22: 898.
- Schumacher G, Sandstedt B, Kollberg B. A prospective study of first attacks of inflammatory bowel disease and infectious Clinical findings and early diagnosis. Scand J Gastroenterol. 1994; 29: 265-274.
- Rao SS, Read NW, Davison PA, et al. Anorectal sensitivity and responses to rectal distention in patients with ulcerative colitis. Gastroenterology. 1987; 93: 1270-1275.
- Rao SS, Holdsworth CD, Read NW. Symptoms and stool patterns in patients with ulcerative Gut 1988; 29: 342-345.
- Farmer RG, Easley KA, Rankin Clinical patterns, natural history, and progression of ulcerative colitis. A long-term follow-up of 1116 patients. Dig Dis Sci. 1993; 38: 1137.
- Langholz E, Munkholm P, Davidsen M, et Changes in the extent of ulcerative colitis: a study on the course and prognostic factors. Scand J Gastroenterol. 1996; 31: 260-266.
- Moum B, Ekbom A, Vatn MH, et Change in the extent of colonoscopic and histological involvement in ulcerative colitis over time. Am J Gastroenterol 1999; 94: 1564-1569.
- Gan SI, Beck A new look at toxic megacolon. An update and review of incidence, etiology, pathogenesis, and management. Am J Gastroenterol. 2003; 98: 2363-2371.
- Truelove SC, Witts LJ. Cortisone in ulcerative colitis; final report on a therapeutic trial. BMJ. 1955; 2: 1041-1048.
- Carter MJ, Lobo AJ, Travis Guidelines for the management of inflammatory bowel disease in adults. Gut. 2004; 53: 6.
- Langholz E, Munkholm P, Davidsen M, et al. Course of ulcerative colitis: analysis of changes in disease activity over the years. Gastroenterology. 1994; 107: 3-11.
- Sands BE. From symptom to diagnosis. Clinical distinctions among various forms of intestinal inflammation. Gastroenterology. 2004; 126: 1518-1532.
- Schwartz DA, Loftus EVJr, Tremaine WJ, et al. The natural history of fistulizing Crohn's disease in Olmsted County, Minnesota. Gastroenterology. 2002; 122: 875-880.
- Auvin S, Molinie F, Gower-Rousseau C, et al. Incidence, clinical presentation and location at diagnosis of pediatric inflammatory bowel disease: a prospective population-based study in northern France (1988–1999). J Pediatr Gastroenterol Nutr. 2005; 41:49-55.
- Su CG, Judge TA, Lichtenstein GR. Extraintestinal manifestations of inflammatory bowel disease. Gastroenterol Clin North Am. 2002; 31: 307.
- Kim SC, Ferry Inflammatory bowel diseases in pediatric and adolescent patients: clinical, therapeutic, and psychosocial considerations. Gastroenterology. 2004; 126: 1550-1560.
- Wagtmans MJ, Verspaget HW, Lamers CB, et al. Clinical aspects of Crohn's disease of the upper gastrointestinal tract: a comparison with distal Crohn's Am J Gastroenterol. 1997; 92: 1467-1471.
- van Hogezand RA, Witte AM, Veenendaal RA, et Proximal Crohn's disease: a review of the clinicopathologic features and therapy. Inflamm Bowel Dis. 2001; 7: 328-337.
- Poggioli G, Stocchi L, Laureti S, et Duodenal involvement of Crohn's disease: three different clinicopathologic patterns. Dis Colon Rectum. 1997; 40: 179-183.
- Farmer M, Petras RE, Hunt LE, et al. The importance of diagnostic accuracy in colonic inflammatory bowel disease. Am J Gastroenterol. 2000; 95: 3184-3188.
- Farmer RG, Whelan G, Fazio Long-term follow-up of patients with Crohn's disease. Relationship between the clinical pattern and prognosis. Gastroenterology. 1985; 88: 1818-1825.
- Guindi M, Riddell RH. Indeterminate colitis. J Clin Pathol. 2004; 57: 1233-1244.
- Sandborn WJ, Fazio VW, Feagan BG, et al. AGA technical review on perianal Crohn's disease. Gastroenterology. 2003; 125: 1508-1530.
- Patrick Alguire. Inflammatory bowel disease. Medical Knowledge Self-Assessment Program, 16 edition. 36-37.
- Brian R. Walker. Inflammatory bowel disease. Davidson's Principles and Practice of Medicine, 22 2014; 22: 897.
- Feshareki R, Soleimani H. Crohn's disease in Isfahan; report of a case. Pahlavi Medical Journal. 1976; 7: 565 - 575.
- Leong RW, Lau JY, Sung The epidemiology and phenotype of Crohn's disease in the Chinese population. Inflamm Bowel Dis. 2004; 10: 646-651.
- Morita N, Toki S, Hirohashi T, et Incidence and prevalence of inflammatory bowel disease in Japan: nationwide epidemiological survey during the year 1991. J Gastroenterol. 1995; 30: 1-4.
- Vahedi H, Merat S, Momtahen S, et al. Epidemiologic characteristics of 500 patients with inflammatory bowel disease in Iran studied from 2004 through 2007. Arch Iran Med. 2009; 12: 454-460.
- Fallahi GH, Moazzami K, Tabatabaeiyan M, et al. Clinical characteristics of Iranian pediatric patients with inflammatory bowel disease. Acta Gastroenterol Belg. 2009; 72: 230-234.
- Aghazadeh R, Zali MR, Ali Bahari, et inflammatory bowel disease in Iran. A review of 457 cases. J Gastroenterol hepatol. 2005; 20: 1691-1695.
- Park SH, Young Min Kim, Suk-kyun Yang, et al. Clinical features and natural history of ulcerative colitis in Korea. Inflamm Bowel Dis. 2007; 13: 278-283.
- Wang YF, Zhang H, Ouyang Q. Clinical manifestations of inflammatory bowel disease: East and West J Dig Dis. 2007; 8: 121-127.
- Thia KT, Widjaja Luman, Ooi Choon Jin, et al. Chrons disease runs a more aggressive course in young Asian Inflamm Bowel Dis. 2006; 12: 57-61.
- Abdul-Baki H, ElHajj I, El-Zahabi LM, et al. Clinical epidemiology of inflammatory bowel disease in Lebanon. Inflamm Bowel Dis. 2007; 13: 475-480.
- Jiang Y, Xia B, Jiang L, et al. Association of CTLA-4 gene microsatellite polymorphism with ulcerative colitis in Chinese patients. Inflamm Bowel Dis. 2006; 12: 369-373.
- Fujimoto T, Kato J, Nasu J, et al. Change of clinical characteristics of ulcerative colitis in Japan: analysis of 844 hospital-based patients from 1981 to Eur J Gastroenterol Hepatol. 2007; 19: 229-235.
- Amira H Shubbar, HH Makki H fayadh, HHH Raghad J AL- Akayshi. Chronic Colitis: Clinical, endoscopic & histological Evaluation of 130 Iraqi patients. IJGE. 2001; 1: 11-17.
- Vavricka SR, Spigaglia SM, Rogler G, et al. Systematic evaluation of risk factors for diagnostic delay in inflammatory bowel disease. Inflamm Bowel Dis. 2012; 18: 496-505.
- Masnadi Shirazi, Mohammad Hossein Somi, Yoosef Bafandeh, et al. Epidemiological and Clinical Characteristics of Inflammatory Bowel Disease in Patients from Northwestern Middle East Journal of Digestive Diseases. 2013; 5: 86- 92.
- Jess T, Riis L, Vind I, et Changes in clinical characteristics, course, and prognosis of inflammatory bowel disease during the last 5 decades: A population-based study from Copenhagen, Denmark. Inflamm Bowel Dis. 2007; 13: 481-489.
- Rubin GP, Hungin AP, Kelly PJ, et al. Inflammatory bowel disease: epidemiology and management in an English general practice Aliment Pharmacol Ther. 2000; 14: 1553- 1559.
- Wiercinska-Drapalo A, Jaroszewicz J, Flisiak R, et al. Epidemiological characteristics of inflammatory bowel disease in North-Eastern Poland. World J Gastroen-terol 2005; 11: 2630-2633.
- Ishibashi N, Hirota Y, Ikeda M, et al. Ulcerative colitis and colorectal cancer: a follow-up study in Fukuoka, Japan. Int J Epidemiol. 1999; 28: 609-613.
- Lakatos L, Lakatos PL. Is the incidence and prevalence of inflammatory bowel diseases increasing in Eastern Europe? Postgrad Med J. 2006; 82: 332-337.
- Wierska-Drapalo A, Jaroszewicz J, Flisiak R, et al. Epidemiological characteristics of inflammatory bowel disease in North-Eastern World J Gastroenterol. 2005; 11: 2630-2633.