Cocaine Induced Peripheral Artery Occlusion Resulting in Critical Limb Ischemia
Author'(s): Kathryn Collins, DO, Ryan Senese, DO and Anantha Ramanathan, MD*
Dept of Surgery, Nassau University Medical Center, 2201, Hempstead Tpke, East Meadow, NY 11554.
*Correspondence:
Anantha Ramanathan, Dept of Surgery, Nassau University Medical Center, Hempstead Tpke, East Meadow, NY, Tel: +1929 365 7501.
Received: 04 December 2020; Accepted: 29 December 2020
Citation: Collins K, Senese R, Ramanathan A. Cocaine Induced Peripheral Artery Occlusion Resulting in Critical Limb Ischemia. Cardiol Vasc Res. 2020; 4(5): 1-5.
Abstract
Introduction: Cocaine addiction is a common health problem. While Cocaine’s effects on the heart and the cerebrovascular system are well documented and studied, cases of peripheral arterial occlusion from Cocaine use are uncommon in the literature.
Case: A case of a forty six year old man with cocaine induced common iliac artery thrombosis which was successfully treated by stenting is presented.
Discussion: Cocaine induced peripheral arterial disease is discussed along with possible mechanisms.
Conclusion: Physicians should be aware of Cocaine use as one of the possible risk factors for peripheral arterial occlusion.
Keywords
Introduction
Cocaine induced peripheral artery occlusion is rare. Few cases of this phenomenon have been reported to date. The vast majority of literature involving cocaine related vascular events pertain to small diameter vessels such as coronary and cerebral vessels [1]. We present a case of a relatively healthy 46 year-old male who developed cocaine induced occlusion of the right common iliac artery. This case not only highlights the detrimental effects of cocaine on peripheral vasculature in the younger, healthier patient population, but also underscores the importance of recognizing cocaine use as a risk factor for peripheral artery disease and acute or acute on chronic limb ischemia.
Case Report
Vascular surgery was consulted for a 46 year-old male with pain, tissue loss and absent pulses in the right lower extremity. He stated that the pain began two months prior after an injury to his right foot at work. He denied previous medical or surgical history, except for 1-2 pack years of smoking over the past five years. Notably there was no history of diabetes, hypertension, and hypercholesterolemia or coronary artery disease. However he admits to the daily use and handling of cocaine for the past several years. There was also a history of intermittent marijuana use.
On physical exam, this was an otherwise healthy looking African American patient writhing in pain and unable to lie comfortably. The patient was acutely hypertensive during this presentation. His right lower extremity foot pulses were not palpable. Femoral and popliteal pulses were decreased on the right side as well. The full complement of pulses was palpable on the left side. A round shaped wound with a necrotic rim was noted on the right lateral malleolus, and a 5th toe lateral wound was also present. The right foot was limited in range of motion, was tender to palpation, and dusky red.
Review of his chart showed that the patient had x-rays of his right foot that did not show evidence of fractures or osteomyelitis. He had mild leukocytosis (11.63) and his Urinalysis tested positive for cocaine and marijuana. Other laboratory findings were noncontributory.
Peripheral arterial studies including Pulse Volume Recordings (PVR) and Ankle-Brachial Index (ABI) were obtained. Results of the study showed severe arterial inflow disease in the right lower extremity when compared to the left lower extremity (Figure 1).
The patient had an angiogram performed under conscious sedation after the urinalysis tested negative for cocaine. His pain and blood pressure required pharmacological management during the procedure. An aortogram and runoff angiogram was performed which demonstrated a focal area of occlusion and stenosis, 3cm long, in the right common iliac artery extending a short distance from the aortic bifurcation (Figure 2a). The area was stented using a balloon mounted stent. The completion aortogram revealed excellent flow through the right iliac system without any stent impingement of the left side (Figure 2b).
There was immediate improvement of the pain and the blood pressure returned to baseline. Bilateral lower extremity pulses were palpable post operatively. The patient subsequently underwent a fifth toe amputation.
Follow-up PVR and ABI studies demonstrated no right arterial inflow disease (Figure 3).
Discussion
Cocaine is an alkaloid psychoactive substance that comes from the plant Erythroxylon coca. Its use has been around for thousands of years and stems from the indigenous people of South America [2,3]. It is also one of the most frequently used addictive recreational drugs resulting in emergency room visits [4]. There are well-documented adverse effects to cocaine, including cardiovascular disease, cardiac ischemia, cardiac arrhythmias, cerebrovascular accidents, intestinal ischemia, and seizures [1,3,5]. However, cocaine-induced peripheral artery occlusion is rare and only a few cases have been reported on this topic. The peripheral arteries involved have included brachial, iliac, femoral and popliteal arteries [1,6-8]. Some of these reports have described simultaneous involvement of multiple arteries. The presentation could be acute or chronic.
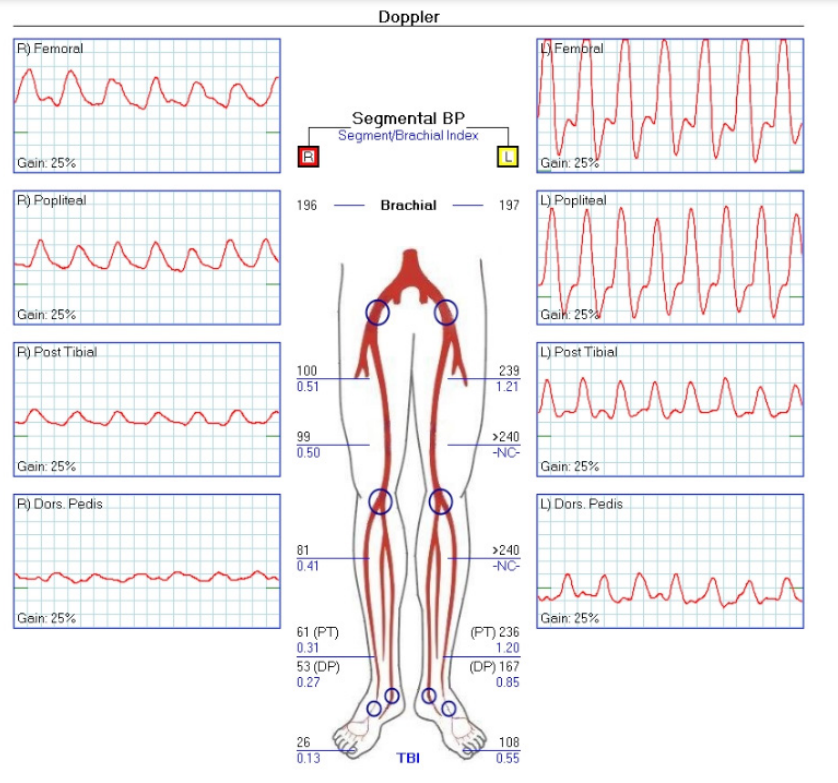
Figure 1: Pre-operative Doppler and segmental pressures showing severe inflow disease.
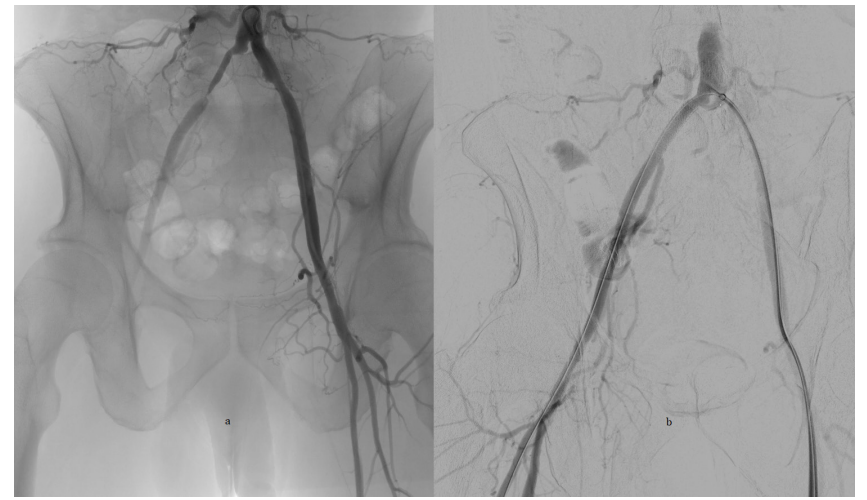
Figures 2a and b: Angiogram demonstrating the critical area of stenosis and occlusion in the right common iliac artery pre- and post-stenting.

Figure 3: Post-operative Doppler and segmental pressures showing resolution of arterial occlusion.
The mechanism by which cocaine causes arterial occlusion is not well understood. It is known that cocaine increases norepinephrine by promoting its release and preventing its reuptake [3,5,9]. Norepinephrine is a potent vasoconstrictor, acting on the alpha- adrenergic receptors of smooth muscle cells and resulting in higher levels of endothelin-1, a vasoconstrictor protein elevated in cocaine users [3,5,10]. Endothelin-1 ultimately causes vasospasm, creating high stress on the vessels resulting in endothelial injury, platelet aggregation and clot formation acutely [3,5,11]. Cocaine also induces an elevated pro-inflammatory cascade (e.g., Tumor necrosis factor alpha, Interleukin 1B) leading to inflammation and accelerated atherosclerosis that is seen in chronic users [5,12]. Cocaine usage could lead to arterial dissection due to vessel wall damage and hypertension [3,5,13]. The patient in this case most likely had a combination of acute and chronic cocaine induced peripheral artery occlusion of mixed etiology.
Recognizing the symptoms and knowing the risk factors of peripheral arterial disease (PAD) is important for diagnosis, timely treatment, and limb preservation. Peripheral artery disease is uncommon before the age of 50 and the incidence rises sharply with age thereafter. In the Limburg peripheral arterial occlusive disease study that based PAD on ABI, incidence was 1.7 per 1000 at the age of 40-55 years [14]. Since our patient is a relatively healthy 46 year-old male, with no medical comorbidities and no history of heavy smoking, it is unlikely that his symptoms were due to peripheral artery disease but rather due to cocaine-induced arterial thrombosis.
Once the diagnosis of cocaine-induced arterial thrombosis is made, intervention is needed to preserve and reestablish arterial circulation to the affected limb(s). Depending on the severity of symptoms and physical exam, different treatment strategies have been explored. In patients with no ischemic symptoms, systemic anticoagulation can be considered [15]. Intra-arterial nitroglycerine and iloprost may be tried if spasm is thought to be a significant factor [8]. On the contrary, patients with ischemic symptoms need urgent operative intervention. One case required open embolectomy after failed balloon angioplasty, although no clot was retrieved [8]. Treatment algorithms for cocaine induced chest pain recommend the use of bare metal stents where necessary [3]. In our case we took a minimally invasive approach, performing an angiogram with balloon mounted bare metal stenting of the right common iliac artery. The completion aortogram showed reperfusion without any further complications. The symptoms resolved, proving that urgent minimally invasive endovascular stenting is a viable option for treatment.
Conclusion
The effects of cocaine on the cardiac and cerebral systems has been widely recognized and studied, however there are few cases of peripheral vascular compromise from cocaine use, making it a difficult diagnosis. The prompt recognition and early surgical intervention resulted in resolution of the patient’s symptoms. Physicians should be aware of cocaine induced peripheral arterial disease as a potential diagnosis in the appropriate patient presentation.
References
- Chen JC, Hsiang YN, Morris C, et al. Cocaine- induced multiple vascular occlusions: A case report. J Vasc Surg. 1996; 23: 719-723.
- Cregler LL. Adverse health consequences of cocaine abuse. J Natl Med Assoc. 1989; 81:27-38.
- Havakuk O, Rezkalla SH, Kloner RA. The Cardiovascular Effects of Cocaine. J AmColl Cardiol. 2017; 70: 101-113.
- Schwartz BG, Rezkalla S, Kloner RA. Cardiovascular effects of cocaine. Circulation. 2010; 122: 2558-2569.
- Bachi K, Mani V, Jeyachandran D, et al. Vascular disease in cocaine addiction. Atherosclerosis. 2017; 262: 154-162.
- Zhou W, Lin PH, Bush RL, et al. Acute arterial thrombosis associated with cocaine abuse. J Vasc Surg. 2004; 40: 291- 295.
- Gutierrez A, England JD, Krupski WC. Cocaine-induced peripheral vascular occlusive disease--a case report. Angiology. 1998; 49: 221-224.
- McMullin CM, Bayat I, Rytina E, et al. Coughlin PA. Profound acute limb ischemia affecting all four limbs following cocaine inhalation. J Vasc Surg. 2015; 61: 504-506.
- Rothman RB, Baumann MH, Dersch CM, et al. Amphetamine - type central nervous system stimulants release norepinephrine more potently than they release dopamine and serotonin. Synapse. 2001; 39: 32-41.
- Claudia G Sáez, Karla Pereira-Flores, Roberto Ebensperger, et al. Atorvastatin reduces the proadhesive and prothrombotic endothelial cell phenotype induced by cocaine and plasma from cocaine consumers in vitro. Arterioscler Thromb Vasc Biol. 2014; 34: 2439-2448.
- Siegel AJ, Sholar MB, Mendelson JH, et al. Cocaine-Induced Erythrocytosis and Increase in von Willebrand Factor: Evidence for Drug-Related Blood Doping and Prothrombotic Effects. Arch Intern Med. 1999; 159: 1925-1929.
- Joana C M Narvaez, Pedro V Magalhães, Gabriel R Fries, et al. Peripheral toxicity in crack cocaine use disorders. Neurosci Lett. 2013; 544: 80-84.
- Daniel JC, Huynh TT, Zhou W, et al. Acute aortic dissection associated with use of cocaine. J Vasc Surg. 2007; 46: 427- 433.
- Hooi JD, Kester AD, Stoffers HE, et al. Incidence of and risk factors for asymptomatic peripheral arterial occlusive disease: a longitudinal study. Am J Epidemiol. 2001; 153: 666-672.
- Webber J, Kline RA, Lucas CE. Aortic thrombosis associated with cocaine use: report of two cases. Ann Vasc surg. 1999; 13: 302-304.