Continuous Moderate Exercise Influence on Cardiac Remodeling in Patients Underwent Percutaneous Coronary Intervention
Author'(s): Ahmed Galal A. Fattah Fahmy MD1, Gamal Abdel Hady MD1, Mai Helmy Hassan MD2, Kareem Mohsen Moussa MD3 and Mohamed EL Bordy MD1*
1Department of Cardiology, National Heart Institute, Cairo, Egypt.
2Department of Physical therapy, National Heart Institute, Cairo, Egypt.
3Department of Radio diagnosis, Faculty of Medicine, Cairo University, Egypt.
*Correspondence:
Mohamed EL Bordy, Ahmed Galal, Department of Cardiology, National Heart Institute, Cairo, Egypt, Cairo Post office NO: 11461, Egypt.
Received: 28 May 2021; Accepted: 02 July 2021
Citation: Fattah Fahmy AGA, Hady GA, Hassan MH, et al. Continuous Moderate Exercise Influence on Cardiac Remodeling in Patients Underwent Percutaneous Coronary Intervention. Cardiol Vasc Res. 2021; 5(4): 1-5.
Abstract
Background: Following myocardial infarction (MI), left ventricle (LV) remodeling is a complex and multifactorial mechanism with therapeutic and prognostic consequences. Medications that reduce LV remodeling increase survival and quality of life. Exercising following a myocardial infarction (MI) is effective according to several trials. The implications on operation and remodeling, however, are still debated
Aim of work: To evaluate continuous moderate-intensity aerobic training effects by using cardiac magnetic resonance imaging on left ventricular remodeling after one month of percutaneous coronary intervention (PCI) following myocardial infarction.
Methods: Forty eligible patients (5 females and 35 males) who had PCI after one month of having MI with age 45-65 years old. They underwent conventional medical treatment in addition to a supervised intensive recovery regimen that included 36 hours of continuous moderate aerobic exercise (three times /week for 12 weeks). Evaluation of the effect of this program was done by magnetic resonance imaging (CMR) to calculate EF.
Result: This research was done on 40 patients (5 females and 35 males) who had PCI after myocardial infarction. The mean age of the participants was 54.1 ± 7.0. Most patients have Killip class I. LAD was the culprit artery in 70% of the patients. The most common risk factors were smoking, dyslipidemia, and overweight. Post-treatment BMI decreased compared with pre-treatment BMI (p <0.05) for an improvement average of 5.37 percent. There was also a substantial improvement in the pretreatment systolic blood pressure and functional parameters as compared for post-treatment (p<0.05). As regard cardiac MRI, There was a significant reduction in post-treatment LV mass (117.2 ± 27.2) relative to pretreatment (128.7 ± 38.9). EF % was marked improvement from 49.32 ± 5.12 to 56.63 ± 5.49 (P value < 000.1). EDV and all other parameters show marked improvement post treatment as compared to pretreatment.
Conclusion: Moderate-intensity aerobic exercise improved LV remodeling after percutaneous coronary intervention (PCI) one month following myocardial Infarction.
Keywords
Introduction
Background
The process of regional and global structural and functional changes in the heart, known as cardiac remodeling, result from loss of viable myocardium, exuberant inflammatory reaction, elevated wall tension in the boundary zone and remote myocardium, and neurohormonal activity. The "adverse" notation applies both to the unfavourable modifications from a hemodynamic point of view and to the processes negative prognostic consequences [1].
In the present reperfusion age, the frequency and degree of adverse ventricular remodeling have decreased dramatically. Acute in- hospital MI mortality has declined markedly, and left ventricular (LV) systolic activity and an impressive 1-year survival rate have been achieved by most MI survivors. However, patients undergoing adverse ventricular remodeling have considerably greater in-hospital and short-term mortality, so the causes and processes of adverse ventricular remodeling following MI need to be established and reversed.
Exercise impact on myocardial activity and LV remodeling after MI remain controversial. According to some studies, exercise following MI can worsen cardiac function further due to increased stress on the infarcted region, aneurysm formation, infarct expansion, or a decrease in ejection fraction (EF). Otsuka Y et al., [2] refuted these conclusions, claiming that exercise has little effect on ventricular parameters regardless of training intensity [3,4]. Other studies have shown that exercise can mitigate and even reverse ventricular remodeling following an.
Exercise following PCI can benefit coronary heart disease CHD. by increasing LVEF and decreasing their risk of myocardial infarction, cardiac death, angina pectoris, coronary angioplasty, and restenosis [5].
Periodic Exercise Training (ET) improves cardiac ischemic disorders, general and cardiac-specific morbidity and mortality. ET boosts the need for myocardial oxygen, improving the supply of coronary blood, increases the supply of myocardial oxygen, which decreases angina frequency, myocardial infarction and increases coronary blood pressure by working specifically on the vasculature by strengthening endothelial function, cardiac vasodilation promotion. In addition, ET increases collateralization by lowering the supply of blood to the ischemic myocardium, coronary induration progression of the arteries and restenosis by stabilizing atherosclerotic lesions possibly. ET is a relatively secure and inexpensive solution. It can be used for Prevention in CAD and treatment [6].
LV remodeling has been tested by echocardiography for a long time. However, as opposed to cardiovascular magnetic resonance imaging (CMR), there are many drawbacks to echocardiography, such as poor vision and prone reproducibility. With a high resolution and signal to noise ratio, CMR is considered to be the golden norm for cardiac activity and structure evaluation [7].
Aim of work
To use cardiac magnetic resonance imaging to evaluate moderate- intensity aerobic activity effects on ventricular remodeling in patients who have had recent myocardial infarction managed by primary PCI.
Material and Methods
This research is pre-post test research. It was carried out in the National Heart Institute, and Kasr E lEini hospital, Cairo, Egypt.
Subjects
Forty eligible patients (5 females and 35 males) after one month of successful primary PCI after having MI. They were selected from National Heart Institute, coronary care unit. They were recruited according to the following criteria: Successful procedure of PCI, their age are 45-65, and all patients were medically stable with no treatment regimen significant changes during the study, Ejection Fraction >40%, BMI (class I-II obesity), controlled mild to moderate hypertensive patients, controlled diabetic patients (type II).
The patients were excluded if they had congestive Heart failure, unstable angina, uncontrolled hypertension, unsuccessful PCI (persistent obstruction more than 30%), cardiogenic shock, ventricular arrhythmias, uncontrolled diabetes and patients with neurological, neuromuscular and orthopedic diseases.
Ethical approval
All participants were briefed about the trial purpose and consequences. An informed written consent form (documented by the ethical committee) was taken from each patient prior to the study. The study had local research and ethics committee approval by the Ethical Review Board of General Health Organization of Teaching Hospitals and Institutes (GOTHI).
Evaluative procedures
Symptom limited exercise test
To record maximum Heart Rate (Max HR) and resting heart rate (RHR). For one minute, patients pedalled at a work pace of 30 W without any additional load. The rate was raised by 30 watts/3 minutes before the patients became symptomatic. During the final 15 seconds of each stage third minute, the maximum heart rate was measured. At the start, the resting heart rate was registered. The exercise test ends with a cool-down stage during which the patient pedals for a fleeting time against zero resistance [8].
Cardiac MRI
were done at Kasr Elini hospital before and after training procedure. MR images were assembled around the long vertical axis (2- and 4-chamber view) and a small stack of axes (contiguous 8-mm- thick slices) spanning the extension of the ventricle. To test the LV mass, LV dimensions, and EF, the later sequence was used. Using Image J.22, LV end-systolic volume and LV end-diastolic volume (LVEDV) were computed using Simpson's law. The LV mass was measured and compounded by the specific myocardial gravity (1.05g/mL) by the sum of the myocardial region (LV epicardial contour minus LV endocardial contour) times the slice thickness.
The LVEF, divided by LVEDV and multiplied by 100, was determined as the difference between LVEDV and LV end-systolic volume. No injection of gadolinium was used [9].
Training procedure
Moderate continuous aerobic training (MCT)
Patients underwent a supervised individual training program based on Symptom limited exercise test result. They were trained using the heart rate range or reserve method (Karvonen's method); training heart rate (THR=HRrest + (HRmax – HRres) 55-80% This formula is the most accurate one [10].
- The session began with a ten-minute warm-up routine consisting of steady riding or quiet Each patient underwent supervised individual instruction based on the outcome of the symptom-limited exercise test.
- Mode of exercise: Bicycle ergometer and treadmill.
- Intensity of exercise: Thirty min of moderate-intensity aerobic training at 60 to 75% of maximum heart rate [11].
- Duration: 50 min session (10 min warming up -30 min conditioning phase and 10 min cooling down)
- After the rehabilitation session ended, all patients had a ten- minute cooling down period.
- Intensity and duration of the exercise program was progressively increased throughout the three months program, as individual tolerance and according to max HR.
Frequency: three times /week for three months.
- All participants were closely monitored using ECG telemetry to control exercise intensity
- To monitor the progression of exercise strength in patients exercising at 11–13 RPE in the absence of symptoms, the Borg rate of perceived exertion (RPE) scale was
- Patient assessment included rating perceived exertion (RPE), constant ECG monitoring, and pre-and post-activity tracking of heart rate, blood pressure, and symptoms. To avoid affecting the study outcomes, patients taking beta-blockers or other rate- lowering medications maintained their current dosage during the study
Statistical analysis
Data analysis was conducted using SPSS, Chicago, IL, USA) version 22 for windows. According to the normality of the data, the mean and standard deviation or median with interquartile range (IQR) were used to summarize numerical variables. To summarize categorical variables, numbers and percentages were used. Comparisons between quantitative variables were performed using independent student's t-test for normally –distributed data or Mann Whitney U test for non-normally-distributed data. Categorical variables were compared using the Chi-square test. Kaplan-Meier curves were used for estimating survival. They were compared using the methods described by Klein and Moeschberger. The significance level was set at a p-value of < 0.05.
Inferential statistic- Mixed ANOVA was used to compare different inside the group.
Results
This research was done on 40 patients (5 females and 35 males) who had PCI after myocardial infarction. The mean age of the participants was 54.1 ± 7.0. Most patients have Killip class 1 LAD was the culprit artery in 70% of the patients. The most common risk factors were smoking, dyslipidemia, and overweight (Table 1).
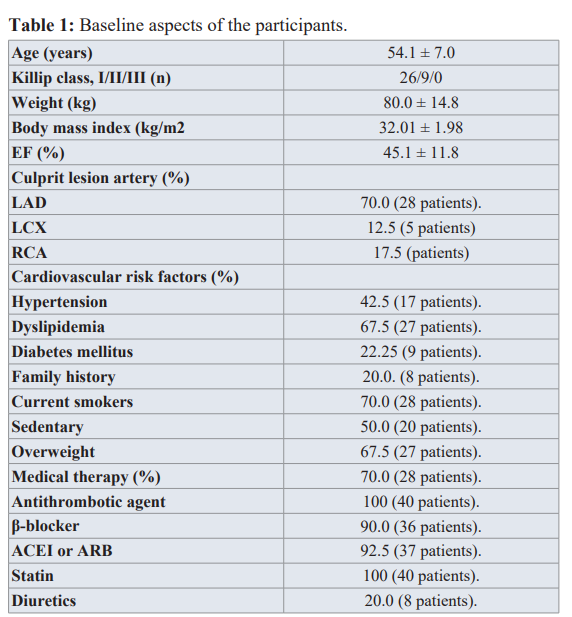
EF: Ejection Fraction; LAD: Left Anterior Descending; LCX: Left Circumflex; RCA: Right Coronary Artery; ACEI: Angiotensin-converting Enzyme Inhibitors; ARB: Angiotensin-Receptor Blockers.
There has been a large decrease in post-treatment BMI compared with pre-treatment BMI (p <0.05) for an improvement average of 5.37 percent. There was also a substantial improvement in the pre-treatment systolic blood pressure and functional parameters as compared to post- treatment (p<0.05).
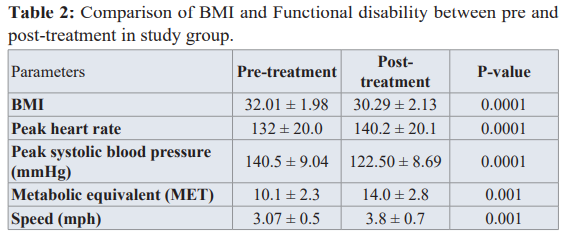
Data was presented as mean ± SD
BMI: Body Mass Index; LV-36: Left Ventricular Questionnaire; EF: Ejection Fraction.
Regarding cardiac MRI, There was a significant reduction in post- treatment LV mass relative to pre-treatment. EF, EDV, and all other parameters show marked improvement post-treatment as compared to pre-treatment (Table 3).
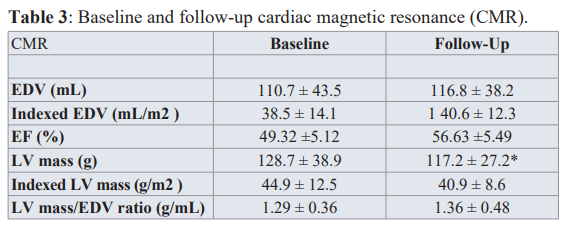
Data was presented as mean ± SD
EDV: End-Diastolic Volume; EF: Ejection Fraction; LV: Left Ventricular.
*p = 0.0032.
Discussion
This study was designed to evaluate continuous moderate exercise training effect on left ventricular remodeling after percutaneous coronary intervention (PCI) one month following myocardial infarction. According to the result of this research, post-treatment revealed high efficacy of the intervention in EF measurement demonstrates that the effects of cardiovascular exercise and post-MI remodeling are controlled by a variety of mechanisms: increased endothelial function, decreased preload, decreased systemic vascular resistance, autonomic system change, decreased blood pressure and heart rate at rest and sub-maximal loads, and decreased LV wall tension [14].
Additionally, our research is consistent with Izeli et al., [15], who examined the impact of moderate-intensity aerobic exercise on cardiac function in patients following a first myocardial infarction using cardiac magnetic resonance. The study found that moderate- intensity aerobic exercise enhanced physical capacity and other cardiovascular variables and that there was a trend toward positive remodeling in the trained population, with an increase in left ventricular diastolic dimension unrelated to an increase in ventricular mass. Due to the fact that echocardiographic mass and function measurements were made using 2D echocardiographic techniques that relied on formulas and assumptions about the LV geometric shape, direct comparisons can be challenging.
Dubach et al, [16] conducted a study on twenty-five patients with decreased LVEF (32.3 ± 6%) following myocardial infarction. Twelve patients were randomly assigned to participate in a rehabilitation center high-intensity physical activity program. Both groups of patients underwent CMR tests at baseline and after two months. The increases in LV end-systolic volume and LVEDV were non-significant (2.5% and 4.8%, respectively) in the TG group. No changes in LV mass or EF were reported in the groups. The same patients were tracked for one year, with one group engaging in intense physical activity and expelling approximately 2,100 Kcal more energy per week than the control group.
Myers J [17], found no significant change in cardiac length, mass, or function, suggesting no adverse effect of cardiac rehabilitation. Schmid et al., [18] tested thirty-eight patients post-MI with an EF of 50.4 ± 12.7% who were randomly assigned to 12 weeks of mixed endurance and resistance training or endurance training alone by magnetic resonance imaging (CMR) provided positive LV remodeling and alteration of cardiovascular risk factors.
CMR has been used in fewer trials to measure mass and function as a reliable instrument for calculating volumes and masses in both normal and pathological scenarios. CMR has been thoroughly validated. Pennell DJ., [12] has also shown that after an intervention, small samples can be used to correctly assess volume and mass changes. No improvement in LVEF or LVEDV, which may represent optimized pharmacological therapy, was observed after aerobic exercise training in both groups. Furthermore, LV mass decreased in the training group and increased marginally in the control group. Since both groups were identical with respect to MI traits, it seems logical to lift the hypothesis that the aerobic exercise intervention may be due to this opposite trend.
The negative exercise effect on cardiac remodeling, as found by Nakada I et al. [13] is not supported by our findings. The literature At the training period end, CMR revealed a small improvement in stroke volume, EF, end-systolic volume, and LVEDV in both groups. There was no evidence of a detrimental impact on remodeling.
Conclusions
The modest diastolic LV size increase associated with a decrease in LV mass observed in the current study indicated that our patients underwent positive remodeling. This was accomplished by moderate-intensity aerobic exercise, which was shown to be effective in fostering beneficial cardiovascular adaptations and lowering cardiovascular risk factors.
References
- Seropian IM, Toldo S, Van Tassell BW, et Anti- inflammatory strategies for ventricular remodeling following ST-segment elevation acute myocardial infarction. J Am Coll Cardiol. 2014; 63: 1593-1603.
- Otsuka Y, Takaki H, Okano Y, et Exercise training without ventricular remodelling in patients with moderate to severe left ventricular dysfunction early after acute myocardial infarction. Int J Cardiol. 2003; 87: 237-244.
- Wisløff U, Støylen A, Loennechen JP, et Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: a randomized study. Circulation. 2007; 115: 3086-3094.
- Giallauria F, Cirillo P, Lucci R, et Left ventricular remodelling in patients with moderate systolic dysfunction after myocardial infarction: favourable effects of exercise training and predictive role of Nterminal pro-brain natriuretic peptide. Eur J Cardiovasc Prev Rehabil. 2008; 15: 113-118.
- Hu Zhang, Rong Chang. Effects of Exercise after Percutaneous Coronary Intervention on Cardiac Function and Cardiovascular Adverse Events in Patients with Coronary Heart Disease: Systematic Review and Meta-Analysis. Journal of Sports Science and Medicine. 2019; 18: 213-222.
- Bruning RS, Sturek Benefits of exercise training on coronary blood flow in coronary artery disease patients. 2015; 57: 443-453,
- Suinesiaputra Am Bluemke DA, Cowan BR, et Quantification of LV function and mass by cardiovascular magnetic resonance: multi-center variability and consensus contours. Journal of Cardiovascular Magnetic Resonance. 2015; 17: 63.
- Chatterjee S, Sengupta S, Nag M, et al. Cardiopulmonary Exercise Testing: A Review of Techniques and Applications. J Anesthe Clinic Res. 2013; 340-346.
- Abràmoff MD Magalhães PJ, Ram Image processing with image. J Biophotonics International. 2004; 11: 36-42.
- Kennedy K, Adams J, Cheng D, et al. High intensity track and field training in a cardiac rehabilitation program : Proc (BaylUniv Med Cent). 2012; 25: 34-36.
- Cardozo GG, Oliveira RB, Farinatti Effects of High Intensity Interval versus Moderate Continuous Training on Markers of Ventilatory and Cardiac Efficiency in Coronary Heart Disease Patients. Scientific World Journal. 2015; 1-8.
- Pennell Cardiovascular magnetic resonance in the quantitative assessment of left ventricular mass, volumes and contractile function. Coronary Artery Dis. 2005; 16: 337-343.
- Nakada I, Yasu T, Katsuki T, et al. Exercise at ventilatory threshold aggravates left ventricular remodeling in patients with extensive anterior acute myocardial Am Heart J. 2004; 147: 113-120.
- Zheng H, Luo M, Shen Y, et al. Effects of 6 months exercise training on ventricular remodelling and autonomic tone in patients with acute myocardial infarction and percutaneous coronary J Rehabil Med. 2008; 40: 776-779.
- Nataly L Izeli, Julio C Crescencio, Antonio Pazin-Filho, et Effects of cardiac rehabilitation on left ventricle function and mass evaluated by cardiac magnetic resonance imaging in post myocardial infarction patients. Journal of Cardiovascular Magnetic Resonance. 2011; 13: 167.
- Dubach P, Myers J, Dziekan G, et Effect of exercise training on myocardial remodeling in patients with reduced left ventricular function after myocardial infarction: application of magnetic resonance imaging. Circulation. 1997; 95: 2060-2067.
- Myers J. Effects of exercise training on abnormal ventilatory responses to exercise in patients with chronic heart failure. Congest Heart 2000; 6: 243-249.
- Schmid JP, Anderegg M, Romanens M, et combined endurance/resistance training early on, after a first myocardial infarction, does not induce negative left ventricular remodeling. Eur J Cardiovasc Prev Rehabil. 2008; 15: 341-346.