Correlation between Diagnostic Accuracy of TIMI Clinical Score and Nuclear Myocardial Perfusion Imaging in Non ST-Elevation Acute Coronary Syndrome
Author'(s): Dr. S. M. Salman Habib1*, Prof. Abdul Rasheed Khan2, Dr. Bushra Sabeen1, Dr. Rizwan Khan3, Dr. Riffat Sultana4 and Prof. Sultana Habib4
1Department of Nuclear Medicine, Karachi Institute of Radiotherapy & Nuclear Medicine, Pakistan.
2Department of Cardiology, Abbasi Shaheed Hospital, Pakistan.
3Department of Adult Cardiology, National Institute of Cardiovascular Diseases, Pakistan.
4Karachi Institute of Heart Disease, Pakistan.
*Correspondence:
Dr. S. M. Salman Habib, Consultant Nuclear Physician and Head Department of Nuclear Medicine, Karachi Institute of Radiotherapy & Nuclear Medicine (KIRAN), Karachi, Pakistan, Tel: 0092-3003568661.
Received: 01 March 2021; Accepted: 30 March 2021
Citation: Habib S, Khan R, Sabeen B, et al. Correlation between Diagnostic Accuracy of TIMI Clinical Score and Nuclear Myocardial Perfusion Imaging in Non ST-Elevation Acute Coronary Syndrome. Cardiol Vasc Res. 2021; 5(2): 1-7.
Abstract
Objectives: The study aimed to compare diagnostic accuracy of TIMI clinical score and nuclear MPI in Non-STE-ACS.
Material and Methods: In this cross-sectional comparative study, a total of 94 patients were included for the year (June 2019 to May 2020) with history of chest pain; provisionally diagnosed either (i) Non-STEMI or (ii) unstable angina. Patients excluded from the study (i) having provisional diagnosis of STEMI (ii) NSTEMI patient with high risk TIMI score (iii) individuals having UA with low risk TIMI score (iv) having recent history of PCI or CABG within 30 days (v) with history of renal failure (vi) hemodynamically unstable patients and (vii) having non-cardiac chest pain. The study population was divided into two major groups on the basis of result of cardiac marker (troponin-I) i.e. NSTEMI (group-A: i.e. positive biomarkers having chest pain at time interval upto 12
hours; n=41) and Unstable angina (group-B: i.e. negative biomarkers for the same period; n=53). TIMI score was calculated of all enrolled patient on the basis of clinical risk score system. Further sub-grouping (A-I, A-II, B-I & B-II) was done using clinical TIMI score as: low risk (0-2), intermediate score (3-4) and high risk (score 5-7). Angiography was performed as gold standard in all groups.
Results: All true and false, positive or negative results were taken into account, and results were divided into groups and subgroups. The sensitivity and specificity of MPI in patients with “low risk TIMI score-NSTEMI” (subgroup A-I) were found to be 92.8% (95% CI 66.13-99.82) and 81.25% (95% CI 54.35- 5.9) with p-value of 0.0001; while sensitivity and specificity of MPI in patients with “intermediate TIMI score- NSTEMI” (subgroup A-II) were found to be 100% (95% CI 47.82-100) and 80.0% (95% CI 35.88-99.58) with p-value of 0.005. The data of subgroup A-I and A-II were found statistically significant while using “Coronary Angiography (CA) as gold standard”. The sensitivity and specificity of MPI in patients having “intermediate TIMI score UA” (subgroup B-I) were found to be 86.67% (95% CI 59.54-98.34), 82.6% (95% CI 68.78-97.45) with p-value of 0.0001; while sensitivity and specificity of MPI in patients having “high TIMI score UA” (subgroup B-II) were found to be 100% (95% CI 59.04-100) and 80.0% (95% CI 28.35-99.49%) with p-value of 0.0038. The data of subgroup B-I and B-II were also found statistically significant while using “Coronary Angiography as gold standard”.
Conclusion: This study concludes that TIMI score is not an ideal tool for exact categorization of patient with NSTE-ACS. Therefore; MPI is more specific to identify definite intermediate and high risk patients allowing early referral or intervention for management, and to reduce health cost burden.
Keywords
Introduction
Cardiovascular diseases (CVDs) are still number one cause of death globally especially in developing countries. Among several causes of CVD, coronary artery disease (CAD) is the most prevalent manifestation of CVD in developing countries rather than in developed countries due to inappropriate life style. It is estimated that by 2030 more than 23 million people will die annually from CVDs [1,2]. Chest pain of cardiac origin constitutes approximately half of these cases while other half is secondary to non-cardiac causes [3]. Chest pain of cardiac origin should be assessed earlier to prevent sudden cardiac death which is the most common manifestation of CAD [4].
Acute coronary syndrome (ACS) encompasses a spectrum of CAD, including UA, NSTEMI and STEMI. Recent studies have shown that patients with NSTEMI constitute the majority (54%) of acute MI admitted to the referring hospitals. The diagnosis of ACS is confirmed in most of cases where significant ECG changes such as STEMI and/or increased levels of myocardial markers in plasma are present. However, absences of such abnormalities don’t exclude ACS. Therefore, it is difficult to diagnose the ACS in its early phase [5]. Therefore, early diagnosis and risk stratifications are essential tools to ensure the accurate, timely and cost-effective early management of NSTE-ACS patients [6]. For assessment of patients with confirmed ACS diagnosis, several scoring methods can be used like TIMI, PURSUIT and GRACE etc [7].
The TIMI risk score is derived in a test cohort of patients with NSTE-ACS by selection of independent prognostic variables i.e., age 65 yrs or older, at least 3 risk factors for CAD, prior coronary stenosis of 50% or more, ST-segment deviation on ECG at presentation, atleast 2 angina events in the previous 24 hours, use of acetylsalicylic acid in the previous 7 days and elevated serum cardiac markers. The PURSUIT risk score predicts 30-day risk and incorporates information from early vital signs. The score ranges from 0 to 25, and is comprised of age, sex, worst Canadian Cardiovascular Society angina class in the previous six weeks, heart rate, systolic blood pressure, signs of heart failure and ST depression. The components of the GRACE risk score (range 2 to 372) are age, heart rate, systolic blood pressure, Killip class, cardiac arrest, serum creatinine, ST-segment deviation and cardiac biomarker status [8].
Single-photon emission computed tomography (SPECT) is a nuclear medicine tomographic imaging technique that was developed to evaluate myocardial perfusion imaging (MPI) and is to assess inducible ischemia due to flow limiting coronary stenosis. Images taken during stress (either physiological or pharmacological) and rest injections enable independent assessment of myocardial perfusion with a SPECT Gamma Camera system [9]. The finding on stress images of a perfusion defect in a region that appears normal on rest images (i.e., a reversible defect) is suggestive of myocardial ischemia. The finding on stress images of a perfusion defect that appears identical on rest images (i.e. a fixed defect/ myocardial infarct) could be either an attenuation artifact or an area of MI [10].
Coronary angiography provides unique information on the presence and severity of CAD and therefore remains the gold standard. Angiography should be performed urgently for diagnostic purposes in patients at high risk and in whom the differential diagnosis is unclear [11]. Angiographically, the typical lesion may be divided as:
(i) discrete
(ii) concentric
(iii) readily accessible
(iv) non-angulated segment
(v) smooth contour
(vi) little or no calcification
(vii) subtotal occlusive
(viii) non-osteal in location
(ix) no major branch involvement and
(x) absence of thrombus. ACC/AHA grouped the criteria into three large categories based
(i) low-risk type A lesions (success rate of >85%),
(ii) moderate-risk type B lesions (60% to 85% success rate) and
(iii) high risk type C lesions (<60% of success rate) [12].
Aim of Study
The purpose of this study is to find correlation between diagnostic accuracy of TIMI clinical score and nuclear MPI in non STE-ACS, so that patients can be diagnosed early and prevent further cardiac complications.
Patients and Methods
This cross sectional study was conducted on patients presenting at ER of Abbasi Shaheed Hospital (a tertiary care hospital) with chest pain upto 12 hours post symptoms. The study was conducted in June 2019 to May 2020 including patients with suspected Non- STE-ACS. The minimum required sample size was calculated to be 46 using Epitool online sample size calculator [13]; (for analyzing sensitivity and specificity of myocardial perfusion imaging, K R Branch et al. [14]) at 95% confidence level. However our sample size was increased up to 94 to prevent underpowered statistical analysis.
Inclusion Criteria: Patients of either gender (age > 25 years) presenting within time period upto 12 hours after onset of chest pain (lasting for more than 20 minutes); provisionally diagnosed as Non-STEMI (including low and intermediate risk) or unstable angina (including intermediate and high risk).
Exclusion Criteria: (i) Recently diagnosed STEMI (ii) high risk TIMI score NSTEMI (iii) UA with low risk TIMI score (vi) history of PCI/CABG within 30 days (v) any known renal disease or serum creatinine level ≥ 1.5 mg/dl (vi) hemodynamically unstable patients (vii) patients having chest pain of non-cardiac etiology.
Ninety four (n=94) individual were enrolled for this study who were assessed initially at the time of onset of chest pain (suspicious of having NSTE-ACS), presence of risk factors and previous history of CAD. History questionnaire and form were filled accordingly. Standard ECG were recorded and blood sample were drawn for cardiac biomarker Trop-I (Troponin-I; measured by immune chromatographic assay technique5) and routine labs; this was irrespective of the ECG findings and clinical history. TIMI score was calculated of all enrolled patient on the basis of selected clinical risk score system. The allocated risk score were: 0-2 (low category), score 3-4 (intermediate category) and score 5-7 (high category). We collected data based on positive biomarker results (positive result of cardiac biomarker Trop-I within 2 to 12 hours interval after onset of chest pain diagnosed as “NSTEMI” or negative biomarker result of same period labeled as “UA”.
Stress MPI were performed either physiological (on medical treatment) or pharmacological stress in all patients by administrating 12 ± 2 mCi of technetium-99m Sesta-MIBI/ Myoview® intravenously for further risk stratification as per decisions made by the consultant cardiologist (in group-A after CA when patients were hemodynamically stable and in group-B before CA as all patients were hemodynamically stable). SPECT MPI images were acquired using a dual-head (90o fixed angles) gamma camera (PHILIPS Cardio MD®). We used step-and-shoot acquisition mode with 32 views (each view generally of 40 second per image) separated by 6o (6 degrees) for all SPECT study. Image reconstruction was performed using standard filter back-projection algorithms along with multilevel gated cines images. Perfusion and gated images were evaluated and reported either positive or negative for infarct or ischemia with relevant risk score. Results showing a “discrete perfusion defect” with or without related abnormalities (and considering the history as well) in wall motion and/or thickening were considered “positive”. Rest of other results was considered as “negative”. Quantitative assessment was performed using software QPS-QGS algorithm to obtain all sum scores and total perfusion defect (TPD including ischemic burden or/and size of infarct) for MPI risk scoring. Then Sum stress score was used for MPI risk calculation to predict future hard cardiac events (Score 0-3 = normal, score 4-7 = low risk, score 8-12 = intermediate risk, score >12 = high risk) [15].
Coronary angiography was performed as per standard techniques of hospital protocol. Coronary angiography’s data of patients was collected directly from patients through telephone or indirectly from referred hospital. Significant CAD was reported when lesion was ≥ 50% stenosis of the left main coronary artery or ≥ 70% stenosis in major coronary arteries, including left anterior descending artery (LAD), left circumflex (LCX), and right coronary artery (RCA) or their branches. However, ACC/AHA grouped the lesion criteria into three large categories based (i) low-risk type A lesions, (ii) moderate-risk type B lesions and (iii) high-risk type C lesions [15].
Statistical Analysis
Microsoft Excel spreadsheet (version 2007) was used to enter the relevant data. The statistical analysis was carried out using SPSS (version 17). Sensitivity and specificity of myocardial perfusion imaging were calculated in comparison with TIMI clinical score and keeping coronary angiography as gold standard. All parameters were analyzed by using test for independence. Results were considered significant if the p-value was less than 0.05.
Results
Out of 94 study population, 34 were females and 60 were males. The minimum age limit was 27 years and maximum age limit was 84 years with a mean age of 54.45 years and SD of ±13. Table-1 demonstrates gender, groups and subgroups.
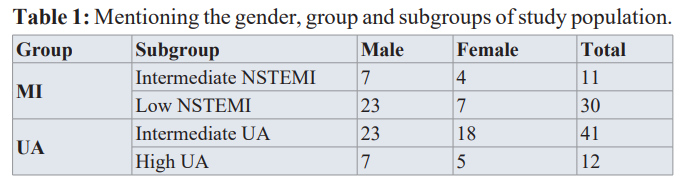
The study population was divided into two groups on the basis of results of cardiac marker, i.e. NSTEMI (group-A: i.e. Positive cardiac biomarkers at any time interval from appearance of symptoms up till 12 hours) and UA (group-B: i.e. Negative cardiac biomarker from appearance of symptoms up till 12 hours). We included all those stable patients who otherwise labeled either low or intermediate risks on clinical ground and likely to get benefit from revascularization therapies with the exclusion of high risk NSTEMI or low risk unstable angina groups. All the patients of group A were further advised CA followed by MPI (Table 1).
MPI in low risk TIMI score (i.e. subgroup A-I; n=30) and intermediate risk TIMI score (i.e. subgroup A-II; n=11) TIMI score patients having diagnosis of NSTEMI were true positive in 13 out of 30 and 5 out of 11 patients, true negative results were obtained in 14 out of 30 and 5 out of 11 respectively. We had obtained 1 false positive and 2 false negative results of MPI in low TIMI score and zero false positive and 1 false negative results of MPI in intermediate TIMI score groups. The sensitivity and specificity of MPI in “low TIMI score NSTEMI” (subgroup A-I) was found to be 92.8% (95% CI 66.13-99.82), 81.25% (95% CI 54.35-95.95); p value< 0.0001 using Chi-square Pearson test) while sensitivity and specificity of MPI in “intermediate TIMI score NSTEMI” (subgroup A-II) was found to be 100% (95% CI 47.82-100) and 80.0% (95% CI 35.88-99.58); p value 0.0057 using Chi-square Pearson test respectively. The data of these patients were also found statistically significant using “CA as gold standard”.
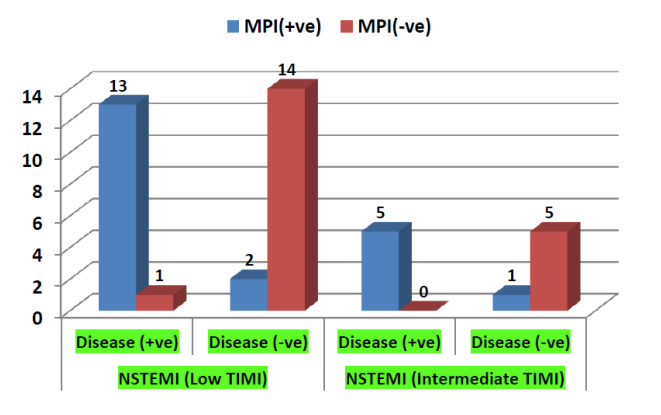
Figure 1: Demonstrated the true positive, true negative, false positive and false negative results of MPI in low and intermediate TIMI patients of NSTEMI.
Similarly in order to minimize neglecting patients who have great suspicious of CAD, we had advised MPI in all those having diagnosis of UA (Group B; n=53) who had intermediate TIMI risk and high TIMI score; they were advised for CA (Figure 1).
MPI in intermediate risk TIMI score (i.e. subgroup B-I; n=41) and high risk TIMI score (i.e. subgroup B-II; n=12) patients having diagnosis of UA were true positive in 13 out of 41 and 7 out of 12 patients, true negative results were obtained in 23 out of 41 and 4 out of 12 respectively. We found 2 false positive and 3 false negative results of MPI in intermediate TIMI score and 0 false positive and 1 false negative results of MPI in high TIMI score groups. The sensitivity and specificity of MPI in “intermediate TIMI score UA” (subgroup B-I) were found to be 86.67% (95% CI 59.54-98.34) and 88.46% (95% CI 69.85-97.55); p value < 0.0001 using Chi-square Pearson test. While sensitivity and specificity of MPI in “high TIMI score unstable angina” (subgroup B-II) were found to be 100% (95% CI; 59.04-100) and 80.0% (95% CI; 28.35-99.49); p value 0.0038 using Chi-square Pearson test. The data of these patients were also found statistically significant using “CA as gold standard” (Figure 2). However, MPI and CA were not performed in low TIMI risk patients of UA as they were advised medical treatment and follow-up. Similarly only CA was performed in high TIMI risk patients of NSTEMI as they need aggressive treatment.
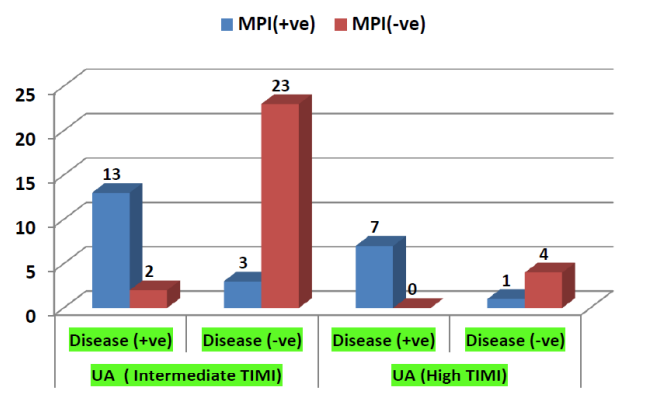
Figure 2: Demonstrated the true positive, true negative, false positive and false negative results of MPI in low and intermediate TIMI patients of UA.
Comparative analysis between TIMI scoring system and MPI
Out of 41 low TIMI patients of NSTEMI group (Subgroup A-I; n=30), MPI showed 15 normal scan, 4 low risk scan but it recognizes 7 intermediate and 4 high risk scan. On performing angiogram, it is found that 16 patients had normal angiogram; 4 reported with low risk angiogram, 6 reported with intermediate patients and 4 reported with high-risk patients were confirmed. In the intermediate TIMI patients of NSTEMI group (Subgroup A-II; n=11), MPI showed 5 normal scan, 2 low risk scan but it recognizes 1 intermediate and 3 high risk scan. Later on CA reported; six as normal CA, 1 with 1ow risk CA, 1 with intermediate risk CA and 3 with high risk CA (Table 02). It was concluded from the comparative analysis between TIMI scoring system and MPI using CA results as gold standard that MPI had provided early detection accuracy rate of 90.91% in intermediate TIMI group while it gave 86.7% accurate rate in low TIMI risk group. These findings are demonstrated in table 2.
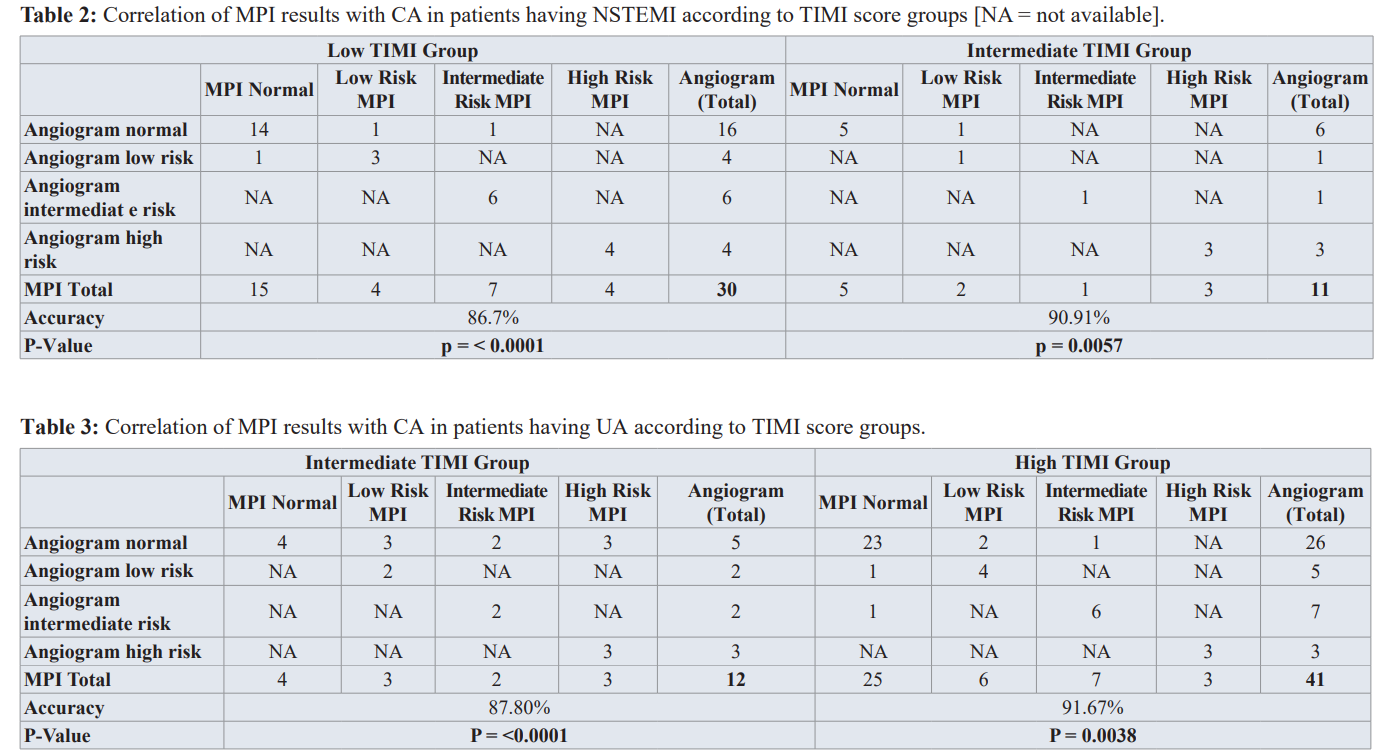
Out of 12 intermediate TIMI patients of UA (Subgroup B-I; n=12), MPI showed 4 normal scan, 3 low risk scan, 2 intermediate and 3 high risk scan. CA detected; five patients as normal CA, 2 as low risk CA, two intermediate CA and three high risk CA. Similarly out of 41 high TIMI risk patients of CA (Subgroup-II; n=41); MPI showed 25 normal scan, 6 low risk scan, 7 intermediate risk scan and 3 high risk scan. Late on CA established; 26 patients as normal CA, 5 as low risk CA, 7 as intermediate risk CA and 3 as high risk CA (Table 3). It was concluded from the comparative analysis between TIMI scoring system and MPI using CA results as gold standard that MPI had provided early detection accuracy rate of 91.67% in high TIMI group while it gave 87.80% accurate rate in intermediate TIMI risk group. These findings are demonstrated in table 3.
Discussion
The demographic data of our study showed mean age of 54.45 years (SD ± 13) while study done by Shaikh M K et al. revealed mean age 60 (SD ± 5.0 years) in Pakistani population [16]. The reason for younger age limit in our population may due to fact that most of our patients had at least 3 or more co-morbidities. We also reported that male gender was more prone to CAD which matched with previous study reported by Iqbal UJ and Suresh et al. for male preponderance [17,18]. It is also postulated in published literature that young female gender implies lower risk for CAD due to estrogen protective effects. This might be a reason that most women with clinical CAD are generally older than men as mentioned by Maas and Appleman [19]. Besides that it was also concluded from the study that there were 3 most important CV risk factors (three or more risk factors n=43; 42%) which were more prone to MI or UA i.e.; hypercholesterolemia, HTN and smoking, followed by diabetes, obesity and family history [20]. Our results also specified the same findings as Chiha et al. Approximately 44% reduction in ACS resulted after modification of these 3 most important cardiovascular risk factors as concluded by Chiha et al. [21].
In this study, we considered TIMI score in all study population to identify low and intermediate risk groups’ patients who still need further investigation prior to confirmation or exclusion for an ACS. It is also found that patients in the high-risk group had a very high prevalence rate of AMI and adverse cardiac events, potentially facilitating selective specialist referral. However, it was reported from our results that even patients with a zero TIMI score, still require further diagnostic testing if used alone as described by Louise et al. [22].
Radionuclide MPI was used as an aid for further diagnostic testing, to improve diagnosis and risk stratification in patients with chest pain and possible ACS. Otto-Langa highlighted the indication of rest MPI as a class I (level A) by the ACC/AHHA/ASNC for the evaluation of myocardial risk in possible ACS patients with a non-diagnostic ECG and initial normal serum markers [23]. We used stress MPI over rest MPI considering the findings of Fesmire et al. [24] that sensitivity and specificity of stress MPI were significantly higher than rest MPI (97% and 88% versus 71% and 73% respectively. In contrast to our study (overall combine sensitivity and specificity: 94.86% and 82.42%), Al Moudi et al. [25] reported the sensitivity of 82% and specificity of 76% for SPECT in detecting CAD. The reason for high sensitivity and specificity in our study is that we included all patients who have already labeled as having NSTE-ACS.
It is revealed from MPI results of our study that patients with diagnosis of NSTEMI, we obtained 3 false positive and 1 false negative patients in low risk TIMI score group and 1 false positive and zero false negative patients in intermediate TIMI score group. Likewise, in-patient with diagnosis of UA, we obtained 4 false positive and 2 false negative patients of intermediate TIMI score group and 1 false positive and 0 false negative patient of high TIMI score group. The reason for false positive test in our study is either from prior MI or due to artifacts secondary to diaphragmatic (mainly in men) and breast (in female) attenuation, resulting in a lower specificity that is also reported by Fathala [15]. On the other hand, considering previous infarcted patient as "false- positive" is not correct; because previous MI is also a main risk factor in patients undergoing assessment for myocardial ischemia so early discharge is not usually appropriate. Kontos et al. [26] also mention that false negative results could be due to balanced ischemia secondary to 3VD or LM because of limitation of SPECT in assessing the relative perfusion. Similar finding was reported by Salerno [27].
The sensitivity and specificity of MPI in case of NSTEMI with low TIMI score was found to be 92.8% and 81.25% while sensitivity and specificity of MPI in case of NSTEMI in intermediate TIMI score NSTEMI was found to be 100% and 80.0% respectively. The sensitivity and specificity of MPI in case of UA with intermediate TIMI score was found to be 86.67% and 88.46% while sensitivity and specificity of MPI in case of UA with high TIMI score was found to be 100%, 80.0% respectively. The data of these patients were also found statistically significant using "CA as gold standard". The overall sensitivity and specificity of MPI was reported for NSTEMI as 96.4% and 80.62% while overall sensitivity and specificity of MPI was reported for UA as 93.33% and 84.23% respectively. The study by Fesmire et al. [24] showed same results like ours combined results (i.e. 93% and 84% versus 96% and 88% respectively).
It was reported from the comparative analysis between TIMI scoring system and MPI using CA results as gold standard in NSTEMI patients that MPI provides early detection accuracy rate of 90.91% in intermediate TIMI group while it produces 86.7% accuracy rate in low TIMI risk group. It was also reported from the comparative analysis between TIMI scoring system and MPI using CA results as gold standard in UA patients that MPI had provided early detection accuracy rate of 91.67% in high TIMI group while it gave 87.80% accuracy rate in intermediate TIMI risk group. Therefore, it was concluded from our study that MPI has remarkably identified more accurately patients who had significant CAD that cannot correctly diagnosed by clinical risk score (TIMI). These results also showed that MPI can be used to further risk stratify those patients for whom the diagnosis of myocardial ischemia is still a concern, despite the absence of definitive proof of MI, and for whom discharge without exclusion of the diagnosis may be risky [28].
It was also revealed from our study that even some self-referral patients who labelled as low TIMI risk and sent for medical follow-up may had significant CAD later on confirmed by invasive CA. In conclusion, it was stated that some high-risk patients with underlying significant CAD afterward diagnosed by CA, may be missed by clinical risk score (TIMI score) or MPI who otherwise labelled as low risk group.
In our study, main primary end points were diagnosis of NSTEMI or UA and evaluation of risk score by MPI using diagnostic CA as standard rather than focused on individual vascular territories followed by intervention. The reason behind it is that we had patients with suspected NSTE-ACS in which we needed detection of CAD as the potential role for a non-invasive imaging (MPI) test to identify those patients who should be referred for invasive testing. Secondly, we wanted to compare MPI with the clinical TIMI risk score that does also not be able to allocate the disease. In conclusion, MPI provides diagnostic as well as prognostic information compared with clinical and stress variables; furthermore, it will reduce the rates of subsequent CA and revascularization when the pre-test probability of disease is relatively low. Thus, it appears that MPI can be used for the triage of patients and act as a “gateway” for appropriate decision regarding early invasive approach or conservative management [29].
Conclusion and Recommendations
Early detection of cardiac diseases is important especially in diabetics as diabetes is a cardiovascular risk equivalent. Hence, early screening for cardiovascular and diabetic complications is essential to prevent progression of diseases [27-30]. This study suggested TIMI score is not as good for exclusion of either infarct or ischemia therefore; MPI is used to identify definite intermediate and high risk patients allowing early referral or intervention for treatment initiation. By more appropriate categorization of all these patients through MPI, CA procedures in low-risk patients can be decrease if accurately applied hence reduced the cost burden through better efficiency. Further studies are required to confirm the findings of our study.
Study Limitations
Our study includes hospital-based population fairly representative of the ER setting and may not necessarily reproduce the results for the general population. Second limitation of our study is that we have less number of patients therefore studies with larger case groups are still required for further evaluation and established identical facts.
References
- World Health Organization. Cardiovascular diseases. WHO Media Centre Fact Sheet. 2015. 317.
- Muhammad SK, Fahim HJ, Tazeen HJ, et al. Knowledge of modifiable risk factors of heart disease among patients with acute myocardial infarction in Karachi, Pakistan: a cross sectional study. BMC Cardiovascular Disorders. 2006; 6: 1-9.
- Claude Lenfant. Chest pain of cardiac and non-cardiac origin. Metabolism: clinical and experimental. 2010; 59: 41-46.
- Zipes Douglas P, Wellens HJJ. Clinical Cardiology: New Frontiers, Sudden Cardiac Death. Circulation. 1998; 98: 2334-2351.
- Achar Suraj A, Kundu Suriti, Norcross WA. Diagnosis of Acute Coronary Syndrome. Am Fam Physician. 2005; 72: 119-126.
- Amsterdam EA, Wenger NK, Brindis RG, et al. AHA/ACC Guideline for the Management of Patients with Non–ST- Elevation Acute Coronary Syndromes. J Am Coll Cardiol. 2014; 64: 2645-2687.
- Backus BE, Six AJ, Kelder JH, et al. Risk Scores for Patients with Chest Pain: Evaluation in the Emergency Dept. Cardiol Review. 2011; 7: 2-8.
- Khalill R, Han L, Jing C, et al. The use of risk scores for stratification of non-ST elevation acute coronary syndrome patients. Exp Clin Cardiol. 2009; 14: 25-30.
- Hung Guang-Uei, Wang Yuh-Feng, Su Hung-Yi, et al. New Trends in Radionuclide Myocardial Perfusion Imaging. Acta Cardiol Sin. 2016; 32: 156-166.
- Dvorak RA, Brown RKJ and Corbett JR. Interpretation of SPECT/CT Myocardial Perfusion Images: Common Artifacts and Quality Control Techniques. Radio Graphics. 2011; 31: 2041-2057.
- Hamm CW, Bassand JP, Agewall S, et al. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. European Heart Journal. 2011; 32: 2999–3054.
- L.W. Klein, R.J. Krone. Angiographic characterization of lesion morphology: are the AHA/ACC and SCAI lesion classifications still useful? Cardiac Interventions Today. 2008; 7: 44-49.
- Hickey GL, Grant SW, Dunning J, et al. Statistical primer: sample size and power calculations—why, when and how? Software: OpenEpi ( http://www.openepi.com ). European Journal of Cardio-Thoracic Surgery. 2018; 54: 4-9.
- Branch KR, Busey J, Mitsumori L, et al. Diagnostic Performance of Resting CT Myocardial Perfusion in Patients with Possible Acute Coronary Syndrome. Am J Roentgenol. 2013; 200: 450-457.
- Fathala A. Myocardial Perfusion Scintigraphy: Techniques, Interpretation, Indications and Reporting. Ann Saudi Med. 2011; 31: 625–634.
- Shaikh MK, Hanif B, Shaikh K, et al. Validation of grace risk score in predicting in-hospital mortality in patients with non ST-elevation myocardial infarction and unstable angina. JPMA. 2014; 64: 807-811.
- Iqbal UJ, Kaleem M, Iqbal N, et al. Frequency of conventional risk factors of myocardial infarction in Gulab Devi chest hospital. Biomedica. 2014; 30: 1-6.
- Suresh K, Devi S A, Badrinath AK, et al. Diagnostic utility of heart type fatty acid binding protein (H-FABP) versus cardiac troponin-I in myocardial Infarction. Int. J Adv Med. 2018; 5: 514-519.
- Maas A.H.E.M, Appelman Y.E.A. Gender differences in coronary heart disease. Netherlands Heart Journal. 2010; 18: 598-602.
- Aziz KMA. Association of Micro-albuminuria with Ischemic Heart Disease, Dyslipidemia and Obesity among Diabetic Patients: Experience from 5 Year Follow up Study of 1415 Patients. Bioenergetics. 2014; 3: 118 (doi:10.4172/2167- 7662.1000118).
- Chiha M, Njeim M, Chedrawy EG. Diabetes and Coronary Heart Disease: A Risk Factor for the Global Epidemic, International Journal of Hypertension. 2012; 1-7.
- Rozenman Y, Gotsman MS. The earliest diagnosis of acute myocardial infarction. Annual Review of Medicine. 1994; 45: 31-44.
- Otto Langa. Acute Coronary Syndromes: Radionuclide imaging in acute coronary syndromes, Coret Vasa. 2014; 354-361.
- Fesmire F.M, Hughes A.D, Stout P.K, et al. Selective dual nuclear scanning in low-risk patients with chest pain to reliably identify and exclude acute coronary syndromes, Annals of Emergency Medicine. 2002; 40: 584–594.
- Moudi M, Sun Z, Lenzo N. Diagnostic value of SPECT, PET and PET/CT in the diagnosis of coronary artery disease. Biomed Imaging Interv J. 2011; 7: 1-9.
- Kontos MC, Jesse RL, Anderson FP, et al. Comparison of Myocardial Perfusion Imaging and Cardiac Troponin I in Patients Admitted to the Emergency Department with Chest Pain. Circulation. 1999; 99: 2073-2078.
- Salerno M, Beller GA. Non-invasive Assessment of Myocardial Perfusion. Circ Cardiovasc Imaging. 2009; 2: 412-424.
- Plein S, Greenwood JP, Ridgway JP, et al. Assessment of non- ST-segment elevation acute coronary syndromes with cardiac magnetic resonance imaging. J Am Coll Cardiol. 2004; 44: 2173-2181.
- Allman KC, Thomson LE J. Prognostic value of myocardial perfusion imaging in patients with known or suspected coronary artery disease. Eur Heart J. 2001; 3: Suppl F5–F7.