Diabetes is a Systemic Disorder: The 'Whole Body' Hypothesis
Author(s): Graham Wilfred Ewing B.Sc*
Mulberry House, 6 Vine Farm Close, Cotgrave, Notts NG12 3TU, Tel: 07885-755847.
*Correspondence:
Graham Wilfred Ewing B.Sc, Mulberry House, 6 Vine Farm Close, Cotgrave, Notts NG12 3TU, Tel: 07885-755847.
Received: 15 January 2021 Accepted: 03 March 2021
Citation: Ewing GW. Diabetes is a Systemic Disorder: The ‘Whole Body’ Hypothesis. Diabetes Complications. 2021; 5(1); 1-8.
Abstract
In 2020 the author was approached by the editorial team of a medical journal, which specialises in Diabetes and Obesity, to compile and submit for publication a summary of his published work, in particular his/the conclusions and papers re diabetes and obesity.
At the outset of this work/research in the period 2003-2007, and the subsequent compilation of >85 peer-reviewed medical papers, the author sought to demonstrate the relationship between sense perception and pathological onset which was considered to be fundamentally important and significant regarding an understanding of how the brain functions and, in particular, how it regulates the autonomic nervous system and/or physiological systems. Diabetes and Developmental Dyslexia provided the two most significant obvious examples because changes of colour perception are recognised to be associated with the onset and progression of these conditions. Moreover, many researchers have sought, unsuccessfully, to develop a precise understanding of this relationship.
The author based this programme of research and publications on ‘the mathematical model of the relationship between sense perception, brain function, the function of the autonomic nervous system and physiological systems, and changes to cellular and molecular biology’ which had been developed by Grakov IG in the period commencing 1981/2 until the prototype system entered the market in 1997, and the end of his research in 2006.
This particular paper focusses upon the fundamental nature of diabetes and obesity. It incorporates and explains the many different aspects of diabetes which often cannot be satisfactorily explained by contemporary biomedicine e.g. that diabetes is a (multi-) systemic disorder which comprises pathological conditions/disorders which occur in the organs in the physiological system which regulates blood glucose; that problems of blood glucose regulation may occur as a result of pathological onset in other adjacent physiological systems e.g. following a hysterectomy; that each pathology may have genetic origins e.g. T1DM, and non-genetic/phenotypic origins e.g. T2DM; that the brain regulates the stable and coherent function of the physiological systems; and that it does so by a biophysical mechanism.
The author singles out suitable references from the peer-reviewed press to support the conclusions made by the author in this programme of published papers, in particular articles re diabetes and obesity, which have been published since 2007.
Keywords
Definition
The author uses the term ‘phenotype’ to refer to processes, which have a predominantly non-genetic character.
Introduction
Medical research can be characterised by its/the pursuit of the ‘silver bullet’ i.e. the one solution which will miraculously cure a particular ailment; however it is very rare that a medical condition is cured by the application of a particular drug or therapy. Perhaps, and arguably, antibiotics represents the best example where a drug can completely remove the cause of an infection yet the use of antibiotics to treat bacterial infection is not completely free from side-effects [1]. Nevertheless, there are often shortcomings with this approach e.g.
- In many cases the drug suppresses the symptomatic consequences and provides relief at least until the drug becomes less effective and the symptoms often re-emerge in ever greater discomfort.
- The application of genetic engineering, ostensibly to correct a single genetic defect, was expected to revolutionise the treatment of genetic conditions yet the effectiveness of such techniques remains significantly below expectations thereby illustrating that the genetic profile is just part of a wider
- It excludes consideration of the stress response i.e., the effect which our exposure to stress has upon the body’s regulated
- There are few instances, if any, where the application of a drug ‘cures’ a particular ailment. In most cases the drug merely suppresses the autonomic response and the presenting symptoms however over time the drugs often become less effective and/ or other symptoms will Consequently, more and more patients become dependent upon a system of healthcare which offers only a partial and temporary solution to their problems.
The etiology of most medical conditions remains poorly defined because most medical conditions are multisystemic, multipathological/polyphenomic and polygenomic i.e. genotype and phenotype exist as comorbidities; therefore any medical tests which are based upon the diagnosis of a single pathological entity must inevitably have significant shortcomings and/or inaccuracies [2] e.g. the diagnosis of T2DM is based upon diagnosis of HbA1c yet there is an extensive range of factors which affect the accuracy of this test including
(i) the prevailing level of insulin,
(ii) the prevailing level of haemoglobin,
(iii) the glycation process produces a range of glycated adducts of which A1c is only one,
(iv) the level/production of the A1c adduct versus other glycated adducts will vary according to circumstances,
(v) the influence of light, pH, levels of minerals, etc,
(vi) pathological onset in other organs and systems e.g. pancreatic cancer, endocrine pathologies, hysterectomy, etc.
Indeed what is it that is being measured in the various biomarker and scanning tests? Is it a particular marker or measure of molecular biology (genotype, phenotype or both), cell biology, organ function, or system function? [3] Is it a measure of their fundamental neurological origins and cause or is it a measure of the biological consequences (see Note 1)? And If we identify a particular genetic abnormality is it scientifically justifiable and safe to assume that correcting a particular genetic defect by genetic engineering will eliminate the genetic problem or trait? [4] Surely this ignores the complexity of gene structure and/or interactions.
This leads us to conclude that many of the identified markers such as the measurement of glycated haemoglobin (HbA1c) are convenient commercial compromises which are not based upon a fundamental and precise understanding of how the body functions and/or of the process which leads to pathological onset and progression.
Note 1: Is the origins of the condition due to changes of the phenomic profile i.e. stress-based (the phenotype); or is it due to factors which influence the genetic profile (the genotype)?
All therapies including drugs, are based upon how the active principle can influence and/or ameliorate the function of the autonomic nervous system yet, although the human body is an intensely and finely regulated entity, a detailed understanding of how the autonomic nervous system functions remains elusive and/ or at [5] or beyond the limits of medical research. Moreover the numbers with diabetes and diabetic complications continue to escalate which indicates that the drugs often do not effect a cure.
Accordingly a significant and comprehensive understanding of how the autonomic nervous system functions and, in particular is regulated, could conceivably reduce: (i) the complexity and cost of screening and treating the patient, and (ii) the political and commercial opportunities for medical research; by its understanding of how the brain functions, how this could be used to screen the patient’s health, and how this could be used to provide more effective treatments for the patient i.e. by adopting such a ‘whole body’ approach [6] which involves modulating brain function in order to address the effect of stress upon the brain (the neural cause), and treating the symptoms (the biomedical consequences). The observation and recognition that stress is experienced through the sensory organs -which some now consider with good reason to be component parts of the brain – may be significant. The subsequent alterations of neural function, arising from changes of sensory input and/or perception, leads to changes to the coherent function of the autonomic nervous system and/or physiological systems [7], and ultimately their manifestation as changes of cellular and molecular biology [8,9] and vice versa. See figure 1.
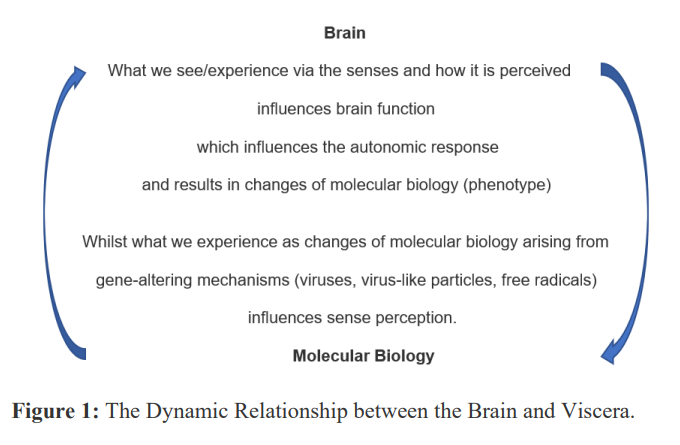
Note 2: changes of molecular biology influence sense perception, which influence brain function and the brain’s subsequent ability to regulate cellular and molecular biology i.e. the dynamic interaction between two data matrices.
In other words what we commonly refer to as the sympathetic response and the parasympathetic response are responsible for changes of cellular and molecular biology which are more commonly known as genotype and phenotype.
If there are changes of molecular biology this must lead inevitably to changes of cellular biology and hence to changes of organ function i.e. in the component parts of the brain and the visceral organs. See figure 2. Moreover our organs are functionally structured in organ systems i.e. which have the express purpose of regulating specific physiological parameters (physiological systems) within set limits e.g. in the case of blood glucose between typically 4 and 8 mmol per litre; but it is at this point that the limits of medical research, in particular of biomedicine, becomes apparent; yet, ironically, a rudimentary knowledge of these physiological systems and/or vital signs is incorporated into a doctor’s training and remains part of a doctor’s medical examination of a patient [5]. So what is the precise nature and structure of these physiological systems and/ or vital signs and what is the mechanism which regulates their function?
Blood Glucose, Blood Pressure, Blood Volume, Blood Cell Content, Breathing, Digestion, Elimination/Urination, pH, Sleep, Body Temperature, Osmotic Pressure, Musculoskeletal/Postural System, Sexual Function. (Origin: I.G.Grakov).
Note 3: The physiological systems are characterised by the use of the terms ‘hyper’ and ‘hypo’ e.g. hyperglycaemia and hypoglycaemia.
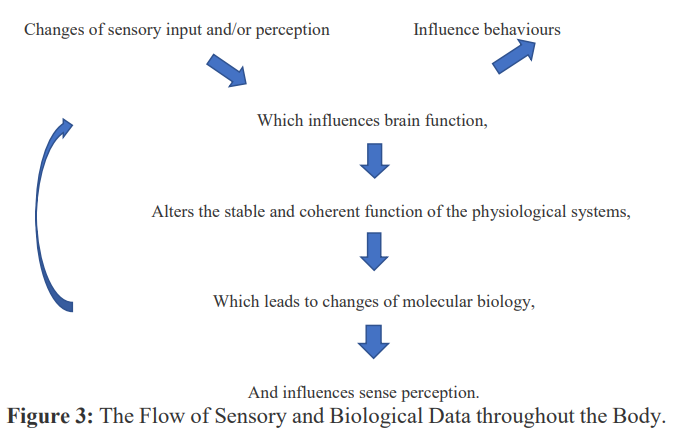
The function of the brain and hence of the physiological systems may be influenced by two significant mechanisms i.e. (i) through the senses and (ii) through molecular biology (genotype and phenotype). See figure 3. Furthermore it is upon recognition of such by eminent neurologists that the European Commission implemented the Human Brain Project [10] i.e. to understand what the brain does and how it does it, to use such knowledge to develop a new generation of cognition-based diagnostics technology with specific emphasis upon identifying the pathological correlates of complex medical conditions such as Alzheimer’s Disease which is often considered to be T3DM, and to understand and adapt with therapeutic effect the multilevel nature of brain function.
Note 4: pathological processes in the blood and peripheral blood vessels continuously release biophotons of light. The blood passes through the retina where it influences colour perception, brain function, and the subsequent regulation of the autonomic nervous system and physiological systems, which is ultimately expressed as pathological onset i.e. changes of molecular biology (genotype and phenotype).
Brain
It is often the case in clinical psychology that behavioural traits in the patient are linked to physiological abnormalities e.g. which could lead to a physiological syndrome such as depression [11]. In an editorial in The Psychologist Zander Wedderburn, former President of the British Psychological Society, spoke about ‘the onward march of neuroscience into psychology’s midst’ thereby emphasising his recognition that traits which have been historically considered to have psychological origins are increasingly recognised to have pathophysiological origins i.e. some may be psychosomatic and others somatic depending upon the level of brain function.
The brain receives sensory input via the sensory organs in which the precise perception of sensory input is influenced by our biology. For example (i) what we see and, in particular our perception of colour, is influenced by our molecular biology (and comprises an estimated 85% of sensory input) and; (ii) what we hear and, in particular our perception of sound, is also influenced by our molecular biology. In patients with diabetes the onset and progression of the condition influences what we see/perceive [12], hear [13], and our perception of taste [14], smell [15,16], touch [17], our vocal abilities [18,19], memory [20], function of the central nervous system [21], etc.
The precise mechanism by which the brain experiences and interprets sensory input, and the intensity of the experience e.g. the greater the sound and the frequency, varies according to the nature of the sensory experience e.g. whether sight is the dominant sense in a particular situation, or whether sound is the dominant sense, or whether other senses are dominant. If sight is the dominant mechanism the passage of biophotons (via the retina and optical nerve) influences the function of the amygdala, hippocampus, lateral geniculate nucleus, and hypothalamus where it influences the expression of endocrine hormones [22] and thereby influences the function of the autonomic nervous system including physiological systems [23]; whereas if hearing is the dominant mechanism the passage of neural stimuli (via the ear and vagus nerve) passes through similar organs (involving the medial geniculate nucleus, arcuate nucleus, etc) although not necessarily in the same sequence, or with the same timing, where it influences the function of the hypothalamus and ultimately the expression of endocrine hormones [22-26]. See Figure 4.
Note 5: If the sensory experience(s) are experienced via a different mechanism then the brain must receive and process these signals at slightly different rates and times. For example explaining how bacterial infections e.g. external or internal otitis; which can often be treated using antibiotics; may lead to problems of sensory perception and coordination (sensory synaesthesia) [27] and thereby influence the function of the autonomic nervous system. The amygdala is characterised by its role in the flight or fight response i.e. the biological correlates of the flight and fight response; and the hippocampus by their role in the consolidation of short-term memories and their subsequent incorporation and consolidation into long-term memory/cortical structures.
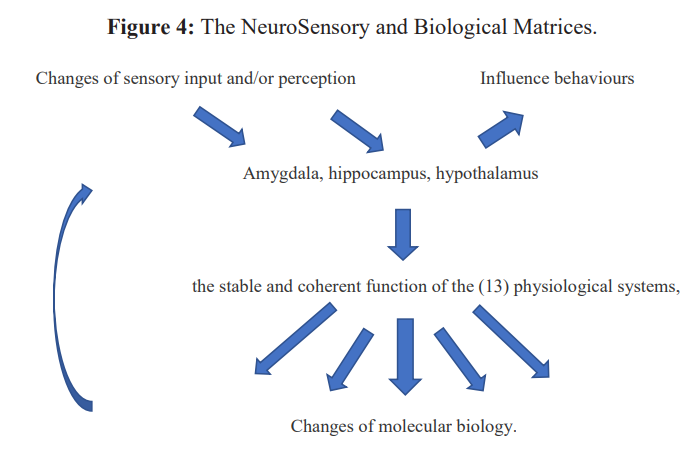
Note 6: the processing of sensory data via the brain influences the coherent function of the physiological structures which regulate the body’s core physiological parameters and/or vital signs. The complex biological consequences of this process subsequently influence brain structures and function.
Neural Regulation of Systemic Stability
This is significant because the endocrine organs: the thyroid, pituitary and adrenal glands are components in each of the organ networks which have a physiological and/or functional capability i.e. in the case of diabetes ‘the regulation of blood glucose levels’; which explains the adoption of terms such as HPA-axis to explain the relationship between the brain and visceral organs yet also illustrates a lack a precise understanding of the nature or function of this relationship. Moreover, biomedicine routinely uses terminology - ‘hyper’ and ‘hypo’ - to highlight the regulation of systemic parameters between high and low limits [28] and which demonstrates the characteristics of a neurally regulated physiological system.
A closer examination of sense perception in the diabetic reveals that the diabetic patient’s sleep is often dysfunctional; that disorders in organs other than the pancreas influence systemic parameters [29,30] including but not limited to blood glucose levels; that feelings of hunger, appetite and satiety are dysfunctional in the diabetic patient; that stress leads to an inflammatory response [31] and influences the systemic stability of the body’s physiological parameters including blood glucose [32], blood pressure [33], pH [34], sleep [35] and other systemic parameters; that the therapeutic application of insulin in the T1DM patient does not prevent the onset and/or progression of further diabetic comorbidities [36]; and that insulin is released by the pancreas in a regular pulsed/ pulsatile sequence [37] which is indicative of neural regulation [38] of this mechanism.
The regulation of blood glucose levels is often influenced by pathological deviations in the pancreas which can have genetic and phenotypic origins; but may also be influenced by pathological onset in other the organs in the system which regulates blood glucose e.g. the endocrine glands; pathological onset in other adjacent physiological systems e.g. the system which optimises sexual function; and systemic imbalance in the brain/whole organism due to stress.
The Pathological Correlates of Stress
To address this issue, we first need to address the following question: ‘What is stress?’ The body’s function can be influenced by many stressors. Stress influences the body’s function in many ways. Although most of us consider stress to be predominantly psychological e.g. due to a bereavement, divorce, etc [39-41]; it is manifest as a series of molecular correlates i.e. changes which accompany altered systemic stability including, but not limited to, increased levels of intercellular acidity (most likely due to dysfunction of the upper digestive tract) in particular low levels of essential minerals incl. magnesium' [41]. Exposure to stress leads initially to increased plasma levels of Mg and increased urinary excretion of Mg [42], increased levels of oxidative stress and/or damage to DNA (and, in particular, increased levels of 8-oxo-7,8- dihydroguanine which is associated with the onset of free radical reactions) [43], sleep deprivation [44], loss of bone density [45], etc. Magnesium modulates the access of corticosteroids to the brain [46], plays an important role in synaptic plasticity, is involved in long-term potentiation (LTP) and the long-term depression (LTD) of synaptic transmission, etc. In other words, a deficiency of magnesium stimulates the sympathetic response.
It is the effect of the stress experience upon the brain (and how the subsequent alterations to the brain and its function subsequently regulates the autonomic nervous system and physiological systems,) which leads to alterations of cellular and molecular biology throughout the body i.e. in the case of diabetes, the molecular and biophysical correlates of appetite, hunger and satiety [47]. Pathological onset influences the pulsatile release of insulin. Whereas under normal circumstances insulin is released every 3-4 minutes, under pathological conditions the release of insulin takes much longer.
Stress is commonly experienced as an acidifying process in which the amounts of acidic moieties produced in the stomach, lungs, etc; are above or below normal levels and subsequently alters the conformation, structure, energetics and reactivity of many of the body’s proteins and enzymes with the result that pathological onset occurs. It is what biomedicine has referred to variously as: the sympathetic nervous system [48] and/or phenotype, and the parasympathetic response and/or genotype. Depending upon your viewpoint and/or circumstances it can be considered to be psychological or psychophysiological.
The cognitive and pathological correlates of stress are interpreted by the brain, compared with short and long-term memories, and subsequently influence the function of the hypothalamus which regulates the release of corticotrophin-releasing hormone (CRH) which acts upon the pituitary gland to secrete adrenocorticotrophin hormone (ACTH) and subsequently influences the adrenal glands to release cortisol and other related adrenocortical hormones into the blood. To further complicate matters exposure to light stimulates the expression or secretion of pituitary hormones [49] incl. Melatonin and suppresses cortisol levels [50].
There are several precedents which support these conclusions:
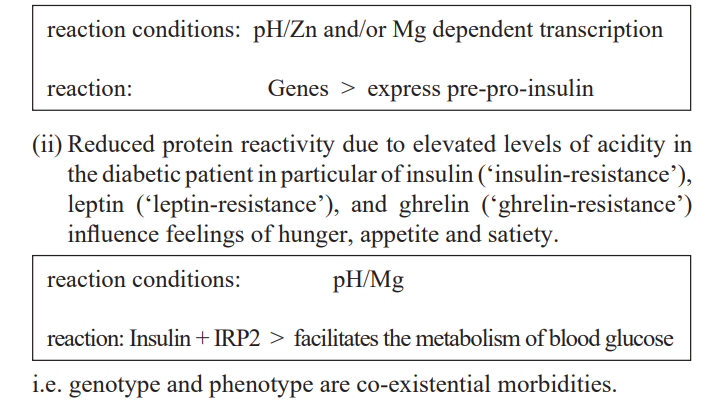
- 1.The levels and/or rate of genetic expression of pre-pro-insulin and subsequently of insulin.
- Changes to the genetic structure/conformation influence the genetic expression of pre-pro-insulin [51].
- Changes to the structure, conformation and activity of transcriptase(s) e.g. due to elevated acidity and hence of reduced levels of essential minerals, in particular Mg and Zn [52,53]; influences the rate of genetic expression.
- Leptin resistance (akin to insulin resistance in T2DM results in an inability to detect satiety despite high energy stores and high levels of leptin [54].
- Ghrelin is often associated with appetite and increase body weight by stimulating triggering the arcuate nucleus [55] in the
- Reduced sensitivity of ‘gastric vagal afferents’; produces a flow of information from the viscera to the brain, autonomic nervous system and/or central nervous system; become increasingly insensitive to gastric distension [56]; and increases the expression of ghrelin [57].
- The reaction of insulin with its receptor protein is a Magnesium dependent reaction - and Magnesium availability is pH dependent [58] - therefore any factors which alters the prevailing pH must inevitably influence the rate at which this occurs and/ or leads to the accumulation of body fat.
- The storage of insulin in the pancreas is a Zinc dependent reaction-and Zinc levels and/or bioavailability are pH dependent [59] therefore any factors, which alter the prevailing pH, must inevitably influence the availability of Zinc and subsequently the storage and/or supply and/or availability of insulin.
- Metformin, the most widely used ‘drug’ for the treatment of T2DM is eliminated from the body almost completely unmetabolized [60] therefore its mode of action cannot involve its metabolism and cannot therefore be pharmacological. This occurs because Metformin is not a ‘drug’. It is a biological buffer [61] which influences/regulates pH.
- 3.Increased capacity of the stomach due to increased consumption of food and drink which leads to obesity and is often corrected via bariatric surgery [62], which effectively reduces stomach capacity, or by lifestyle changes including exercise and diet/ dietary control [63].
What is the Mechanism, which regulates the Body’s Function?
As outlined above, the body is a complex biofeedback system, which involves a dynamic relationship between the brain, which receives and interprets cognitive input, and the visceral organs. The brain regulates and fuels the body’s complex function. Moreover the vast majority of the body’s behaviours – seeking and eating food and drink, seeking warmth, sexual activity, sleep – are devoted to supporting the body’s continued existence; however pathophysiology alone is unable to explain the complex mechanisms which govern how this complex regulatory mechanism functions. The observation that changes of molecular biology influences cellular biology, and that changes of cell biology influences organ biology, appears unable to explain how the organs function in coherent organ networks (physiological systems) function. If so, what is the mechanism by which these organs function together?
The evidence suggests that the brain functions as a biophysical entity which uses a complex mechanism, involving sensory input and frequency, to regulate the stable and/or coherent (in a ‘best-fit’ manner) function of the physiological systems [64,65]
In summary
The arguments set out in this text are supported by a series of papers, which have been peer-reviewed by reviewers in the various journals. Each of these papers was compiled by the author in a logical sequence in order to build the scientific justification for Grakov’s mathematical model which are based upon the relationships set out in this paper i.e. Grakov’s mathematical model of the relationship between sense perception, brain function, the autonomic nervous system and physiological systems, and cellular and molecular biology. It queries whether clinical medicine on its own is fundamentally limited in its scope and hence is unable to solve the problem of diabetes, its diagnosis and treatment.
The author’s bibliography sets out a fundamental and logical reappraisal of the etiology of diabetes and obesity which, it is argued, cannot be solved by the solely biological or pharmacological approach which excludes any consideration of the causal, psychological and/or psychophysiological mechanisms. This includes a series of articles illustrating how the technique, upon which Grakov’s mathematical model is based, performs as a diagnostic and/or screening modality [8,29,66-69]; how it contributes to a better and inclusive understanding of the relationship between diabetes and diabetic comorbidities including heart disease(s) [70], depression/mental health [71], cancer [72], Alzheimer’s Disease [73], the Aging Process [74] and CoVid-19 [75- 77]; and how it performs as a therapeutic modality [78-80] which initial studies have illustrated is ca 75-96% effective depending upon the nature and progression of the conditions being treated.
Acknowledgement
The author thanks the internationally eminent and respected Dr S.H.Parvez, former Head of the CNRS Neuroendocrine Unit, former Asst Editor NeuroEndocrine Letters/currently Deputy Chief Editor, former Editor-in-Chief Activitas Nervose Superiore Rediviva (the former Journal of Neurocognitive Research), and former Editor-in-Chief Biogenic Amines for his continuing support and encouragement.
References
- Gaynes Preserving the Effectiveness of Antibiotics. JAMA. 2010; 303: 2293-2294.
- Ewing A Discussion of the Current Limitations of Diabetes Etiology. EC Endocrinology and Metabolic Research RCO. 2019; 1: 11-13.
- Ewing The Limitations of Big Data. The Limitations of Big Data in Healthcare. MOJ Proteomics Bioinform. 2017; 5: 1-4.
- Ewing GW. The Interpretation of Genetic Data - Considering the Effect of Changes to Gene Conformation -- If the facts don’t support the theory, change the theory – how does this contribute to understanding Diabetes? J. Genet. Disor. Genet. 2017; 6: 1-4.
- https://www.msdmanuals.com/en-gb/home/brain,-spinal-cord,-and-nerve-disorders/autonomic-nervous-system-disorders/overview-of-the-autonomic-nervous-system
- Ewing The Future of Medicine: Biomedicine or Neuroscience? Insights in Biomedicine 2016; 1: 14-17.
- Ewing GW, Ewing EN. Cognition, the Autonomic Nervous System and the Physiological Biogenic Amines. 2008; 22: 140-163.
- Ewing GW, Parvez SH. The Dynamic Relationship between Cognition, the Physiological Systems, and Cellular and Molecular Biochemistry: a Systems-based Perspective on the Processes of Pathology. Act. Nerv. Super. Rediviva. The Journal for Neuro Cognitive 2010; 52: 29-36.
- Christensen JS, Wild H, Kenzie ES, et al. Diverse Autonomic Nervous System Stress Response Patterns in Childhood Sensory Front. Integr. Neurosci. 2020; 14: 6.
- https://www.humanbrainproject.eu/en/
- Won E, Kim Y-K. Stress, the Autonomic Nervous System, and the Immune-kynurenine Pathway in the Etiology of Curr. Neuropharmacol. 2016; 14: 665-673.
- Kurtenbacha A, Schiefera U, Neub A, et Preretinopic changes in the colour vision of juvenile diabetics. British Journal of Ophthalmology. 1999; 83: 43-46.
- Gupta S, Eavy RD, Wang M, et al. Type 2 diabetes and the risk of incident hearing Diabetologia. 2019; 62: 281-285.
- Neiers F, Canivenc-Lavier M-C, Briand What Does Diabetes “Taste” Like? Curr. Diab. Rep. 2016; 16: 49.
- Reinhart Early Detection of Diabetic Ketoacidosis by Breathalyzer in a Sailor Reporting for Duty. Mil.Med. 2019; 184: e951-e952.
- De Moraes AG, Surani S. Effects of diabetic ketoacidosis in the respiratory World J.Diabetes. 2019; 10: 16-22.
- Rayman G, Vas PR, Baker N, et The Ipswich Touch Test. A simple and novel method to identify inpatients with diabetes at risk of foot ulceration. Diabetes Care. 2011; 34: 1517-1518.
- Hamdan A-L, Jabbour J, Nassar J, et al. Vocal characteristics in patients with type 2 diabetes European Archives of Oto-Rhino-Laryngology. 2012; 269: 1489-1495.
- Maddaloni E, Pozzilli Getting it right for people with LADA. Diabetes Voice. 2014; 59: 31-32.
- Sommerfield AJ, Deary IJ, McAulay V, et al. Short-Term, Delayed, and Working Memory Are Impaired During Hypoglycemia in Individuals With Type 1 Diabetes Care. 2003; 26: 390-396.
- Malone Diabetic Central Neuropathy: CNS Damage Related to Hyperglycemia. Diabetes. 2016; 65: 355-357.
- Ising H, Braun C. Acute and chronic endocrine effects of noise: Review of the research conducted at the Institute for Water, Soil and Air Hygiene. Noise Health. 2000; 2: 7-24.
- Jansen AS, Nguyen XV, Karpitsky V, et Central command neurons of the sympathetic nervous system: basis of the fight- or-flight response. Science. 1995; 270: 644-646.
- Ortiga-Carvalho TM, Chiamolera MI, Pazos-Moura CC, et Hypothalamus- Pituitary-Thyroid Axis. Compr. Physiol. 2016; 6: 1387-1428.
- Ising H, Babisch W, Kruppa B. Noise-Induced Endocrine Effects and Cardiovascular Risk. Noise and Health. 1999; 1: 37-48.
- Lockett MF. Effects of Sound on Endocrine Function and Electrolyte Excretion. Physiological Effects of Noise. 1970; 21-41.
- Ewing GW, Parvez SH. The Influence of Pathologies upon Sensory Perception and Sensory Coordination in Children with Developmental Dyslexia and Learning Disorders: A Unified Theory of Developmental Dyslexia. N Am J Med Sci. 2012; 4: 109-116.
- Ewing Grakov IG. A Further Review of the Genetic and Phenotypic Nature of Diabetes Mellitus. Case Reports in Clinical Medicine. 2013; 2: 538-553.
- Ewing GW, Parvez The Multi-systemic Nature of Diabetes Mellitus: genotype or phenotype? N.Am.J.Med.Sci. 2010; 2: 444-456.
- Ewing GW. The ‘Biology of Systems’ or the ‘Systems of Biology’: Looking at Diabetes from the Systemic International Journal of Systems Biology. 2013; 4: 45-56.
- Cameron AR, Morrison VL, Levin D, et al. Anti-Inflammatory Effects of Metformin Irrespective of Diabetes Status. Circ. 2016; 119: 652-665.
- Ewing GW, Parvez Mathematical Modeling the Systemic Regulation of Blood Glucose: ‘a top-down’ Systems Biology Approach. NeuroEndocrinology Letters. 2011; 32: 371-379.
- Ewing Mathematical Modeling the Neuroregulation of Blood Pressure using a Cognitive Top-down Approach. N.Am.J.Med.Sci. 2010; 2: 341-352.
- Ewing The Regulation of pH is a Physiological System. Increased Acidity alters Protein Conformation and Cell Morphology and is a Significant Factor in the onset of Diabetes and other common pathologies. The Open Systems Biology Journal. 2012; 5:1-12.
- Ewing What is the function of the Brain? What does it do and how does it do it? It functions as a Neuroregulator, which continuously regulates the Autonomic Nervous System and Physiological Systems, and enables us to Recognise that Sleep Exhibits the Characteristics of a Neurally Regulated Physiological System. J.Neurol.Psychol. 2016; 4: 9.
- Long AN, Dagoco-Jack The Comorbidities of Diabetes and Hypertension: Mechanisms and Approach to Target Organ Protection. J.Clin.Hypertens. 2011; 13: 44-251.
- Hellman Pulsatility of insulin release – a clinically important phenomenon. Ups.J.Med.Sci. 2009; 114: 193-205.
- Osundiji MA, Lam DD, Shaw J, et al. Brain glucose sensors play a significant role in the regulation of pancreatic glucose- stimulated insulin Diabetes. 2012; 61: 321-328.
- Seelig MS. Consequences of magnesium deficiency on the enhancement of stress reactions; preventive and therapeutic J.Amer.Coll.Nutr. 1994; 13: 429-446.
- Henrotte JG, Plouin PF, Levy-Leboyer C, et al. Blood and urinary magnesium, zinc, calcium, free fatty acids, and catecholamines in type A and type B subjects. J.Amer.Coll. 1985; 4: 165-172.
- James Magnesium: an emerging drug in anaesthesia. Brit. J.Anaesth. 2009; 103: 465-467.
- Murck Magnesium and affective disorders. Nutr. Neurosci. 2002; 5: 375-389.
- Radak Z, Boldogh I. 8-oxo-7,8-dihydroguanine: Link to gene expression, aging and defense against oxidative stress. Free Biol. Med. 2010; 49: 587-596.
- Omiya K, Akashi YJ, Yoneyama K, et al. Heart-rate response to sympathetic nervous stimulation, exercise, and magnesium concentration in various sleep conditions. Int.J.Sport Nutr. Exercise 2009; 19: 127-35.
- Suarez-Bregua P, HGuerrero PM, Rotllant Stress, Glucocorticoids and Bone: A Review From Mammals and Fish. Front Endocrinol (Lausanne). 2018; 9: 526.
- Billard Ageing, hippocampal synaptic activity and magnesium. Magnes. Res. 2006; 19: 199-215.
- Ahima RS, Antwin Brain regulation of appetite and satiety. Endocrinol. Metab. Clin. North Am. 2008; 37: 811- 823.
- Pan H, Guo J, Su Advances in understanding the interrelations between leptin- resistance and obesity. Physiology & Behaviour. 2014; 130: 157-169.
- Slominski AT, Zmijewski MA, Plonka PM, et al. How UV Light Touches the Brain and Endocrine System Through Skin, and Endocrinology. 2018; 159: 1992-2007.
- Kostoglou-Athanasssiou I, Treacher DF, Wheeler MJ, et al. Bright light exposurfe and pituitary hormone secretion. Clin. (Oxf). 1998; 48: 73-79.
- Pierce SB, Costa M, Wisotzkey R, et al. Regulation of DAF- 2 receptor signaling by human insulin and ins-1, a member of the unusually large and diverse C. elegans insulin gene Genes & Dev. 2001; 15: 672-686.
- Cousins A role of zinc in the regulation of gene expression. Proceedings of the Nutrition Society. 1998; 57: 307-311.
- Haase H, Mazzatti DJ, White A, et Differential Gene Expression after Zinc Supplementation and Deprivation in Human Leukocyte Subsets. Mol.Med. 2007;13: 362-370.
- Myers MG, Leibel RL, Seeley RJ, et al. Obesity and Leptin Resistance: Distinguishing Cause from Trends Endocrinol. Metab. 2010; 21: 643-651.
- Dickson SL, Leng G, Robinson IC. Systemic administration of growth hormone-releasing peptide activates hypothalamic arcuate Neuroscience. 1993; 53: 303-306.
- Page AJ, Slattery JA, Milte C, et Ghrelin selectively reduces mechanosensitivity of upper gastrointestinal vagal afferents. American Journal of Physiology. Gastrointestinal and Liver Physiology. 2007; 292: G1376-1384.
- Ewing GW. A Different Perspective on Diabetes & Obesity – what it is and how it can be Case Reports in Clinical Medicine. 2018; 7: 269-287.
- Gommers LMM, Hoenderop JGJ, Bindels RJM, et Hypomagnesemia in Type 2 Diabetes: A Vicious Circle? Diabetes. 2016; 65: 3-13.
- Yang Zinc and insulin in pancreatic beta-cells. Endocrine. 2014; 45: 178-189.
- Li Gong, Srijib Goswami, Kathleen Giacomini, et al. Metformin pathways: pharmacokinetics and pharmacodynamics. Pharmacogenet. Genomics. 2012; 22: 820-827.
- Ewing GW. Is Metformin a Drug or a Buffer and Why is this Significant? Further evidence that the brain Regulates the Autonomic Nervous System, in particular prevailing levels of Intercellular pH. Endoc. Diabetes and Metab. Journal. 2018; 2: 1-9.
- Wolfe BM, Kvach E, Eckel Treatment of Obesity: Weight Loss and Bariatric Surgery. Circ. Res. 2016; 118: 1844-1855.
- Hallberg SJ, Gershuni VM, Hazbun TL, et Reversing Type 2 Diabetes: A Narrative Review of the Evidence. Nutrients. 2019; 11: 766.
- Ewing GW. A Theoretical Framework for Photosensitivity: Evidence of Systemic Journal of Computer Science and System Biology. 2009; 2: 287-297.
- Ewing GW, Parvez SH, Grakov Further Observations on Visual Perception: the influence of pathologies upon the absorption of light and emission of bioluminescence. The Open Systems Biology Journal. 2011; 4: 1-7.
- Ewing A Comparison of the Diagnostic Scope of Biomarker techniques, Genetic Screening and Virtual Scanning. Immunology, Endocrine & Metabolic Agents in Medicinal Chemistry 2013; 13: 35-45.
- Ewing GW, Duran JC. A Report of the Ability of Strannik Virtual Scanning to Screen the Health of a Randomly Selected Cohort of Enliven: Neurol Neurotech. 2016; 2: 001.
- Ewing GW, Grakov IG, Mohanlall R, et al. A Clinical Study Report and Evaluation of the Ability of Strannik Virtual Scanning to Screen the Health of a Randomly Selected Cohort of 50 J. Neurophysiol. Neurol. Disord. 2017; 4: 1-12.
- Ewing GW, Parvez SH. Diabetes is a Complex Neurological, Multisystemic, Multipathological and Polygenomic disorder: Use of Strannik Software as an Effective Modality to Illustrate its J. Neurol. Psychol. 2019; 7: 14.
- Ewing GW, Ewing EN. Computer diagnosis in cardiology. Am.J.Med.Sci. 2009; 1: 152-159.
- Ewing How Disruptive Solutions Could Improve the Prevailing Healthcare Paradigm. A Novel Perspective Regarding the Treatment of Mental Health Conditions: the Strannik Mathematical Model. J.Clin.Cases Rep. 2019; 3: 89- 114.
- Ewing GW. Using Artificial Intelligence to Simulate Brain Function, Enhance the Etiology of Diabetes and Cancer, and more Precisely, Effectively and Remotely Screen and Treat the Journal of Diabetes and its Complications. 2020; 4:1-8.
- Ewing GW, Parvez The Multisystemic Origins of Alzheimer’s Disease. J.Aging Sci. 2020; 8: 226.
- Ewing GW. The Neurological, Multisystemic, PolyGenomic and Multipathological Basis of Aging (the ‘Autonomic’ Hypothesis). Neurol.Neurobiol. 2020; 6.
- Ewing GW. Issues which Influence the Etiology of CoVid-19 infection: a Proposed Treatment Protocol based upon optimising the autonomic and immune Health Education & Public Health. 2020; 3: 290-295.
- Ewing GW. SARS-COV-2: Learning the Lessons from our A Critical and personal Review. Asian Journal of Pharmacy, Nursing & Medical Sciences. 2020; 8: 42-48.
- Cruise AB, Grimes T, Peng Li, et Metformin use is Associated with Reduced Mortality in a Diverse Population with CoVid-19 and Diabetes. Front. Endocrinol. 2021.
- Grakov Strannik Diagnostic and Treatment System: a Virtual Scanner for the Health Service. Minutes of Meeting No. 11 of the Praesidium of the Siberian of the Academy of Medical Sciences of the USSR (AMN) held in Novosibirsk. 1985.
- http://www.montaguehealthcare.co.uk/files/Vysochin/pdf
- Grakov I G, Graham Ewing, Mohanlall R, et al. A summary or meta-analysis of data regarding the use of Strannik Virtual Scanning as a screening modality for Asian Journal of Pharmacy, Nursing and Medical Science. 2017; 5: 55-71.