Double Valve Replacement in a Patient with Severe Rheumatic Heart Disease and Acute Decompensated Heart Failure
Author'(s): Binu R Abraham MD, Megan E Atkinson MD, Sandeep Markan MD, and Yi Deng MD*
Baylor College of Medicine, Department of Anesthesiology, Baylor Plaza, MSC 120, Houston, USA.
*Correspondence:
Yi Deng, MD Baylor College of Medicine, Department of Anesthesiology, Baylor Plaza, MSC 120, Houston, TX, USA, Tel:410-227-5358; Fax: 713-873-2867; E-mail: yd1@bcm.edu.
Received: 05 July 2018; Accepted: 01 August 2018
Citation: Binu R Abraham, Megan E Atkinson, Sandeep Markan, et al. Double Valve Replacement in a Patient with Severe Rheumatic Heart Disease and Acute Decompensated Heart Failure. Anesth Pain Res. 2018; 2(2): 1-3.
Abstract
Advanced rheumatic heart disease (RHD) with end stage sequelae is rarely seen in the United States. We report a complex case of a patient with advanced RHD complicated by Tricuspid stenosis, tricuspid regurgitation, mitral stenosis, and pulmonary hypertension in the setting of acute heart failure who undergoes urgent double valve
replacement surgery. There are many notable complex interactions of the pathologies in patients with RHD who need to go on cardiac bypass.
Keywords
Introduction
Rheumatic heart disease (RHD) is responsible for 250,000 global deaths annually, and it represents one of the most common causes of cardiac morbidity amongst young people. Global incidence is estimated at 300,000 to 350,000 per year with a great deal of variation by geographic region. Approximately 15.6-19.6 million people carry the diagnosis by traditional diagnostic criteria. It is the leading cause of heart failure in children and young people worldwide [1]. RHD is typically preceded by Group A strep pharyngitis leading to rheumatic fever, during which cardiac inflammation of the valvular endocardium is likely to occur through antigenic mimicry. Early signs include valvulitis, pericarditis, and very rarely, myocarditis [2]. Subsequent damage from recurrent infectious episodes leads to a majority of the cardiac pathology, with the peak of RHD cases presenting in the age range from 20-50. Mortality in regions without access to medical care can reach 20%. In early stages of the disease, mitral valvular incompetence is compensated for by left atrial and left ventricular dilation. Tricuspid and aortic regurgitation also often occur in concert with mitral regurgitation.
Despite its prevalence worldwide, advanced rheumatic heart disease with end-stage sequelae is rarely seen in the United States. We report a complex case of a patient with advanced RHD in acute heart failure who underwent urgent double valve replacement surgery.
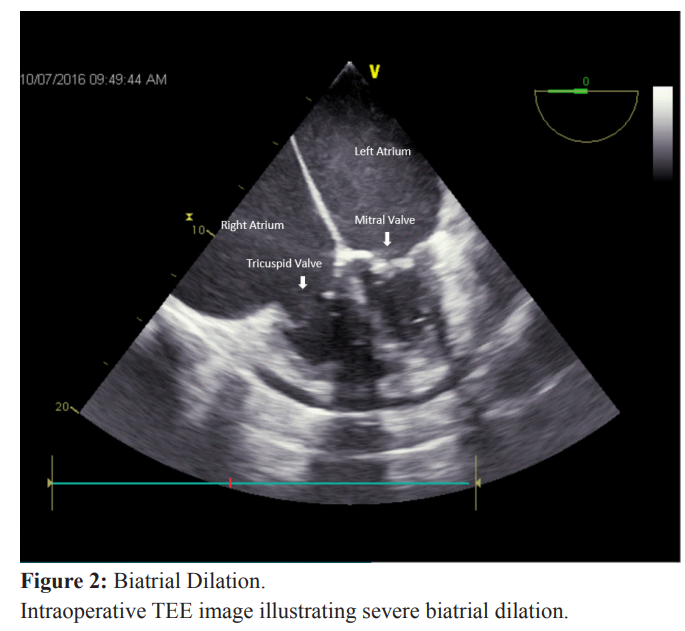
A 69-year-old female with advanced RHD and severe mitral stenosis (MS) complicated by severe pulmonary hypertension (pHTN), and severe tricuspid stenosis (TS) with regurgitation (TR) presented to hospital in acute heart failure secondary to urosepsis. She developed respiratory failure requiring mechanical ventilation and cardiorenal syndrome requiring continuous dialysis. Despite optimal medical management and a failed attempt at balloon valvuloplasty, she continued to deteriorate with increasing vasopressor requirements. A decision was made to attempt double valve replacement surgery despite calculated mortality risk of >50%. Intraoperative transesophageal echocardiogram (TEE) showed classic “hockey-stick” pattern of restricted leaflet movement for both the mitral and tricuspid valves, biventricular failure, large pericardial effusion, and enormously dilated left and right atria (area > 90 cm2) with intra-operative spontaneous echo contrast due to longstanding stenotic valves (Figures 1 and 2).
After sternotomy, a massive right atrium was encountered which comprised the entire anterior surface of the heart. Aortic and venous cannulation proceeded in standard fashion albeit with great surgical difficulty. The mitral and tricuspid valves were sequentially replaced with bioprosthetic valves on cardiopulmonary bypass (CPB). The patient was weaned off CPB methodically, requiring infusions of epinephrine, norepinephrine, vasopressin, and milrinone, in addition to intra-aortic balloon pump support. Total bypass time was 251 minutes. Post-bypass TEE revealed mild regurgitant jet in the mitral valve and a well-functioning tricuspid valve. The patient demonstrated gradual recovery of cardiac function in the intensive care unit postoperatively and was eventually weaned off all vasopressor support 17 days after surgery

RHD is exceedingly rare in the United States and typically only affects the mitral and aortic valves [3]. Our patient exhibited severe MS, TS, TR, and pHTN which proved extremely challenging for surgery. Multiple management decisions had to be made perioperatively. As early as the 1950s, clinicians have noted the myriad of issues that can complicate general anesthesia for an RHD patient [4]. MR is also the most common overriding pathology, as opposed to MS as seen in our patient [5].
Pulmonary HTN is a noted cause of perioperative morbidity and mortality as pertains to cardiac surgery. Bypass itself can worsen pHTN acutely due to the release of inflammatory mediators from pulmonary endothelium, exacerbating any previous predilection to hypoxia [6]. The TR also routinely encountered in such patients is often a result of RV dilation, secondary to pHTN, which in turn is a result of MV stenosis. Surgical correction of TR in patients with pHTN carries increased risk of mortality as the RV loses its “release valve” post-correction, resulting in acute decompensation due to rapid worsening of pHTN. However, due to severe MS in this case, treatments aimed at lowering pulmonary pressure would have the additional effect of limiting LV filling and could potentially precipitate LV failure.
In cases of mitral valve stenosis with concomitant tricuspid regurgitation, it has been proposed in surgical literature that these pathologies should be corrected in stages, with mitral repair followed by tricuspid 7-14 days later. This allows for some pulmonary hypertension improvement, with pulmonary vascular remodeling before tricuspid pathology is repaired. One report suggested a benefit to this “double-staged” approach for multiple- valve surgery, however our patient was too physiologically tenuous and likely would not survive a second exposure to CPB in the week following her first [7]. As was anticipated, repair of our patient’s MS precipitated acute RV failure that had to be managed intra-operatively with pulmonary vasodilators.
Multiple valve involvement with progressive stenosis usually occurs late in the disease course, either due to rheumatic involvement or subsequent dilation. In patients undergoing double valve replacement, it was noted that NYHA status and hemoglobin levels were successful predictors of surgical outcome [8]. Both were significantly compromised in this patient due to her aforementioned comorbidities. Traditionally TR is a poor prognostic indicator in the MV valve repair recovery period. Studies have also shown that uncorrected TR can actually worsen in the period post MV repair [9-11]. In our patient, her TR was already advanced and was already complicated by CHF.
Severe biatrial dilatation can predispose the patient to malignant arrhythmias and thromboembolism, not to mention challenges in sternotomy, surgical exposure, and cannulation [8].The selection of vasopressor/inotropes had to be carefully titrated, given the patient’s multiple cardiac pathologies affecting loading conditions and function, with additional supplementation of amiodarone due to high likelihood of postoperative arrythmia.
These distinct pathologies, while themselves not exceedingly rare, are more uncommon presenting together in the typical bypass patient. The presence of severe diastolic dysfunction in the setting of tricuspid and mitral valve stenosis creates a tenuous milieu centered around the stenotic mitral valve. Any quick correction of forward flow, especially in the pulmonary vasculature, could have lead to a sudden drop in left ventricular preload resulting in systolic collapse. Considering the increasing elderly immigrant population in many parts of the US, discussion of the complex interaction of the pathologies secondary to advanced RHD remains important for both academic and practical purposes.
References
1.Marijon E, Mirabel M, Celermajer DS, et al. Rheumatic heart disease. The Lancet. 2012; 379: 953-964.
2.Kumar R, Tandon R. Rheumatic fever & rheumatic heart disease: The last 50 years. Indian J Med Res. 2013; 137: 643.
3.Woldu B, Bloomfield G. Rheumatic heart disease in the twenty-first century. Curr Cardiol Rep. 2016;18: 96.
4.Karpawich AJ. Evaluation of general anesthesia for rheumatic heart disease. Oral Surgery, Oral Medicine. Oral Pathology. 1950; 3: 631-637.
5.Reckard D, Cipcic E, Mackin C. Mitral valve replacement: a case report. AANA J. 2008; 76: 125-129
6.Akca B, Erdil N, Disli OM, et al. Coronary Bypass Surgery in Patients with Pulmonary Hypertension: Assessment of Early and Long Term Results. Annals of Thoracic and Cardiovascular Surgery. 2015; 21: 268-274.
7.Jouan J, Achouh P, Besson L, et al. Advanced mitral-tricuspid disease with severe right ventricular dysfunction: the double- staged approach. Ann Thorac Surg. 2012; 94: 992-993.
8.Fernandes AMS, Andrade GMd, Oliveira RM, et al. Evaluation of variables responsible for hospital mortality in patients with rheumatic heart disease undergoing double valve replacement. Revista Brasileira de Cirurgia Cardiovascular. 2014; 29: 537-542.
9.Binder T, Bosenhek R, Frank H, et al. Congenital malformation of the right atrium and the coronary sinus: an analysis based on 103 cases reported in the literature and two additional cases. Chest. 2000; 117: 1740-1748.
10.Karpawich AJ. Evaluation of general anesthesia for rheumatic heart disease. Oral Surgery, Oral Medicine. Oral Pathology. 1950; 3: 631-637.
11.Kim JB, Yoo DG, Kim GS, et al. Mild-to-moderate functional tricuspid regurgitation in patients undergoing valve replacement for rheumatic mitral disease: the influence of tricuspid valve repair on clinical and echocardiographic outcomes. Heart. 2012; 98: 24-30.