Effect of Malaria Infection in Pregnancy on Some Inflammatory and Haematological Indices at Nnamdi Azikiwe University Teaching Hospital, Nnewi
Author'(s): Ifeanyichukwu M.O1*, Okezie B.N1,2 and Obi E3
1 Department of Medical Laboratory Science, Immunology Unit, Faculty of Health Science and Technology, Nnamdi Azikiwe University, Anambra State, Nigeria.
2 Department of Medical Laboratory Science, Haematology unit, Faculty of Health Science and Technology, Nnamdi Azikiwe University, Nnewi Campus, Anambra state, Nigeria.
3Department of Pharmacology and Therapeutics, Toxicology Unit, Faculty of Medicine, Nnamdi Azikiwe University, Anambra State, Nigeria.
*Correspondence:
Ifeanyichukwu M.O, Department of Medical Laboratory Science, Immunology Unit, Faculty of Health Science and Technology,Nnamdi Azikiwe University, Anambra State, Nigeria, E-mail:moifeanyi@yahoo.co.uk.
Received: 21 April 2019; Accepted: 28 May 2019
Citation: Okezie B. N, Ifeanyichukwu M. O, Obi E. Effect of Malaria Infection in Pregnancy on Some Inflammatory and Haematological Indices at Nnamdi Azikiwe University Teaching Hospital, Nnewi. Clin Immunol Res. 2019; 3(1): 1-5.
Abstract
This study was carried out to determine the effect of malaria infection in pregnancy on some inflammatory and haematological indices. It was carried out at the ante natal clinic of Nnamdi Azikiwe University Teaching Hospital, Nnewi. Two hundred and sixty two subjects were recruited comprising: Two hundred and six pregnant women who tested positive to malaria infection and fifty-six who tested negative to malaria infection. C-reactive (CRP), Complements 3 and 4 (C3 and C4), were determined using turbidimetric method, haematological parameters were done using automation method and malaria infection was determined using Giemsa staining technique. Pearson correlation was used to test for relations while Student t-Test and Analysis of Variance (ANOVA) were used to analyze significance of differences in mean values between groups and among groups respectively. The C3 and C4 were significantly reduced in pregnant women infected with malaria parasite when compared with control (P<0.05 in each case). The C3 did not show any significant difference among the trimesters (P>0.05 in each case). However, C4 was significantly reduced in pregnant women with malaria infection in their first and third trimesters when compared with the second trimesters (P<0.05 in each case). The CRP was significantly higher in malaria infected pregnant women than the control (P<0.05). Malaria infected pregnant women in their second and third trimesters showed a significant higher CRP value when compared with the first trimester (P<0.05 in each case). The haematocrite (HCT), and haemoglobin (Hb) levels of malaria infected pregnant women were significantly lower when compared with the control (P<0.05 in each case). The other haematological parameters (red blood cell (RBC), and mean cell haemoglobin concentration (MCHC)) showed no significant difference between pregnant women infected with malaria and the control (p >0.05 in each cases). There was an observed significant correlation between C3 and HCT, Hb, and RBC but C4 and CRP showed no significant correlation with any of the haematological indices. In conclusion there was reduced CRP and C3 and C4 and also HCT and Hb in malaria infected pregnant women in comparison with control subjects. The RBC and MCHC showed significant difference.
Keywords
Introduction
Malaria is transmitted from an infected mosquito to a human host when plasmodium sporozoites in the saliva of the mosquito are transferred into the capillary bed of the host [1]. Pregnant women, immune compromised persons and younger children under 5years are at a higher risk of infection than others [2]. The risk of malaria infection and clinical disease is usually higher in pregnant than non-pregnant women [3]. Several factors contribute to the increased risk which could be immunologic, hormonal or physical. Other contributing factors are gestational age, parity and maternal age [4].
Evidences have shown that younger women in their adolescent stage are at a greater risk of malaria infection irrespective of their parity. Malaria in pregnancy is often associated with high risks of miscarriages, premature deliveries, maternal morbidity and neonatal deaths [5].
Malaria pathogenesis often causes alterations in the haematological parameters [6], which include reduction in haemoglobin concentration [7], other red cell indices [8] changes in total white blood cell count, and thrombocytopenia [9]. There is rapid haemolysis and sequestration of infected red blood cells during malaria in pregnancy which often lead to anaemia [10]. Severe malaria in pregnancy can lead to death or be associated with other conditions e.g. eclampsia to cause maternal morbidity [5]
The complement system, which consists of small proteins that are synthesized mainly in the liver [11], is a part of the innate immune system that enhances the ability of the phagocytic cells to clear invading pathogens from the body. Complements can cause the destruction of malaria infected erythrocytes through the phagocytic process and induction of inflammation [12]. Inflammation is a considered as a mechanism of the innate immunity because it is non-specific to causative agent [13]. It responds to the infection, eliminates the causative agent and repairs the damage caused by the initiating factor [14]. C reactive protein is a serum acute phase protein [15] produced by the liver and increases in the presence of inflammation in the body. C reactive protein activates the classical complement cascade, opsonises bacteria for phagocytosis, stimulates phagocytic cells, and can also bind to the parasitized red blood cells [16].
Haemoglobinopathies, level of malaria endemicity, malaria immunity and nutritional status of an individual can lead to varying alterations in the haematological indices during malaria infection [17]. In malaria endemic regions, malaria in pregnancy causes maternal anaemia by increasing red blood cell destruction and decreasing erythropoiesis [18]. During pregnancy, there is a decrease in PCV because the plasma volume increases and predisposes to haemodilution, increased rate of infection especially malaria, hormonal changes and other conditions that promote inflammation [19].
Materials and Method
Study area and sample population
This study was conducted at the Nnamdi Azikiwe University Teaching Hospital (NAUTH) Nnewi, Ananmbra state. Nnamdi Azikiwe University Teaching Hospital is a tertiary health institution that serves as a reference center for Nnewi metropolis and beyond. Ethical approvals was obtained from the NAUTH Ethics committee and informed consent administered to the participants prior to recruitment. Two hundred and sixty-two pregnant women aged between 18-45 years were selected for this study and are grouped into two hundred and six who tested positive for malaria infection and fifty six who tested negative for malaria infection.The study population was selected from those that are not on any non-steroidal anti-inflammatory drugs, no history of rheumatoid arthritis, systemic lupus erythematosus (SLE) and other inflammatory disorders.
Sample collection and laboratory analysis
Blood samples (four milimeters) were drawn asceptically from each subject by venepuncture. From the collected sample, 2mls was dispensed into a plain container, allowed to clot and serum obtained for inflammatory markers estimation. The remaining 2mls was dispensed into a container with potassium ethylene- diamine tetra acetic acid (K3-EDTA) at a concentration of 1.5mg/ ml, properly mixed and labelled for full blood count estimation and thick smear preparation.
Estimation of Malaria Parasite
Properly prepared and air-dried thick smear slides were placed face downwards in a shallow tray supported on two rods. Diluted Giemsa stain (10%) was poured into the shallow tray and the slides stained for 60minutes. Afterwards the stained slides were washed using buffered water, the back side cleaned and placed in a draining rack to air-dry. When the thick films were completely dried, a drop of immersion oil was applied to an area of about 10mm in diameter, examined for ringforms, trophozoites, pigments, etc using 100X objective and reported appropriately using the plus sign (+) grading system.
Complement Factor 3 (C3)
This was done using turbidimetric method and reagents supplied by Cromatest Linear Chemicals, Barcelona, Spain. The reagent and the spectrophotometer were pre-warmed to 37oC. Then, distilled water was used to zero the photometer. One mililiter (1ml) of C3 Reagent (R1) was dispensed into the cuvette and ten microliter (10µl) of serum was also added. The whole mixture was mixed properly and inserted into the spectrophotometer. The absorbance (A) was recorded after 2minutes at 340nm. The concentration of the C3 was extrapolated from the calibration curve.
Complement Factor 4 (C4)
This was done using turbidimetric method and reagents supplied by Cromatest Linear Chemicals, Barcelona, Spain. The reagent and the spectrophotometer were pre-warmed to 37oC. Then, distilled water was used to zero the photometer. One mililiter (1ml) of C4 Reagent (R1) was dispensed into the cuvette and twenty-five microliter (25µl) of serum was also added. The whole mixture was mixed properly and inserted into the spectrophotometer. The absorbance (A) was recorded after 2minutes at 340nm. The concentration of the C4 was extrapolated from the calibration curve.
C-Reactive Protein (CRP)
This was done using turbidimetric method and reagents supplied by Cromatest Linear Chemicals, Barcelona, Spain. The reagent and the spectrophotometer were pre-warmed to 37oC. Then, distilled water was used to zero the photometer. One mililiter (1ml) of Working Reagent was dispensed into the cuvette and five microliter (5µl) of serum was also added. The calibrator was also treated the same way as the sample. The whole mixture was mixed properly and inserted into the spectrophotometer. The absorbance (A1) was recorded immediately and Absorbance (A2) after 2 minutes at 540 nm. The concentration of the CRP was calculated using the formula provided by the manufacturer.
Full Blood Count (FBC)
This was done using Abacus 380 haematology analyser (manufactured by Budapest) based on aperture impedance principle. The K3-EDTA anticoagulated whole blood sample was homogenously mixed using a mechanical mixer and placed in the sample adapter of the analyser and the ‘Start’ button pressed. The sample rotor turns the container into the inside of the instrument and in-built needle draws sample from the tube. After, a few seconds, the rotor turns out and the sample removed from the adapter. Inside the fluidic system, the different components were automatically analysed and the result displayed and then printed from the analyzer.
Data analysis
The data obtained was analysed using statistical package for social sciences (SPSS) (version 20). Data were expressed as mean ± SD. The significance of differences in mean values between groups were analysed using Student’s (independent) t-test, while significance of the differences in mean values among different groups was evaluated using one-way ANOVA. The test for relationship was done using Pearson correlation. Results were considered statistically significant at P<0.05, unless otherwise stated.
Results
Table 1 shows the comparison of inflammatory markers based on malaria infection. It was observed that the Mean ± SD C3 and C4 values) of pregnant women with malaria infection (117.04 ± 16.86 mg/dl and 26.19 ± 2.60 mg/dl respectively) was lower than that of non-infected pregnant women (128.89 ± 20.09 mg/dl and 27.23 ± 3.62 mg/dl respectively), p <0.05 in both cases. It was also observed that the CRP Mean ± SD values of the pregnant women infected with malaria (8.35 ± 6.41 mg/l) was higher than that of the non-infected ones (5.14 ± 2.98 mg/l), and this difference was significant, p = 0.001.
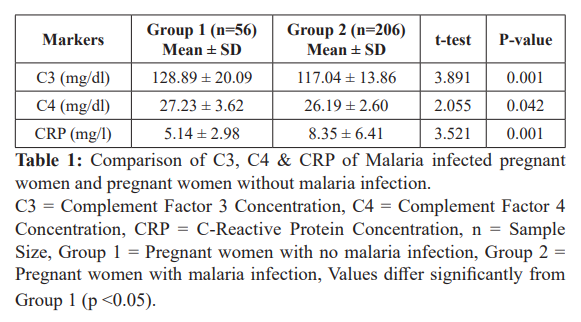
Table 2 shows the Mean values of C3, C4 & CRP at different trimesters for malaria infected pregnant women. No significant difference in C3 value (p = 0.185) was observed among the various trimesters but a significant difference was observed in the C4 values of malaria infected pregnant women (p = 0.001) among the groups. Post-hoc analysis revealed that the C4 value was significantly lower in first (25.94 ± 2.51 mg/dl, p = 0.017) and third (25.09 ± 1.85 mg/dl, p = 0.001) trimesters compared to the second trimesters (27.64 ± 2.80 mg/dl). But no significant difference was observed between the first and third trimesters, p = 0.329.
Furthermore, there was a significant difference in the CRP value of malaria infected pregnant women (p = 0.001) among the various trimesters. The Tukey post-hoc analysis indicated that the CRP value was significantly higher in second (10.70 ± 4.75mg/l, p = 0.001) and third (10.25 ± 5.87mg/l, p = 0.001) trimesters compared to the first (4.48 ± 6.50mg/l). But no significant difference was observed between the second and third trimesters, p = 0.949.
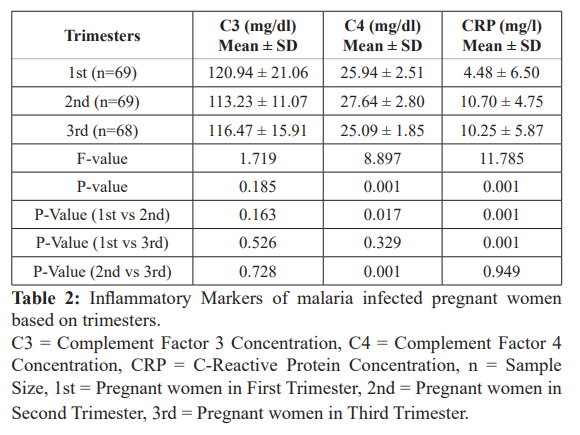
Table 3 shows the comparison of the haematological indices based on malaria infection. It was observed that malaria infected pregnant women had significantly lower Mean ±SD HCT and Hb values (32.43 ± 2.51% and 10.85 ± 0.89g/dl respectively) than those who are non-infected (35.01 ± 1.66% and 11.91 ± 0.55g/dl respectively), p = 0.001 in both cases. The other haematological indices: RBC and MCHC showed no statistically significant difference, p = 0.737, p = 0.493 respectively.
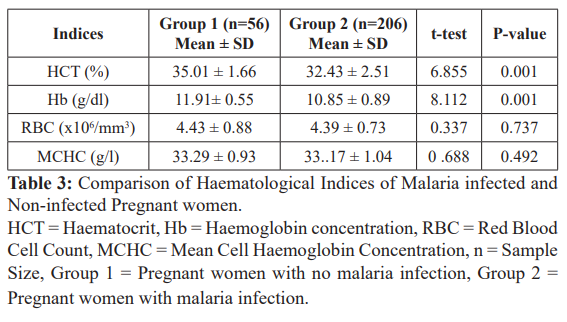
Table 4 shows the comparison between the Mean (± SD) values of HCT, HB, RBC, and MCHC at different trimesters for malaria infected pregnant women. The table shows a significant difference between the HCT value (P = 0.041) in malaria infected pregnant women among the various trimesters. Post-hoc test revealed a significantly lower HCT value in third (31.54 ± 2.46%, p = 0.045) trimesters compared with second (33.05 ± 2.18%) trimesters. There were no significant differences between the first (32.72 ± 2.66%) and second (33.05 ± 2.18%) trimesters (p = 0.850). Again, there were no observed significant differences between the HB, RBC, and MCHC values in malaria infected pregnant women among the various trimesters.
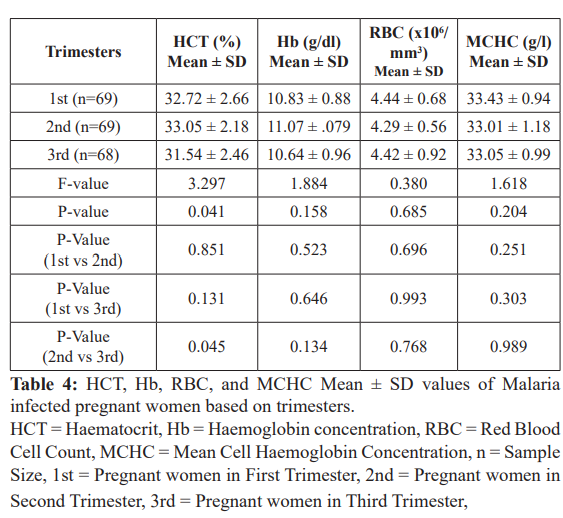
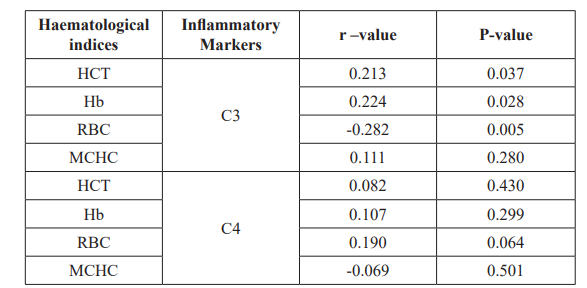
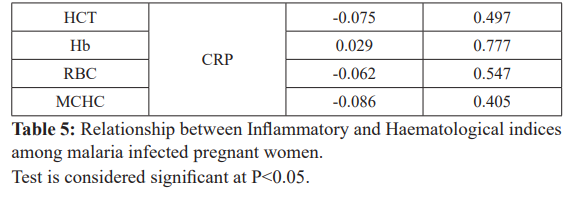
Table 5 shows the relationship between C3 C4 and CRP values and haematological indices of malaria infected pregnant women. Significant positive correlations between C3 and HCT (r = 0.213, p = 0.037), Hb (r = 0.224, p = 0.028), and negative significant RBC (r = - 0. 282, p = 0.005) were observed in malaria infected pregnant women while MCHC showed no significant correlation with C3 in malaria infected pregnant women r =0.111, p = 0.280 The C4 and CRP values of pregnant women infected with malaria showed no significant correlation with any of the haematological indices, p>0.05.changes, iron deficiency and conditions that promote fluid retention can also lead to decrease in HCT. Although, the HCT value of the malaria infected women among the various trimesters showed a significant difference but the mean values were within the WHO reference ranges for pregnancy. However, the Hb values among the various trimesters did not show significant variation, as the mean values were also within the WHO reference ranges for pregnancy [23]. This agrees with the study by Osonuga et al., [24] but disagrees with previous studies done by Idowu et al., [25]; Ichipi-Ifukor et al., [26] and Ukibe et al., [27]. The lack of significant difference may be due to implementation of focused ante-natal care for the pregnant women, and adequate management of their blood profiles with various dietary supplementations [28].
Discussion
Increased rate of infection during malaria causes reduction in HCT and Hb leading to anaemia in pregnant women. This finding is in consonance with previous studies of Adesina et al. [8], Erhabor et al. [20], Akinboye et al. [21] and Jombo et al. [22]. Hormonal
During invasion by plasmodium, complement is the one of the first line of defense against invasion [29]. The complement system is a part of the immune system that helps or improves the ability of antibodies and phagocytic cells to clear pathogens from an organism, hence its consumption when there is an infection. In this study, mean value of the C3 was significantly reduced in pregnant women with malaria infection than the control. There was a significant reduction in the mean value of C4 of pregnant women with malaria when compared with the control. Also, there was a significant difference in C4 values of both malaria infected and non-infected pregnant women among the various trimesters. CRP is an acute phase protein that is involved in the activation of complement, acceleration of phagocytosis and detoxification of substances released from the damaged tissue. In this study, CRP value was found to be significantly higher in pregnant women with malaria infection compared to the control. This conforms to the findings of Banik and Adhikary, [30]; Lima-Junior et al., [31]; Agrawal et al., [32]; and Utuk et al., [33]; although they findings were based on malaria infection but not compared in pregnancy. During an infection, CRP are mobilised to the site to aid activation of complements. Hence, they are increased while the activated complements factors are utilised in the process of phagocytosis.
The findings of this study showed reductions in the HCT, Hb, C3 and C4; and an increase in CRP values of pregnant women infected with malaria. This shows that malaria infection causes variations in certain inflammatory and haematological indices. Further studies are needed to elucidate more on these findings especially in relation to malaria parasite density. It is also recommended that laboratory tests on inflammatory markers be included in the focused ante-natal care package for malaria infected pregnant women in endemic regions.
References
- Schantz-Dunn J, Nour MN. Malaria and pregnancy: A global health Reviews in Obstetrics and Gynecology. 2009; 2: 186-192.
- Autino B, Corbett Y, Castelli F, et Pathogenesis of malaria in tissues and blood. Meditterean Journal of Hematology and Infectious Diseases. 2012; 4: e2012061.
- Takem E, D’Alessandro Malaria in pregnancy. Mediterranean Journal of Hematology and Infectious Disease. 203; 5: e2013010.
- Ayoola OO, Whatmore A, Balogun WO, et al. Maternal malaria status and metabolic profiles in pregnancy and in cord blood Relationships with birth size in Nigerian Malaria Journal. 2012; 11: 75.
- Adam I, Elhassan EM, Mohmmed AA, et al. Malaria and pre- eclampsia in an area with unstable malaria transmission in Central Malaria Journal. 2011; 10: 258.
- Kotepui M, Phunphuech B, Phiwklam N, et al. Effect of malaria infection on haematological parameters in population near Thailand-Myanmar Malaria Journal. 2014; 13: 218-225.
- Uneke CJ. Impact of placental plasmodium falciparum malaria on pregnancy and perinatal outcome in Sub-saharan Africa Part III Placental Malaria, Maternal Health and Public Health. Yale Journal of Biology and 2008; 81: 1-7.
- Adesina KT, Balogun OR, Babatunde AS, et Impact of malaria parasitemia on haematological parameters in pregnant women at booking in Ilorin Nigeria. Trends in Medical Research. 2009; 4: 84-90.
- Abdalla SPG. Platelets and blood coagulation in human Imperial College Press London. 2004; 249-276.
- Ngassa Malaria and pregnancy. Postgraduate research training in Reproductive Health. Faculty of Medicine University of Yaounde. 2004.
- Walport MJ. Complement Second of two parts. New English Journal of 2001; 344: 1140-1144.
- Guo RF, Ward PA. Role of C5a in inflammatory responses. Annual Review of 2005; 23: 821-852.
- Abbas AB, Lichtman Functions and disorders of the immune system. Innate immunity In Basic Immunology. 3rd Edition. Saunders Elsevier Missouri USA. 2009.
- Nathan Points of control in inflammation. Nature. 2002; 420:846-852.
- Lima-Junior JD, Rodrigues-da-Silva RN, Pereira VA, et Cells and mediators of inflammation C-Reactive protein, nitric oxide, platelets and neutrophils in the acute and convalescent phases of uncomplicated Plasmodium vivax and Plasmodium falciparum infection. Memorias do Instituto Oswaldo Cruz. 2012; 107: 1035-1041.
- Ansar W, Bandyopadhyay SM, Chowdhury S, et Role of C-reactive protein in complement-mediated haemolysis in malaria. Glycoconjugate Journal. 2006; 23: 233-240.
- Erhart LM, Yingyuen K, Chuanak N, et al. Hematologic and clinical indices of malaria in a semi-immune population of Western Thailand. American Journal of Tropical Medicine and 2004; 70: 8-14.
- Menendez C, Fleming AF, Alonso PL. Malaria-related anaemia. Parasitology 2000; 16: 469-476.
- American College of Obstetricians and Gynecologists . ACOG Practice Bulletin 0095: Anaemia in pregnancy. Obstetricians and Gynecologists. 2008; 112: 201-208.
- Erhabor O, Adias TC, Hart Effects of falciparum malaria on the indices of anaemia among pregnant in the Niger Delta of Nigeria. Journal Of Clinical Medicine and Research. 2010; 2: 035-041.
- Akinboye DO, Okonofua CC, Awodele O, et The influence of malaria on some haematological parameters in pregnancy. Nigerian Journal of Parasitology. 2011; 32: 187-191.
- Jombo GTA, Mbaawuaga EM, Ayegba AS, et Anaemia, malaria burden and its control methods among pregnant women in a semi-urban community of Northern Nigeria. Journal of Public Health and Epidemiology. 2011; 3: 317-323.
- http://pdf.usaid.gov/pdfdocs/Pnada621.pdf.
- Osonuga IO, Osonuga OA, Onadeko AA, et al. Haematological profile of pregnant women in Southwest of Asian Pacific Journal of Tropical Disease. 2011; 1: 232-234.
- Idowu OA, Mafiana CF, Sotiloye D. Anaemia in pregnancy: A survey of pregnant women in Abeokuta, Nigeria. African Health 2005; 5: 295-299.
- Ichipi-Ifukor PC, Jacobs J, Ichipi-Ifukor RN, et Changes in haematological indices in normal pregnancy. Physiology Journal. 2013; 10: 1155-1159.
- Ukibe SN, Ikeako L, Mbanugo J, et Prevalence of anaemia in pregnant women attending antenatal clinics in Anambra State South- Eastern Nigeria. International Journal of Advanced Research. 2013; 1: 65-69.
- Federal Ministry of Health. Malaria during pregnancy: In the context of Focused Antenatal Care. An orientation package for Health Care Provider. Abuja Nigeria FMOH and Malaria Action 2014; 66-71.
- Tham WH, Schmidt CQ, Hauhart RE, et Plasmodium falciparum uses a key functional site in complement receptor type-1 for invasion of human erythrocytes. Blood. 2011; 118: 1923-1933.
- http://www.japi.org/march_2009/tropical_medicine_poster_html.
- Agrawal V, Vaishali J, Shubho Evaluation of C-reactive protein as a biochemical marker for assessing disease severity in malaria. IOSR Journal of Dental and Medical Sciences. 2013; 8: 23-26.
- Utuk EE, Ikpeme EE, Udo JJ, et al. Relationship between serum C-reactive protein levels and severity of Plasmodium falciparum malaria in children seen in South-South Nigeria. International Journal of Tropical Disease and 2004; 4: 1078-1087.