Effectiveness of Analgesia Nociception Index (ANI) As a Monitoring Tool to Evaluate Intraoperative Pain in Pediatric Patients Undergoing Sevofluorane Sedation and Locoregional Anesthesia
Author'(s): Ragone R, Lavermicocca T, Maranzano F, De Renzo F, Labellarte C, Lasorella ML and Milella L*
Pediatric Department of Anesthesia and Intensive Care UnitGiovanni XXIII Hospital-Policlinico di Bari, Italy.
*Correspondence:
Milella L, Pediatric Department of Anesthesia and Intensive Care Unit- Giovanni XXIII Hospital-Policlinico di Bari, Italy
Received: 21 Jan 2023; Accepted: 01 Feb 2023; Published: 09 Mar 2023
Citation: Ragone R, Lavermicocca T, Maranzano F, et al. Effectiveness of Analgesia Nociception Index (ANI) As a Monitoring Tool to Evaluate Intraoperative Pain in Pediatric Patients Undergoing Sevofluorane Sedation and Locoregional Anesthesia. Anesth Pain Res. 2023; 7(1): 1-4.
Abstract
Background: We present our results about pediatric patients undergoing sevofluorane sedation and locoregional anesthesia (LRA) referred for visceral, urological and orthopedic surgery, using Analgesia Nociception Index (ANI) as a monitoring tool for intraoperative pain.
Objective: The aim of this study was to evaluate the effectiveness of ANI to provide assessment of locoregional anesthesia success (opiod-free anesthesia) following skin incision in pediatric patients sedated with sevofluorane.
Materials and Methods: We enrolled 60 patients aged 2-17 years from September 2022 to November 2022. All patients were eligible for locoregional anesthesia, not suffering from cardiac arrhythmias, neurological disorders and not treated with opioids or drugs interfering with Autonomic Nervous System. Following preoperative assessment and consent, premedication with midazolam (0,5 mg/Kg per os) was used. Standard monitoring (SpO2 , HR, ECG, NIBP, body temperature sensor) and ANI was placed prior to induction of anesthesia. Once intravenous access had been established, anesthesia was induced with sevofluorane or propofol, was maintained with sevofluorane (MAC 1.3 in oxygen) and then ultrasound guided locoregional anesthesia was performed. ANI values were recorded prior to skin incision (T0) after 30 seconds (T1) and after 2 minutes (T2) from skin incision. A rise in HR≥10% from baseline occurring within the 2 minutes after skin incision was considered to be a LRA failure, which requires fentanest (1-2 γ/Kg). A rise in HR<10% from baseline occurring within the 2 minutes after skin incision was instead considered LRA success, not requesting opioid.
Results: 43 patients presented LRA success and 17 patients presented LRA failure. In the LRA failure group, skin incision caused ANI values decrease (p<0,05) within 30 seconds from skin incision. We described that ANI<68 in the first 2 minutes following skin incision can identify LRA failure with a sensitivity of 100% and a specificity of 82.4% (AUC:0.984).
Conclusion: ANI values rapidly decrease after skin incision in case of LRA failure and this tool, alone or in combination with HR changes, could guide anesthesiologists in using intraoperative opioid in children over 2 years of age sedated with sevofluorane.
Keywords
Introduction
Locoregional anesthesia and analgesia have been shown to offer benefits over general anesthesia (shorter postoperative fasting times, avoidance of airway manipulation that is important because pediatric airway is more reactive than in adult) and over opioid- based analgesia (reducing paralytic ileus and desaturation risk).
Big-data studies establish that there is low incidence of serious complications of pediatric locoregional anesthesia thanks to ultrasound-guided techniques [1,2].
Ultrasound-guided locoregional anesthesia improves success rate over blind techniques and this means short procedure times with fewer needle passes, longer postoperative analgesia effects, and improved postoperative pain scores [2].
Locoregional anesthesia in children is generally performed after induction of sedation but prior to skin incision. Inadequate locoregional anesthesia is identified by an increase in the heart rate from the baseline, in response to a surgical stimulus, even if this parameter has been shown to be imprecise to evaluate effectiveness of locoregional anesthesia [3-6].
It is known that a noxious stimulus can lead to sympathovagal alterations [7], for this reason autonomic nervous system monitoring techniques may help clinician to identify promptly an inadequate analgesia. In this way, adjustment of the analgesic strategy can occur during surgery.
The Analgesia Nociception Index (ANI) is an online heart rate variability (HRV) analysis that can be used to assess pain presence in people undergoing general anesthesia [8-11]. HRV refers to the degree of change in time and frequency analysis of the interval between successive hearbeats, which reflects balance between sympathetic and parasympathetic nervous system. HRV monitoring devices measure and calculate HRV parameters such as standard deviations of RR intervals on electrocardiogram (time-domain analysis) or high frequency (HF)/low frequency (LF) ratio (frequency domain analysis) quickly, easily and not invasively [12,13]. LF components reflect both sympathetic and parasympathetic activities, whereas HF components only reflect parasympathetic activity. The LF/HF ratio represents a quantitative measure of the balance of the autonomic system and when the ratio is high, indicates an increase in sympathetic activity or inhibition of parasympathetic activity. ANI monitoring system shows parasympathetic activity in a numeric range between 0 (maximum pain) and 100 (absence of pain). Previous studies on ANI regarded ANI ≥50 as appropriate analgesia and predicted autonomic nervous system responsiveness caused by nociceptive stimulus when ANI <30 [14,15].
To date there is not much evidence for the use of ANI in children [11], therefore the aim of this study is to evaluate if ANI monitoring can provide early assessment of locoregional adequacy after skin incision in children sedated with sevofluorane.
Materials and Methods
In these study 60 patients, aged 2-17 years from September 2022 to November 2022 were recruited. All patients were eligible for locoregional anesthesia, not suffering from cardiac arrhythmias, neurological disorders and not treated with opioids or drugs interfering with Autonomic Nervous System. Following preoperative assessment and consent, premedication with midazolam (0,5 mg/Kg per os) was used. Standard monitoring (SpO2, HR, ECG, NIBP, body temperature sensor) and ANI (Figure 1) was placed prior to induction of anesthesia. Once intravenous access had been established, anesthesia was induced with sevofluorane or propofol, was maintained with sevofluorane (MAC 1.3 in oxygen) and then ultrasound guided locoregional anesthesia was performed. ANI values were recorded prior to skin incision (T0) after 30 seconds (T1) and after 2 minutes (T2) from skin incision. A rise in HR≥10% from baseline occurring within the 2 minutes after skin incision was considered a LRA failure [16], which requires fentanest (1-2 γ/Kg). A rise in HR<10% from baseline occurring within the 2 minutes after skin incision was instead considered LRA success, not requesting opioid.
ANI was continuously displayed on the Physiodoloris-specific monitor. The algorithm used for ANI has been well described by several authors [8-10] and ANI is expressed as a numerical value between 0 (maximum pain) and 100 (absence of pain).
Patients were allocated into two groups: patients whose heart rate increase was ≥10% from the baseline were in the failure group, whereas patients whose heart rate increase was <10% from the baseline were in the success group. Failure group patients were treated with fentanest 1-2 γ/Kg.
The data were compared by χ2 test (Chi-square test), Mann- Whitney test and Kruskal-Wallis test. A p-value<0.05 was considered significant.
To assess the ability of the parameters to identify failure of locoregional analgesia, receiver-operating characteristic (ROC) curves were generated varying the minimal value of ANI recorded during the firt 2 minutes after skin incision. The power calculation assumed an area under ROC of 0.75 with a Type 1 error of 0.05 and Type2 error of 0.20. Statistical analysis were performed using Stata/MP17 software.
Results
43 patients (71.7%) patients presented locoregional anesthesia (LRA) success and 17 (28.3%) presented locoregional anesthesia failure. There were no significant differences between these groups with respect to age, gender and weight (Table 1).
Skin incision resulted in a significant decrease in ANI (p<0.05) both at 30 seconds (T1) and at 2 minutes (T2) in the locoregional anesthesia failure group (Table 2). Results are shown in the box- plot in Figure 2.
We also described that ANIl<68 in the first 2 minutes following skin incision can identify LRA failure with a sensitivity of 100% and a specificity of 82.4% (AUC:0.984). Results of ROC analysis are shown in Figure 3.
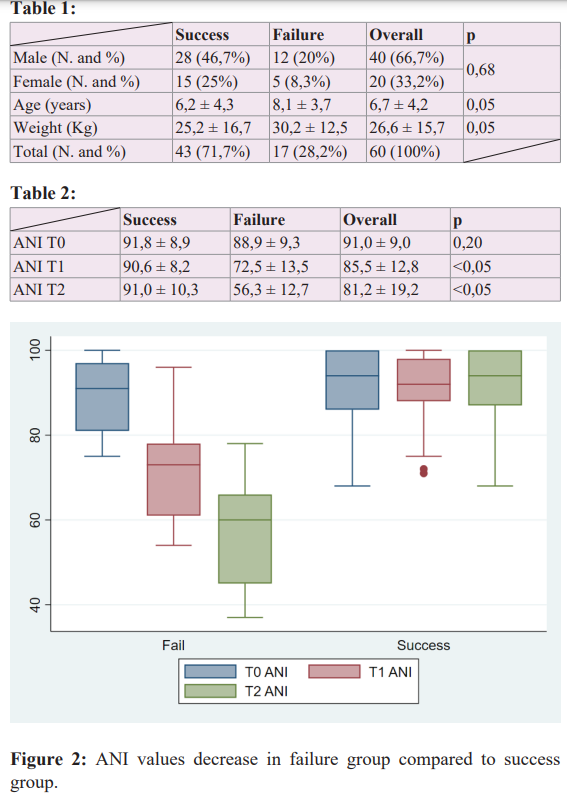
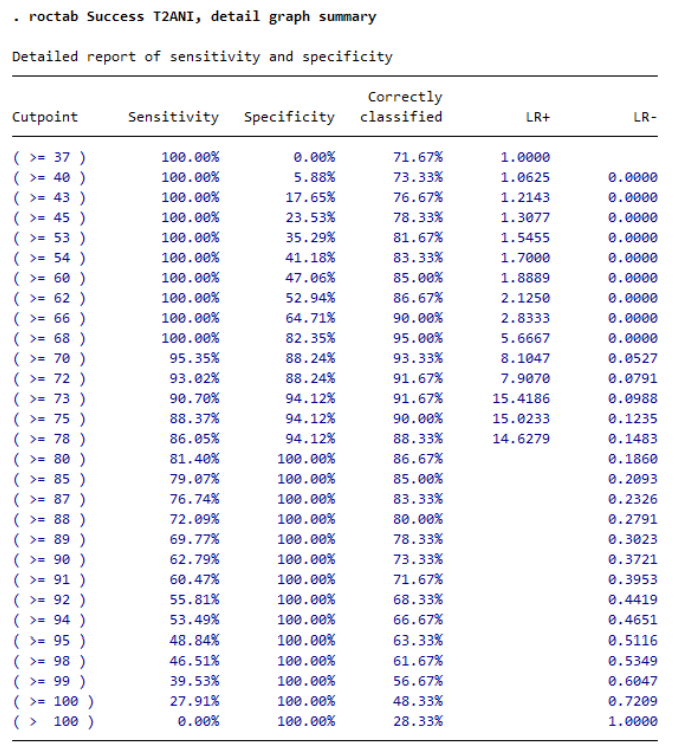
Figure 3: ROC analysis and cutoff values from minimal ANI recorded during the first 2 minutes following skin incision in the identification of failure of LRA.
Discussion
This study demonstrates that LRA failure is associated with a significant decrease in ANI values, in children over 2 years of age, within the first 30 seconds of skin incision.
ANI has been used successfully as a pain monitoring system during surgery in adults [17, 8-10] but there is still little evidence to support its use in pediatric patients [11].
Nowadays pediatric anesthetists still use to evaluate changes in heart rate from the baseline following skin incision to assess LRA adequacy [3-6] but it is important to consider that heart rate variations depend not only on the quality of LRA during surgery, but also on other factors such as age, volume status and depth of anesthesia. In addition to this, the percentage rise in heart rate required to establish LRA failure in pediatric patients under general anesthesia is still under debate [4-6].
In our department, we used an increase in heart rate of 10% from the baseline following skin incision, as an inadequate analgesia after LRA. Sevofluorane itself can have sympathetic and parasympathetic effects on the cardiovascular system in children [17,18] so there could be a pharmacological effect of the alogenate on the ANI values, even if it is unlikely that it could have a significant effect because recordings in both group were taken at steady-state, when end-tidal sevofluorane concentrations had been set to maintain a MAC (Minimum Alveolar Concentration) of 1.3.
Another limit of this study is due to the heterogeneity of patients, concerning different ages (2-17 years) and weights, and this affects the concentrations and volumes of the local anesthetics used to perform the nervous block, so the procedures were not standardized.
Conclusion
This study demonstrates that ANI values rapidly decrease after skin incision in case of LRA failure in children over 2 years of age, sedated with sevofluorane and not treated with opioids. This suggests that ANI monitoring system could represent a valid tool to discriminate LRA failure or success in pediatric patients undergoing general anesthesia or sedation and to realize an opioid- free anesthesia in children.
References
- Polaner DM, Taenzer AH, Walker BJ et Pediatric Regional Anesthesia Network (PRAN): a multi- institutional study of the use and incidence of complications of pediatric regional anesthesia. Anesth Analg 2012; 115: 1353-1364.
- Guay J, Suresh S, Kopp The use of ultrasound guidance for perioperative neuraxial and peripheral nerve blocks in children: a Cochrane review. Anesth Analg. 2017; 124: 948- 958.
- Ecoffey C, Lacroix F, Giaufré E, et al. Epidemiology and morbidity of regional anesthesia in children: a follow-up one- year prospective survey of the French-Language Society of Paediatric Anaesthesiologists (ADARPEF). Pediatr Anesth. 2010; 20: 1061-1069.
- Oberndorfer U, Marhofer P, Bo€senberg A, et Ultrasonographic guidance for sciatic and femoral nerve blocks in children. Br J Anaesth. 2007; 98: 797-801.
- Chhabra A, Sinha R, Subramaniam R, et al. Comparison of sub-Tenon’s block with v. fentanyl for paediatric vitreoretinal surgery. Br J Anaesth. 2009; 103: 739-743.
- Naja Z, Al-Tannir MA, Faysal W, et al. A comparison of pudendal block vs dorsal penile nerve block for circumcision in children: a randomised controlled trial. Anaesthesia. 2011; 66: 802-807.
- Benarroch Pain-autonomic interactions: a selective review. Clin Auton Res. 2001; 11: 343-349.
- Logier R, De Jonckheere J, Delecroix M, et Heart rate variability analysis for arterial hypertension etiological diagnosis during surgical procedures under tourniquet. Annu Int Conf IEEE Eng Med Biol Soc. 2011; 2011: 3776-3779.
- Logier R, Jeanne M, De Jonckheere J, et PhysioDoloris: a monitoring device for analgesia/nociception balance evaluation using heart rate variability analysis. Annu Int Conf Proc IEEE Eng Med Biol Soc. 2010; 2010: 1194-1197.
- Jeanne M, Clément C, De Jonckheere J, et al. Variations of the analgesia nociception index during general anaesthesia for laparoscopic abdominal surgery. J Clin Monit Comput. 2012; 26: 289-294.
- Sabourdin N, Arnaout M, Louvet N, et Pain monitoring in anesthetized children: first assessment of skin conductance and analgesia-nociception index at different infusion rates of remifentanil. Pediatr Anesth. 2013; 23: 149-155.
- Koenig J, Jarczok MN, Ellis RJ, et Heart rate variability and experimentally induced pain in healthy adults: a systematic review. Eur J Pain. 2014; 18: 301-314.
- Heart rate variability: standards of measurement, physiological interpretation and clinical use. Task Force of The European Society of Cardiology and The North American Society of Pacing and Electrophysiology. Circulation. 1996; 93: 1043-
- Upton HD, Ludbrook GL, Wing A, et Intraoperative “Analgesia Nociception Index”-guided fentanyl administration during sevoflurane anesthesia in lumbar discectomy and laminectomy: a randomized clinical trial. Anesth Analg. 2017; 125: 81-90.
- Szental JA, Webb A, Weeraratne C, et Postoperative pain after laparoscopic cholecystectomy is not reduced by intraoperative analgesia guided by analgesia nociception index (ANI®) monitoring: a randomized clinical trial. Br J Anaesth. 2015; 114: 640-645.
- Constant I, Nghe MC, Boudet L, et Reflex pupillary dilatation in response to skin incision and alfentanil in children anaesthetized with sevoflurane: a more sensitive measure of noxious stimulation than the commonly used variables. Br J Anaesth. 2006; 96: 614-619.
- Wodey E, Senhadji L, Pladys P, et The relationship between expired concentration of sevoflurane and sympathovagal tone in children. Anesth Analg. 2003; 97: 377-382.
- Constant I, Dubois MC, Piat V, et Changes in electroencephalogram and auto- nomic cardiovascular activity during induc- tion of anesthesia with sevoflurane compared with halothane in children. Anesthesiology. 1999; 91: 1604- 1615.
- Jeanne M, Logier R, De Jonckheere J, et Heart rate variability during total intravenous anesthesia: effects of nociception and analgesia. Auton Neurosci. 2009; 147: 91-96.