Eosinophilic Esophagitis in Adult Patients with Upper Gastrointestinal Symptoms: a Cross-Sectional Study in Northeastern Egypt
Author'(s): Mohamed El.alawy1, Mohamed Abo Elmagd1, Wafaa Hassan1, Wael Maher2, and Mohamed Fathalla Hassan1
1Department of Endemic and Infectious Diseases, Egypt.
2Department of Pathology, Faculty of Medicine, Suez Canal University, Ismailia, Egypt.
*Correspondence:
Mohamed Fathalla Hassan, Department of Endemic and Infectious Diseases, Egypt, Tel: +2- 01221420025; E-mail: Mfmhassan666@yahoo.com.
Received: 14 March 2019 Accepted: 08 April 2019
Citation: Mohamed El.alawy, Mohamed Abo Elmagd, Wafaa Hassan, et al. Eosinophilic Esophagitis in Adult Patients with Upper Gastrointestinal Symptoms: a Cross-Sectional Study in Northeastern Egypt. Gastroint Hepatol Dig Dis. 2019; 2(1): 1-6.
Abstract
Background and Aim of Study: Eosinophilic Esophagitis (EoE) is a chronic immune/antigen-mediated esophageal disease characterized clinically by symptoms related to easophageal dysfunction and histologically by eosinophil-predominant inflammation. This study was performed to determine the prevelance of eosinophilic Esophagitis in Adult patients with Upper Gastrointestinal symptoms in Ismailia Governate, Egypt.
Patients and Methods: This cross-sectional descriptive study recruited all patients with Upper Gastrointestinal Symptoms omitted for endoscopic evaluation at Suez Canal University Hospital, Endoscopic Unit, after giving written consent. Esophageal biopsy samples were obtained and histological evaluation for the presence of eosinophils was performed for every patient. EoE was defined with at least 15 eosinophils were present in a single
high-power field.
Results: Out of 354 adult patients with Upper Gastrointestinal symptoms underwent upper endoscopy, only 35 cases (10.2%) diagnosed as EoE based on presence of 15 eosinophils/HPF in esophageal biopsies.
Conclusion: Patients with persistent symptoms of severe GERD, who do or do not respond to PPI should undergo UGI endoscopy with multiple biopsies to exclude EoE.
Keywords
Introduction
Eosinophilic esophagitis (EoE) is a chronic immune/antigen- mediated esophageal disease characterized clinically by symptoms related to esophageal dysfunction and histologically by eosinophil- predominant inflammation [1]. Eosinophilic esophagitis is increasingly being recognized in adults and pediatric populations either as a separate entity or as a part of the spectrum eosinophilic gastroenteritis [2]. In adults, eosinophilic esophagitis can present in the third or fourth decades of life and various studies implicate it to be more predominant in men [3].
Eosinophilic esophagitis is a common diagnosis in patients with refractory Gastro-esophageal Reflux Disease (GERD). Patients with eosinophilic esophagitis are usually young men, present with a history of intermittent solid food dysphagia, and often have a history of food impaction. Most of these patients carry an underlying diagnosis of GERD [4,5].
The first case of eosinophilic esophagitis (EoE) was reported in 1977 in an adult patient [6]. However, In 1993, Attwood et al reported first case series of EoE in 12 adult patients and suggested that this is an entity distinct from GERD [7]. In 2005, Straumann and Simon reported an average incidence of 1.438 cases of EoE per 100,000 inhabitants over a 16-year observational period in Olten County, Switzerland [8]. The current prevalence in developed countries is between 45 and 55 cases per 100,000 population [9]. In Egypt, The prevalence of EoE is about 3.3% in adult patients presenting with upper gastrointestinal symptoms [10].
The pathogenesis of EoE is felt to be immune-mediated [1]. In response to antigen stimuli, either from food or environmental allergies, a Th3 inflammatory response is triggered and factors such as IL-4, IL-5, and IL-13 stimulate eotaxin-3, a potent chemokine, to traffic eosinophils to the esophageal mucosa [11]. When activated, the eosinophils cause local tissue damage and recruit other effector cells such as mast cells and fibroblasts, which play a role in esophageal remodeling [12,13].
The first consensus diagnostic guidelines for EoE were published in 2007 [14]. A key point emphasized in the 2007 guidelines was that EoE was a clinicopathologic condition. Because there was no single clinical finding or histologic feature that was pathognomonic for EoE, the sum of the clinical and histologic information had to be considered prior to making a diagnosis. To formalize this, the guidelines required three criteria to be met: 1) symptoms of esophageal dysfunction (i.e. dysphagia, food impaction, chest pain, heartburn); 2) a maximum esophageal eosinophil count of at least 15 eos/HPF in at least one microscopy field; and 3) lack of responsiveness to high dose PPI therapy (or a negative pH study) to exclude GERD as a cause of esophageal eosinophilia [14]. The consensus diagnostic guidelines were updated in 2011 and there were several notable changes. First, the guidelines provided a conceptual definition of EoE as an immune-mediated disorder with symptoms of esophageal dysfunction and eosinophil-predominant inflammation. This emphasized the clinicopathologic nature of the diagnostic process. Second, the updated guidelines still required three criteria to be met, but with some modifications: 1) clinical symptoms of esophageal dysfunction; 2) a maximum esophageal eosinophil count of at least 15 eos/HPF, with few exceptions 3) exclusion of other possible causes of esophageal eosinophilia, including PPI-responsive Esophageal Eosinophilia [1].
Endoscopically, EoE in adults is characterized by esophageal linear furrows with loss of vascularity, mucosal rings (trachealization), a small-caliber lumen, strictures, mucosal exudates, and, less commonly, polyps and ulcerations [15].
Patients and Methods Type of Study
Cross Sectional Descriptive Study. Site of Study: Upper Gastrointestinal endoscopy unit of Suez Canal University, Endoscopic Unit, Ismailia, Egypt. Study Population: Adult patients with upper gastrointestinal symptoms who will be omitted to UGI endoscopy at Suez Canal University Hospital, Endoscopic Unit.
Criteria of selection
Adult patients >18 years old with upper gastrointestinal symptoms who will be omitted to UGI endoscopy. All patients with decompensated chronic diseases, history of hypersensitivity reactions, receiving any form of corticosteroid therapy including inhaled preparations were excluded.
Study Methods
Patient assessment
Assessment of adult patients presented by upper gastro-intestinal manifestations was done using close ended questionnaire including personal data, presenting symptoms, data about endoscopy findings and histopathological examination of biopsy.
UGI Endoscopy
Upper GIT endoscopy was done for all participants with at least 3 biopsies taken from 2 different sites in the esophagus including the distal and either mid or proximal esophagus even if the esophagus appeared endoscopically normal.
Laboratory procedure
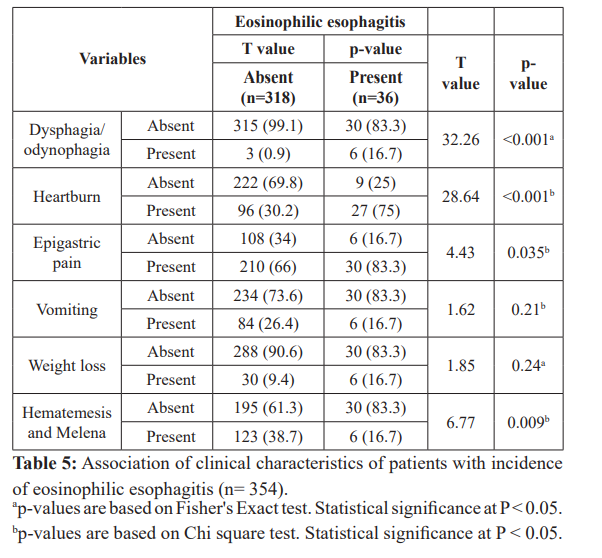
After hematoxylin/eosin staining, all biopsies were examined histopathologically by pathologist. An esophageal eosinophilic count >15/HPF, along with normal gastric and duodenal biopsies, substantiated the diagnosis of eosinophilic esophagitis.
Ethics
The study confirmed to the 1975 Declaration of Helsinki and was approved by the Ethics Committee of Suez Canal University Faculty of Medicine. Written, informed consent was obtained from each patient included in this study.
Statistical analysis
Statistical analyses were performed using the statistical software package SPSS for Windows, version 22 (SPSS, IBM Inc., NC, USA). Data will be prepared as tables and graphs, T-test will be used to compare quantitative data (expressed as mean ± standard deviation). Chi square test will be used to compare qualitative data (expressed as number and percentage). Significant P value will be considered at a level of ≤ 0.05.
Results
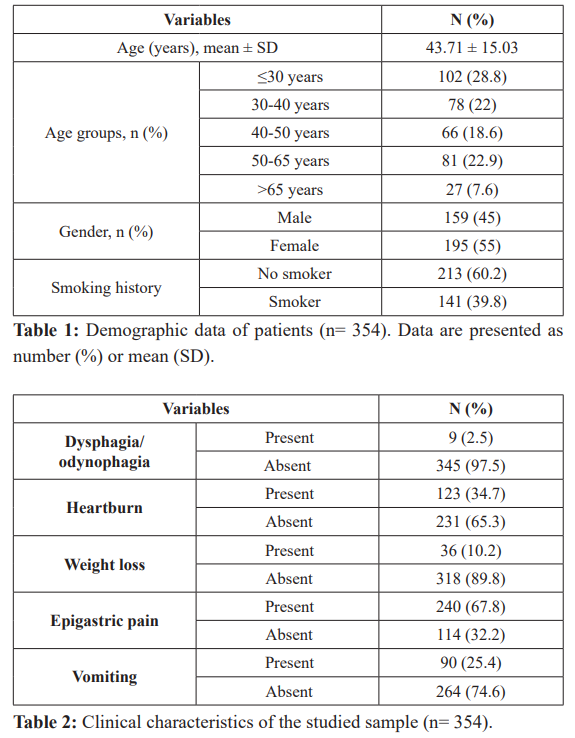
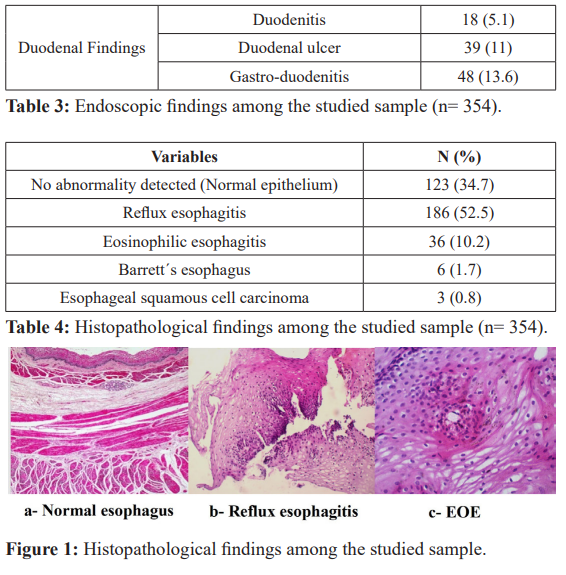
Mean age of participants was 43.71 ± 15.03 years; 195 (55%) of them were females and 159 (45%) were males, about 40% are smokers or had history of smoking. Epigastric pain was reported in 240 patients (67.8%), vomiting in 90 (25.4%), dysphagia in 9 (2.5%) and heartburn in 123 (34.7%). A history of weight loss was reported in36 cases (10.2%).
Endoscopic findings were as follow: GERD in 120 (33.9%); hiatus hernia in 39 (11%); Esophageal mass in 3 (0.8%); gastritis in 168 (47.5%); gastric ulcer in 54 (15.3%); gastric mass in 9 (2.5%); duodenitis in 18 (5.1); duodenal ulcer in 39 (11%) and gastro- duodenitis in 48 (13.6%). Normal endoscopic findings were present in 9 patients (2.5%).
The esophageal pathological findings were as follows: reflux esophagitis in 186 (52.5%), eosinophilic esophagitis in 36 (10.2%), Barrett´s esophagus in 6 (1.7%) and esophageal carcinoma in 3 (0.8%). No abnormality detected (Normal epithelium) was reported in 123 (34.7%).
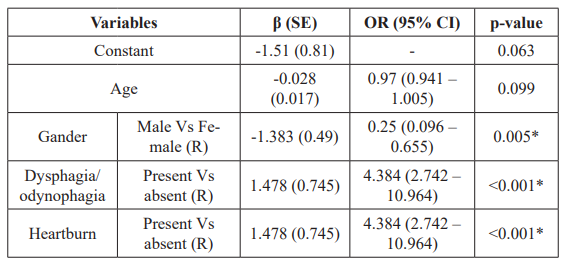
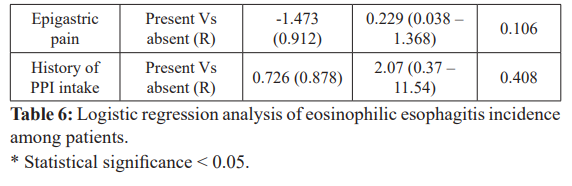
Logistic regression analysis was used to assess predictors of eosinophilic esophagitis incidence among patients. There is a decrease by 75% in the odds of having eosinophilic esophagitis for male patients compared to female one (p=0.005). Meanwhile, there is an increase in the odds of having eosinophilic esophagitis for those who came.
Complaining of dysphagia 4.38 times compared to who do not (p<0.001). Moreover, there is an increase in the odds of having eosinophilic esophagitis for those who came complaining of heartburn 2.32 times compared to who do not (p<0.001).

Discussion
Eosinophilic esophagitis (EoE) is likely when symptoms of esophageal dysfunction are present and is confirmed by an eosinophilic infiltrate in any part of the esophagus. A minimum of 15 eosinophils/HPF is required for a diagnosis of EoE [16]. The epidemiology of EoE varies; several studies have suggested that this is due to increasing incidence or more frequent recognition [17].
The purpose of our study was to determine EoE prevalence in adults complaining of UGI symptoms in our locality and to identify the clinical manifestations. In the current study, we included 354 patients with various upper gastro-intestinal symptoms, 10.2% of them had EoE. A prospective study in an Indian study included 185 patients with reflux symptoms, 3.2% of them had EoE. When patients with both GERD and EoE were compared to patients with GERD only, the authors found that the former group had higher percent of allergic history 16.6% versus 0.11% in the latter group, in addition to non-response to PPI. These two factors were considered predictors of EoE among GERD patients [18]. In a comparable Brazilian study, the prevalence of EoE was much lower (0.97%) in patients with refractory GERD [19].
Similarly, in An Egyptian study, was conducted at Al Kasr Al- Ainy hospitals, to address the prevalence of EoE among patients presenting with upper GI complaints found that the prevalence of EoE among GERD patients was 3.3%. EoE positive GERD patients in this study were more allergic than those EoE negative [10]. In another Egyptian study conducted in El-Minia University showed the prevelance of EoE among adult Patients with Upper Gastrointestinal Symptoms was 1.8% [20].
This variable prevalence may be attributed to the unrepresentative sample size in some studies, and rather because of using different diagnostic criteria. Also, EOE may be isolated or to be as part of diffuse eosinophilic gastroenteritis, and/or after rolling out Coeliac disease. As a result, what is thought to be GERD could turn out to be EoE; similar to the conclusions of Markowitz et al. study where they found that 15% of the studied population was firstly diagnosed as GERD patients [21].
In the current study, Mean age of participants was 43.71 ± 15.03 years, 55% of them were females and 45% were males, 40% are smokers or had history of smoking. In our research, most EoE patients were younger than 40 years, these findings were similar to those found in an Egyptian study contucted in El-Minia University which found that all EoE patients were younger than 40 years [20]
Symptoms of EoE vary with age [22]. The most presenting symptoms in adults include dysphagia, food impaction, heartburn and chest pain [23]. The typical symptoms of GERD patients are heartburn and regurgitation [24]. In current study, the most common presenting symptoms among patients was epigastric pain (67.8%) which was similar to study contucted in El-Minia University which showed that Epigastric pain was reported in 138 patients (63.3%) [20]. In another Australian study found that dysphagia was present in 64.0% and in up to 89% of EoE patients [25]. Moreover, a study in the United States showed that the most common endoscopy indication in adults with EoE was dysphagia (70.1%), followed by GERD/heartburn (27.1%) [26].
EoE may be underestimated or missed on endoscopic examination [25]. Thus, even with a high index of suspicion, the presence or absence of endoscopic findings of EoE is inadequate to make a definitive diagnosis. Mucosal biopsy samples should be taken regularly from any patient with EoE symptoms (unexplained dysphagia, refractory heartburn, or chest pain), regardless of the endoscopic findings [27]. Endoscopic findings of EoE include: esophageal rings, strictures, narrow-caliber esophagus, linear furrows, white plaques or exudates, and pallor or decreased vasculature [28].
In our study, thirteen of the thirty-six positive cases of EoE (36.1%) showed normal endoscopic appearance of the esophagus and twenty third had an overlap with GERD. One study of histologically confirmed EoE reported that 8.8% of patients had no detectable endoscopic findings of EoE [17]. Another study reported normal endoscopic findings in 17% of histologically confirmed EoE cases [27]. Moreover, a study by Hunter et al, found a normal esophageal endoscopic appearance in 2 of 3 histologically diagnosed EoE cases [10]. Also, a study conducted in El-Minia University found only 4 of 6 patients (1.8%) endoscopically diagnosed with EoE matched the histopathological findings of EoE (15 eosinophils/ HPF) [20].
Historically, the diagnosis of EoE was often overlooked in adults with many patients alternatively diagnosed as having GERD or a Schatzki ring. In some instances, these patients had undergone repeated endoscopies prior to accurate diagnosis [29]. Another historical explanation for the delayed diagnosis of EoE is that eosinophilic infiltrate in the esophageal mucosa was previously associated with GERD [30]. The current strategy for making this distinction is to rely on a quantitative threshold of eosinophilic infiltration (currently ≥15/HPF in the area of greatest eosinophilic infiltration); lower counts are presumed related to GERD whilst higher counts are diagnostic of EoE [23].
GERD is extremely common, with an incidence of 10 to 20% in Western adults presenting with reflux symptoms and heartburn [31], and is the most common disease in patients referred for upper endoscopy [32]. The prevalence of GERD in our patients was 34%. In the 36 cases of EoE, 23 cases (63.9%) had also features of GERD. The overlap between GERD and EoE continues to be unknowable because of the high prevalence of GERD in the adult population.
It is now suggested that EoE is more prevalent among GERD patients who do not respond to treatment with PPIs [33]. An initial trial of PPI therapy in patients with clinical, endoscopic and pathologic findings of EoE is thus necessary. Lack of a response to PPI may reinforce a diagnosis of EoE, but a clinical response to PPI may not rule out EoE.
In current study, about 62% of patients were taken proton pump inhibitors for 8 weeks with no response to PPI. An An Egyptian study, was conducted at Al Kasr Al-Ainy hospitals showed 65 (71%) gave history of use of PPIs and 26 (28.5%) gave history of use of h2RA [10].
Conclusion
In conclusion, Eosinophilic Esophagitis is rather common among patients with GERD particularly with those presenting with dysphagia, interractable with severe persistant symptoms of GERD. Such patients may do or don’t respond to PPI should undergo UGIT endoscopy with multiple biopsies taken to exclude EoE.
Acknowledgment
We acknowledged the help of all staff in endoscopic unit of Suez Canal University hospital.
References
- Liacouras CA, Furuta GT, Hirano I, et al. Eosinophilic esophagitis: Updated consensus recommendations for children and Journal of Allergy and Clinical Immunology. 2011; 128: 3-20.
- Eosinophilic gastrointestinal disorders (EGID). J Allergy Clin Immunol. 2004; 113: 11-28.
- Potter JW, Saeian K, Staff D, et Eosinophilic esophagitis in adults: an emerging problem with unique esophageal features. Gastrointest Endosc. 2004; 59: 355-361.
- Fox VL, Nurko S, Furuta GT. Eosinophilic esophagitis: It’s not just kid’s Gastrointestinal Endos. 2002; 56: 260-270.
- Desai TK, Stecevic V, Chang CH, et al. Association of eosinophilic inflammation with esophageal food impaction in adults. Gastrointest Endosc. 2005; 61:795-801.
- Dobbins JW, Sheahan DG, Behar Eosinophilic gastroenteritis with esophageal nvolvement. Gastroenterology. 1977; 72:1312-1316.
- Attwood SE, Smyrk TC, Demeester TR, et al. Esophageal eosinophilia with dysphagia. A distinct clinicopathologic syndrome. Dig Dis Sci. 1993; 38: 109-116.
- Straumann A, Simon HU. Eosinophilic esophagitis: escalating xxx Original article epidemiology?. J Allergy Clin Immunol. 2005; 115: 418-419.
- Straumann A, Aceves SS, Blanchard C, et Pediatric and adult eosinophilic esophagitis: similarities and differences. Allergy. 2012; 67: 477-490.
- Hunter S, Helmy D, Zayed N, et Eosinophilic esophagitis in Egyptian adult patients presenting with upper gastrointestinal symptoms. Open Journal of Gastroenterology. 2014; 4: 88-95.
- Rothenberg Biology and treatment of eosinophilicesophagitis. Gastroenterology. 2009; 137: 1238-1249.
- Aceves SS, Newbury RO, Dohil R, et al. Esophageal remodeling in pediatric eosinophilic esophagitis. J Allergy Clin Immunol. 2007; 119: 206-212.
- Dellon ES, Chen X, Miller CR, et al. Tryptase staining of mast cells may differentiate eosinophilic esophagitis from gastroesophageal reflux disease. Am J Gastroenterol. 2011; 106: 264-271.
- Furuta GT, Liacouras CA, Collins MH, et al. Eosinophilic esophagitis in children and adults: a systematic review and consensus recommendations for diagnosis and treatment. Gastroenterology. 2007; 133: 1342-1363.
- Sherrill JD, Rothenberg Genetic dissection of eosinophilic esophagitis provides insight into disease pathogenesis and treatment strategies. J Allergy Clin Immunol. 2011; 128: 23- 32.
- Liacouras CA, Furuta GT, Hirano I, et al. Eosinophilic esophagitis: updated consensus recommendations for children and adults. J Allergy Clin Immunol. 2011; 128: 3-20.
- Sgouros SN, Bergele C, Mantides Eosinophilic esophagitis in adults: a systematic review. Eur J Gastroenterol Hepatol. 2006; 18: 211-217.
- Baruah, B. Kumar T, Das P, et al. Prevalence of eosinophilic esophagitis in patients with gastroesophageal reflux symptoms : A cross-sectional study from a tertiary care hospital in North India. Indian Journal of Gastroenterology. 2017; 36: 353-360.
- Sá CC, Kishi HS, Silva-Werneck AL, et al. Eosinophilic esophagitis in patients with typical gastroesophageal reflux disease symptoms refractory to proton pump Clinics (Sao Paulo). 2011; 66: 557-561.
- Magdy Fouad, Hamdy Ahmed Mokareb, Elham Ahmed Mohamed, et al. Prevalence of Eosinophilic Esophagitis in Adult Patients with Upper Gastrointestinal Symptoms in a Locality in Upper Egypt.Clin Endosc. 2018; 51: 358-359.
- Markowitz JE, Spergel JM, Ruchelli E, et Elemental diet is an effective treatment for eosinophilic esophagitis in children and adolescents. American Journal of Gastroenterology. 2003; 98: 777-782.
- Brown-Whitehorn TF, Spergel The link between allergies and eosinophilic esophagitis: Implications for management strategies. Expert Review of Clinical Immunology. 2010; 6: 101-109.
- Furuta GT, Liacouras CA, Collins MH, et al. Members of the First International Gastrointestinal Eosinophil Research Symposium (FIGERS) Subcommittees. Eosinophilic esophagitis in children and adults: A systematic review and consensus recommendations for diagnosis and treatment. Gastroenterology. 2007; 133: 1342-1363.
- Klauser AG, Schindlbeck NE, Muller-Lissner Symptoms in xxx Original article gastro-oesophageal reflux disease. Lancet. 1990; 335:205-208.
- Croese J, Fairley SK, Masson JW, et al. Clinical and endoscopic features of eosinophilic esophagitis in adults. Gastrointest Endosc. 2003; 58: 516-522.
- Kapel RC, Miller JK, Torres C, et Eosinophilic esophagitis: a prevalent disease in the United States that affects all age Gastroenterology. 2008; 134: 1316-1321.
- Kim HP, Vance RB, Shaheen NJ, et al. The prevalence and diagnostic utility of endoscopic features of eosinophilic esophagitis: a meta-analysis. Clin Gastroenterol Hepatol. 2012; 134: 1316-1312.
- Dellon ES, Gibbs WB, Fritchie KJ, et Clinical, endoscopic, and histologic findings distinguish eosinophilic esophagitis from gastroesophageal reflux disease. Clin Gastroenterol Hepatol. 2099; 7: 1305-1313.
- Remedios M, Campbell C, Jones DM, et al. Eosinophilic esophagitis in adults: Clinical, endoscopic, histologic findings, and response to treatment with fluticasone propionate. Gastrointestinal Endoscopy. 2006; 63; 3-12.
- Morrow JB, Vargo JJ, Goldblum JR, et al. The ringed esophagus: Histological features of American Journal of Gastroenterology. 2001; 96; 984-989.
- Dent J, El-Serag HB, Wallander MA, et al. Epidemiology of gastroesophageal reflux disease: A systematic review. 2005; 54; 710-717.
- Voutilainen M, Sipponen P, Mecklin JP, et Gastroesophageal reflux disease: Prevalence, clinical, endoscopic and histopathologic findings in1,128 consecutive patients referred for endoscopy due to dyspeptic and reflux symptoms. Digestion. 2000; 61: 6-13.
- Molina-Infante J, Ferrando-Lamana L, Mateos-Rodriguez JM, et al. Overlap of reflux and eosinophilic esophagitis in two patients requiring different therapies: A review of the World Journal of Gastroenterology. 2008; 14: 1463- 1466.