Epidemiological Profile and Management of Intestinal Occlusions of Cancer Origin in Three Hospitals in the City of Douala
Author'(s): Jean Paul Engbang1,2, Basile Essola1, Bekolo Fouda1,3, Sosthene Baira1 and Marcelin Ngowe Ngowe1
1Faculty of Medicine and Pharmaceutical Sciences, the University of Douala, Douala-Cameroon.
2Laquintinie hospital of Douala, Douala-Cameroun.
3Douala Military 2nd Region Hospital.
*Correspondence:
Jean Paul Engbang, Faculty of Medicine and Pharmaceutical Sciences, the University of Douala, Douala-Cameroon.
Received: 15 January 2021; Accepted: 05 February 2021
Citation: Engbang JP, Essola B, Fouda B, et al. Epidemiological Profile and Management of Intestinal Occlusions of Cancer Origin in Three Hospitals in the City of Douala. Cancer Sci Res. 2021; 4(1): 1-10.
Abstract
Background: Malignant bowel obstruction (MBO) is the complete cessation of physiological intestinal transit made up of matters and gases for more than 24 hours having as etiology an obstructive malignant neoplasia, which may be intra or extra abdominal. It requires a specific diagnostic evaluation and multidisciplinary care. MBO is not only less frequent in our context but little update are known about the disease, hence the interest of our work.
Objective: to study the epidemiological profile and management of MBO in three hospitals in the Douala city.
Methodology: This was a transversal analytical study with collected retrospective data collection over a period of 10 years, ranging from January 2010 to December 2019 within eight months. The study, which took place in three hospitals in Douala’s city, had included the complete files of admitted patients and management of MBO with evidence of histological malignancy. Patients who had been managed out of our study sites as well as those who died before treatment and incomplete records were excluded. Results analysis is done statistically using sphinx plus2 version 5.0 and Microsoft Excel 2016 software. Results means from the experiment were compared using chi2 variable comparison. P<0.05 is taken as statistically significant with a confidence interval of 95%.
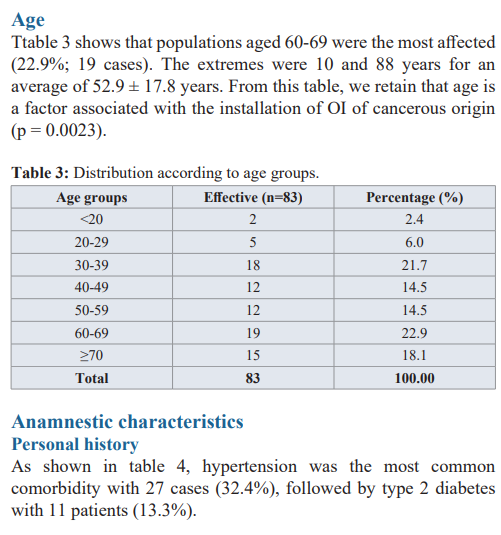
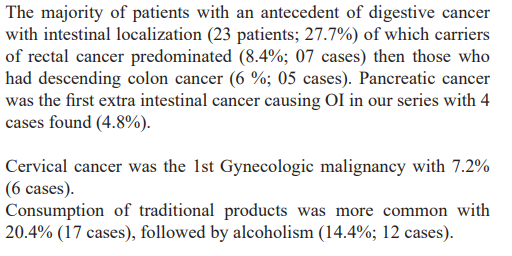
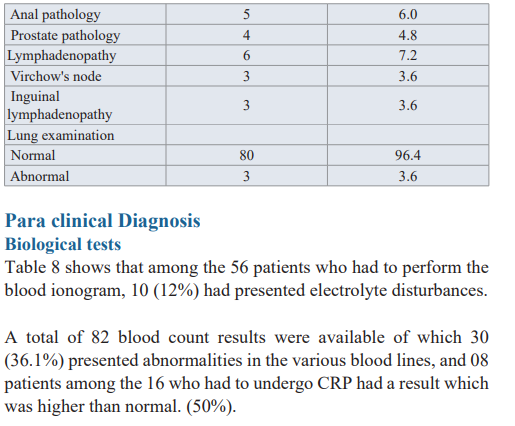
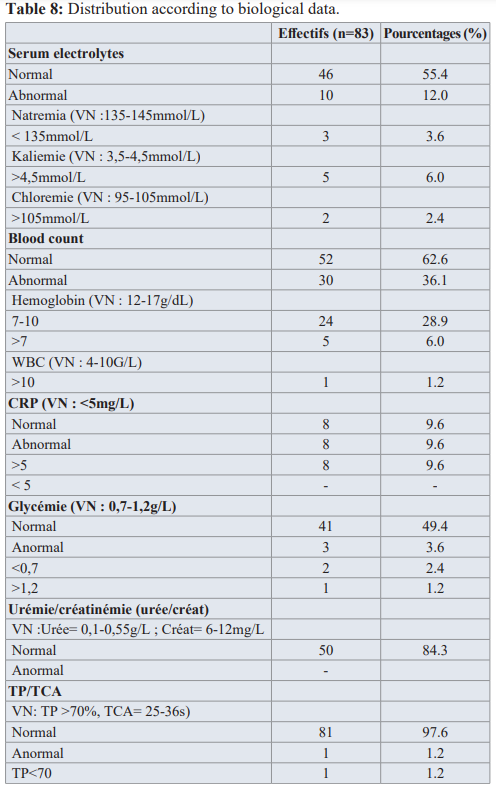
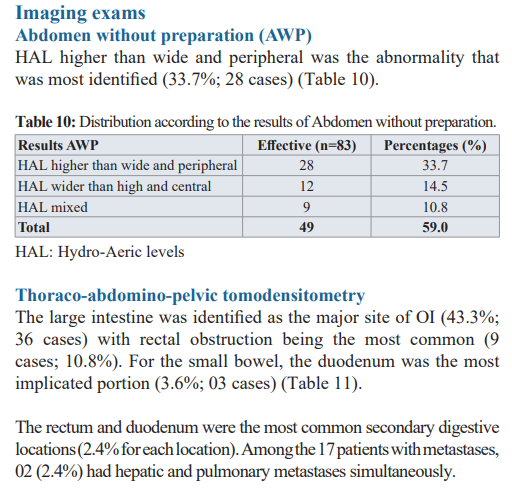
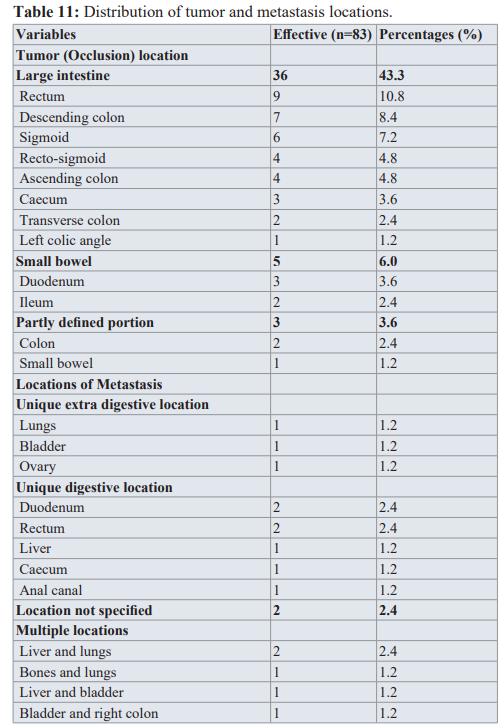
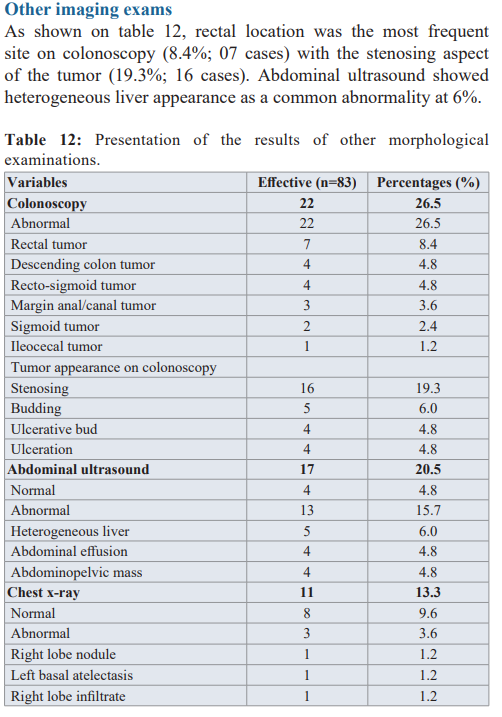
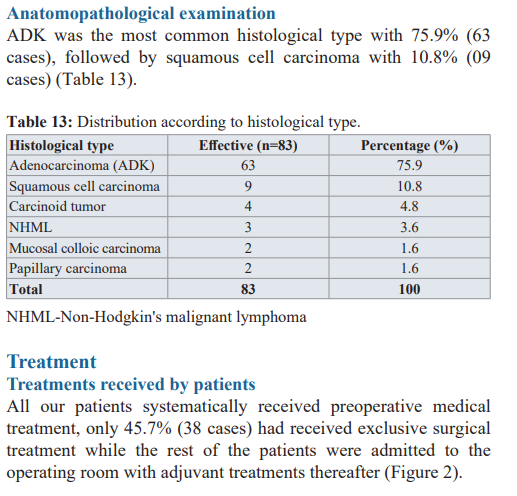
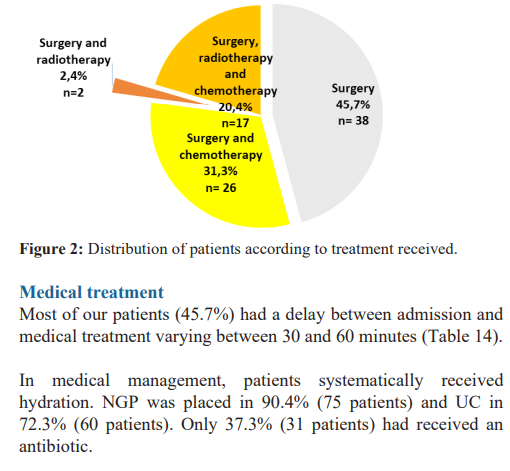
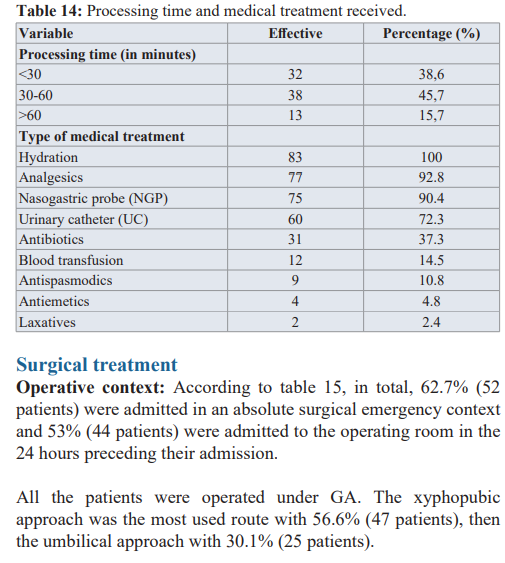
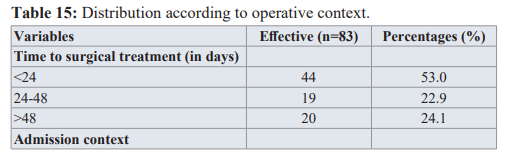
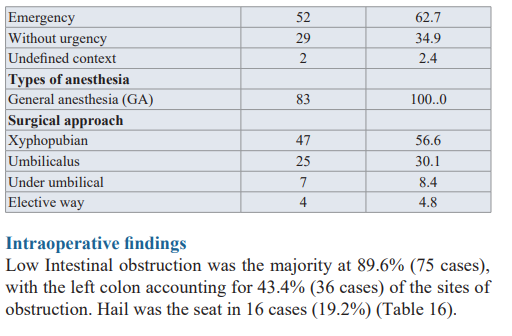
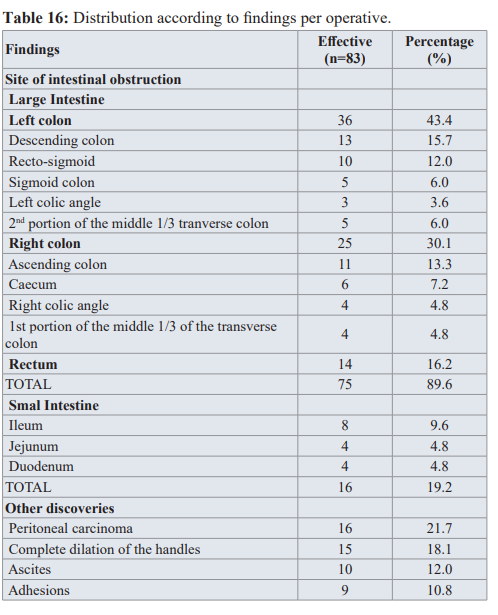
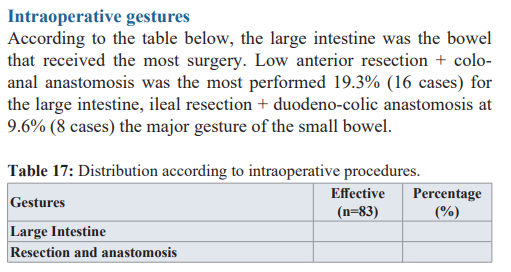
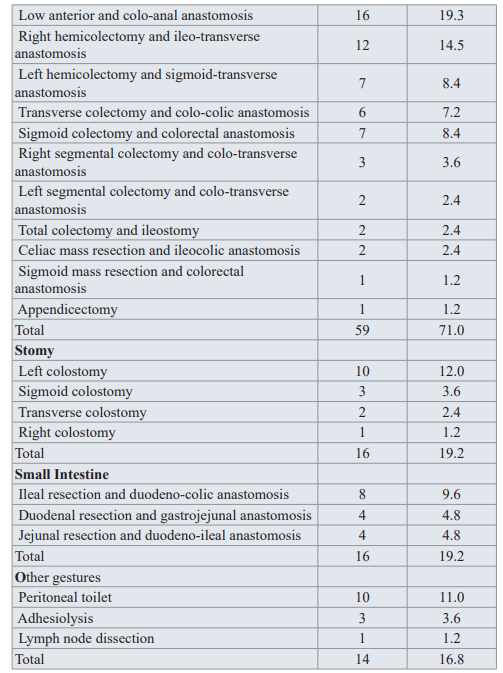
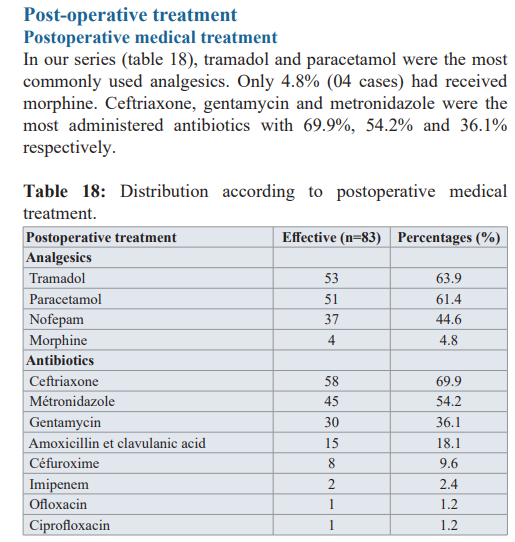
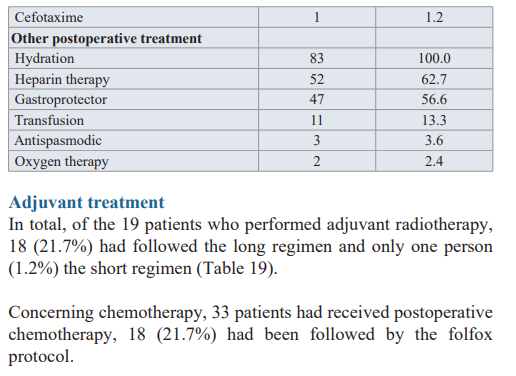
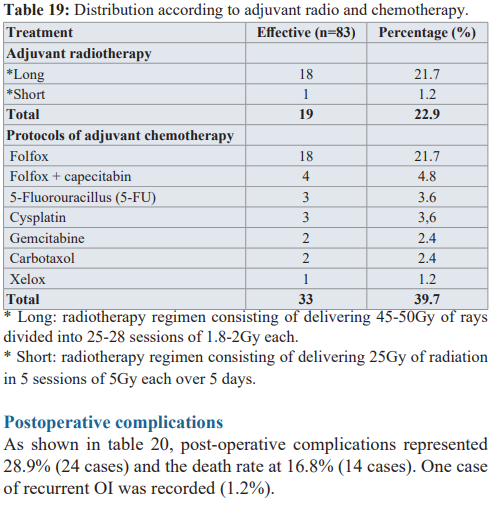
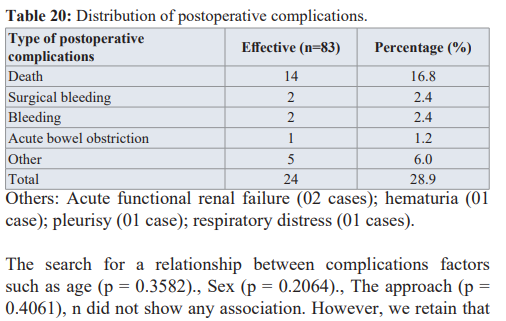
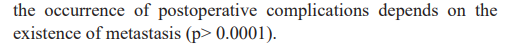
Results: We recruited 83 MBO cases. The hospital prevalence was 3.3% with a male predominance of 53% and the male / female sex ratio was 1:1. The mean age was 52.9 ± 17.8 years with the most affected being subjects from 60 years of age. Abdominal pain was the main reason for consultation (95.2%; 79 cases). Overall, 2.4% (03 cases) of our population were admitted with a state of hemodynamic instability and only 1.2% (01 case) was feverish. Meteorism was the most constant physical sign (81.9%; 68 cases). The X-ray examination of the abdomen was one of the most prescribed morphological tests (40.3%) but the thoraco-abdomino-pelvic scanner was most reliable for its precision of the occlusion site by obstructive mass with an reliability at 70.4% (p> 0.0001). The left colon was the majority obstruction site (43.4%). Intestinal resection with anastomosis was the most commonly performed surgical procedure (71%; 59 cases). In addition to surgical treatment, 31,3% of our population study benefited from exclusive chemotherapy, 2,4% from adjuvant radiotherapy and 20,4% from concomitant radio and chemotherapy. Post-operative morbidity was represented by infections and bleeding from operative wound (2.4% respectively) and recurrence of bowel obstruction. Post-operative mortality rate of 16.8% was dependent on the existence of metastases (p> 0.0001).
Conclusion: Malignant bowel obstruction is generally more frequent among aged people with a male predominancy. Surgery is the essential treatment with adjuvant methods. The prognosis is pejorative especially in the presence of metastases. Therefore, we recommend strengthening the monitoring of patients having a cancer to increase their life expectancy.
Keywords
Introduction
Acute intestinal obstruction (AIO) is one of the most common pathologies in emergency digestive surgery [1]. Several etiologies are at the origin of AOI, including mechanical and functional causes. In patients with predominantly late abdominopelvic tumors, AOI is a common complication [2-4]. The worldwide prevalence of OI on tumors varies between 3 and 15% with a higher risk in older subjects, males and especially carriers of intestinal cancer [5]. Primary intra-abdominal cancers causing AOI are mainly those of the colon (25% to 40%), followed by the ovaries (16% to 29%) and those of extra-abdominal origin causing OI are those of the breast (2% to 3%) and melanoma (3%) [5]. Affected subjects have a poor life expectancy. In the United States, for example, 17.5% of patients hospitalized for ovarian cancer develop AOI while in Spain; the 30-day mortality rate is 25% with a median survival rate of 7 months [5,6]. Colorectal adenocarcinoma is the primary cancer most implicated in malignant AOI (55%) in China [7]. Long considered the preserve of high-income countries, cancer is no longer spared in Africa today. In Africa, the diagnosis of cancer is most often made late, especially digestive cancers, sometimes at the AOI stage. This is due to the fact that the inaugural symptomatology is sometimes trivialized by the patient but also by the lack of screening means in some hospitals in addition to the poverty that reigns in the cradle of humanity [8,9]. Thus, according to the World Health Organization (WHO), cancer is a public health problem in the African region [10]. In Morocco, the main primary tumors causing AOI are predominantly digestive at 92.85% followed by gynecological tumors with 3.57% [11]. On average, 30% of patients with left colon cancer manifest their pathology by OI in the Maghreb while the mode of revelation of colorectal cancer is 53.3% in Nigeria and postoperative mortality 9.5% in Ivory Coast [11-14]. In Cameroon, Ngowe et al. report AOI of small bowel by tumor in the elderly subjects in 2010 in Yaoundé over ten years of recruitment [15]. Unlike other etiologies of OI giving a picture of abrupt acute abdomen, malignant OI sets in in a sneaky form after a few weeks or even months [2,5]. Symptoms include nausea, vomiting and abdominal pain with cessation of materials and gas within the previous 72 hours until a typical acute abdominal picture develops [5,16]. An abdominal x-ray is sufficient in most cases to suggest OI, CT scan and other x-ray examinations increase diagnostic accuracy [5,17]. Cancerous OI usually indicates a poor prognosis. Possible treatment principles include surgery which is the main measure that restores digestive transit, endoscopy, symptomatic medical treatment and anti- cancer treatment after clearing [5,14,18,19]. In Douala, the work of England et al. has long explored the epidemiological and histological characteristics of cancers of the small intestine and colon without, however, emphasizing the OIs that these can induce [20,21]. In view of these data, we therefore proposed to deepen our knowledge of the cancer etiology of OI being not only infrequent but also little explored in our context, hence our interest in carrying out a study on the epidemiological profile and treatment of OI of cancerous origin in three hospitals in the city of Douala.
Material and Methods
This was a transversal analytical study with collected retrospective data collection over a period of 10 years, ranging from January 2010 to December 2019 within eight months. The study, took place in surgery, operating theater, oncology and pathological anatomy departments of three hospitals in Douala’s city in Cameroon (Douala Laquintinie Hospital, Douala General Hospital, Douala Military 2nd Region Hospital), and included the complete files of admitted patients and management of MBO with evidence of histological malignancy. Patients who had been managed out of our study sites as well as those who died before treatment and incomplete records were excluded. The variables studied were socio-demographic data, clinical and Para clinical data, treatment and postoperative complications. Results analysis is done statistically using sphinx plus2 version 5.0 and Microsoft Excel 2016 software. Results means from the experiment were compared using chi2 variable comparison. P<0.05 is taken as statistically significant with a confidence interval of 95%.
Results
Epidemiology Frequency of major abdominal emergencies
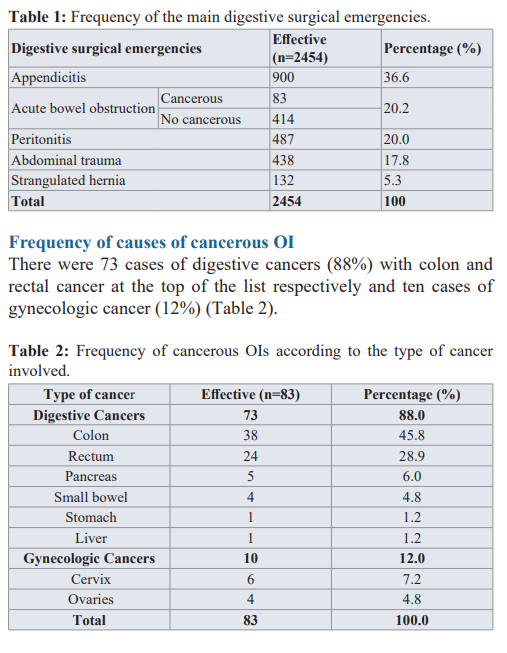
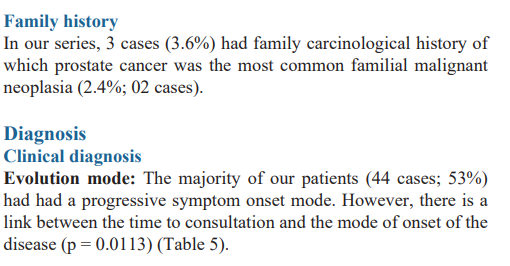
As shown in table 1, we found 2454 files of patients operated on for acute abdomen. Acute bowel obstruction represented the second digestive surgical emergency (497 cases; 20.2%) of which 83 cases were of cancerous origin, the hospital prevalence being 3.3% (prevalence = study population selected / abdomen population treble * 100).

Discussion
In 2010 and 2012, the prevalence of cancerous OI was in the range 3-15% [5,22]. During our study, it was around 3.3%, which brings us closer to the data in the literature.
In our series, both sexes were largely represented with a slight male predominance: 44 cases (53%) against 39 (47%) for the female sex. This same observation had been made by other authors. Thus, in the American continent, especially in Canada and the United States, Chakraborty and Dalal found this male predominance, i.e. 54.3% and 55% respectively [23,24]. Kim et al. also identified a male preponderance in South Korea at 73.9% [25]. Likewise, in Europe, Delgado et al. found the male sex to be 66% dominant [26]. Kaissi in 2019 found 75% in North Africa, as did Abudu et al. in 2016 in West Africa (57.7%) [12,13]. In South Africa, Moola et al. found male predominance at 57.1% in 2014 [27]. Our results are similar to those of previous studies.
The average age of our patients was 52.9 years. This finding is confirmed with other studies done in Africa, in which the average age was also in the fifties precisely 56 years in North Africa, 55.9 years in West Africa and 59 years in South Africa [11,13,27]. These results diverge from series made in other continents where the average age was older. In South Korea, a study reports 62.8 years, 61 years in North America and 67.3 years in Europe [23,25,26]. Indeed, this age difference of African stories with other continents is explained by the life expectancy which is higher in these continents compared to ours, particularly in Cameroon where life expectancy is estimated on average. at 55 years old [28].
Subjects aged 60-69 years represented the population most affected in our work (22.9%; 19 cases). This same observation was made in Nigeria in 2015 and also in South Asia: Abudu et al. 28.9% for the 61-70 years age group, 29.7% for the 60-69 age group according to Mohd et al. [13,29]. Indeed, according to Engbang et al, subjects over 50 years of age are more at risk of developing colon cancer [21]. So having this entity, they are more likely to manifest an occlusive syndrome with primary intestinal cancer as the etiology.
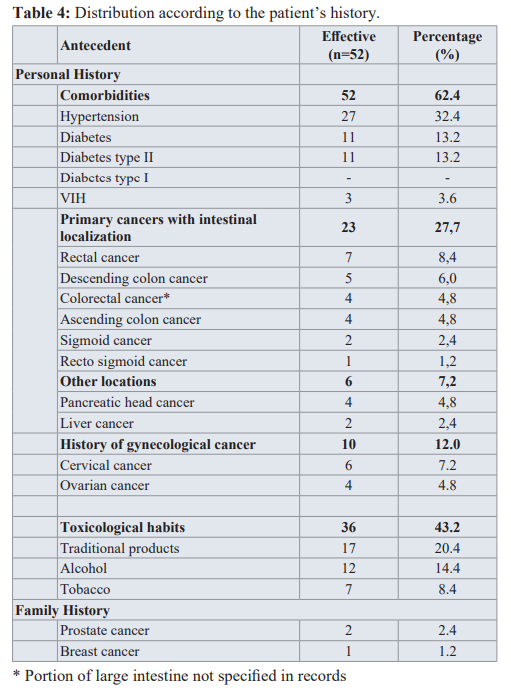
During the course of their neoplastic disease, in 28% of patients with colorectal cancer (CRC), OI occurs justifying a surgical procedure, the CRC would thus increase the occurrence of IO [28]. In our analysis, it emerged that among the 29 patients dead of digestive cancer, 23 (27.7%) had known primary intestinal cancer (colon or rectum). Indeed, the work of Hsu and his collaborators in 2019 in the United States, had shown that 8-29% of patients with CRC developed OI, and in Europe 10-29% were identified [5,30]. In North Africa, Bouchra also found in his series 29% of patients with history of primary digestive cancer [11]. Our results are therefore similar with the work carried out previously and this would therefore confirm that the existence of a primary digestive neoplasia is a possible factor in the development of intestinal obstruction, especially when it is localized at the colorectal level.
After colorectal cancers, gynecological neoplasias and particularly those of the ovary, uterus and endometrium are considered to be the first secondary cancers causing intestinal obstructions. In our case, 12% of the population had history of gynecological cancers. We have noticed that this proportion tends to be closer to the Moroccan data which related 19% but the difference is important compared to other continents [11]. Particularly in France, 21.8% are reported according to Prost à la Dénise et al, while in China this rate is 28% according to Tsai et al. [31,32]. This could be explained by the fact that our study was done in a poorer country as compared to others. The population then has little financial means to carry out regular screening examinations for gynecological cancers.
Certain toxic products are also involved in the genesis of precancerous lesions, such as alcohol and tobacco, for example. We found that 8.4% of our population were smokers and 14.4 %% alcohol users. These proportions were divergent from those of the Maghreb [11]. Indeed, North Africa being predominantly Muslim, alcohol is prohibited and this is not the case in Central Africa and particularly in the city where our study was made. Unfortunately for the other authors, the traditional product component had not been studied so that we could make a comparison.
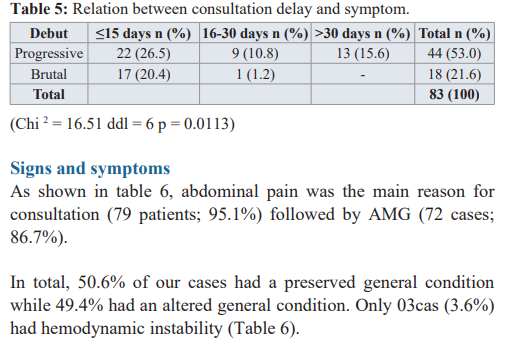
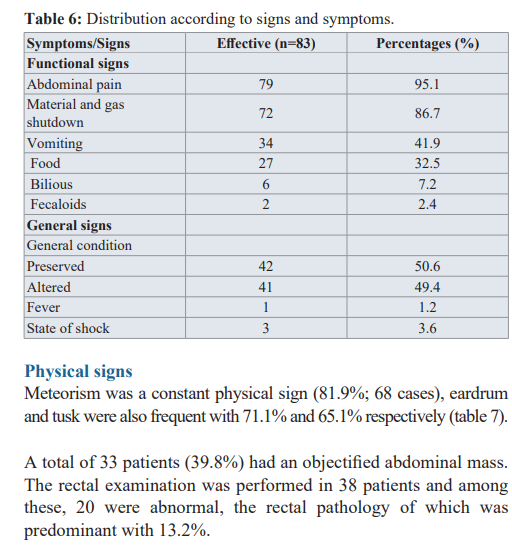
Abdominal pain is a common functional sign caused by abdominal distension or a tumor mass invading or compressing the intestine [4,11]. It was found in our series in 95.1% (79 cases) as in Bouchra who also found a frequency of 93% in Morocco [11]. Western series report a slightly low frequency: 80% according to Laval et al. in France, 72-80% according to Tuca et al. in Spain [5,33]. We note that the frequency of abdominal pain is higher in African series compared to those of Westerners, because the majority of Africans tend to trivialize the symptoms and only go to hospitals when the pain becomes unbearable or unmanageable by traditional practitioners. Like abdominal colic, vomiting is classic in occlusive syndrome, but it can be intermittent or continuous. Their frequencies as well as their abundance will be the cause of probable dehydration. In our study, they were present in 41% (34 cases) with the most frequent food content with 32.5%. Ripamonti et al. described a frequency between 68-100% in 1993, Dean et al. 62% while Ferguson et al. reported 87-100% in 2015 as well as Bento de Sousa et al. in 2019 [4, 34-36]. This difference with the Western and American series is argued by the fact that in the event of low IO vomiting can be observed late and the majority of our patients had colonic obstruction (85.2%). Stopping transit is the master of symptoms but stopping gas has a high semiological value [11]. In our study, matter and gas arrest (AMG) was noted in 86.7% (72 cases). Tuca et al. found AMG in 85-93% in 2012, as did Ferguson et al. in 2015 as well as Bento de Sousa et al. in 2019 [5,34,36]. Our results therefore go hand in hand with those of the literature.
Meteorism is a major sign of OI [5,37]. We report 68 cases in our series, i.e. a rate of 81.9%. This rate is close to those of the Spanish (56-90%), Moroccan (95%) and French (86%) stories [5,11,33]. Rectal examination (DRE) is mandatory in OI, to confirm rectal emptiness and rule out obstruction by faecal impaction or rectal mass [36]. In our study, 20 patients had pathological TR (24.1%) of which 11 had rectal tumor (13.2%). This rate matches that of the study in the Maghreb which reported 16% [11].
The management of OI with cancerous etiology is multidisciplinary [5,23]. Once diagnosed with OI, oral nutrition and hydration are stopped [33]. The surgical technique depends on the patient's condition, the findings during the operation and the surgeon's preference [32].
In our series, 45.7 %% of the selected population had received surgical treatment only. Other African series yielded 84% and 100% while Western studies reported lower figures, 24% in Great Britain and 8.3% in Canada [9,11,23,35]. This statistical difference in African figures from other continents could be elucidated by the fact that cancer patients are very well followed, and probably have little chance of having complete intestinal obstruction in these developed countries compared to African patients who are little followed, either by the lack of specialized doctors, or by an inadequate technical platform for better follow-up or by the ignorance and poverty of the patients.
Only 31.3% of the patients in our study benefited from adjuvant chemotherapy, 2.4% from radiotherapy and 20.4% from concomitant radiochemotherapy postoperatively. In Morocco, adjuvant chemotherapy was performed in 38.1%, radiotherapy 1% and the combination radio chemotherapy 7% [11]. Very high frequencies have been reported in America, i.e. 83.8% surgery associated with adjuvant chemotherapy and 22.8% surgery with postoperative radiotherapy in Brazil, 78% postoperative chemotherapy and 31% adjuvant radiotherapy in the United States [24,34]. The statistical discrepancy with the American series could be explained by the lack of universal health coverage in our context. Added to this is the poverty that reigns within our populations in order to be able to follow adjuvant treatment under optimal conditions, and also the lack of specialist doctors.
Conclusion
In the light of this work carried out on 83 cases of intestinal obstruction of cancerous origin over a period of 10 years in the city of Douala, it emerges that the pathology appeared to be that of predominantly male elderly subjects with cancer, colon as the main etiology. Its diagnosis being both clinical and paraclinical, abdominal pain was the most constant functional sign and abdominal meteorism the most frequent physical sign. PSA was the most prescribed x-ray examination, but the thoraco-abdominopelvic scan was more reliable for the accuracy of the site of obstruction by the cancerous mass. His surgical management consisted of performing intestinal resection with anastomosis in most cases. Half of the patients had received adjuvant treatment based on exclusive chemotherapy, single radiotherapy or a concomitant combination of radio and chemotherapy. The prognosis is poor especially in the presence of metastases, hence the severity of the pathology related to the poor ground on which it occurs.
References
- Aslar AK, Ozdemir S, Mahmoudi H, et al. Analysis of 230 cases of emergent surgery for obstructing colon cancer lessons J Gastrointest Surg. 2011; 15: 110-119.
- Guirimand F. Prise en charge des occlusions intestinales chez des patients atteints de cancer en phase avancée. Méd pal. 2003; 2: 197-210.
- Ripamonti C, Easson AM, Gerdes Management of malignant bowel obstruction. Eur J Cancer. 2008; 44: 1105-1115.
- Ripamonti C, De Conno F, Ventafridda V, et al. Management of bowel obstruction in advanced and terminal cancer Ann oncol. 1993; 4: 15-21.
- Tuca A, Guell E, Martinez-Losada E, et Malignant obstruction in advanced cancer patients epidemiology management and factors influencing spontaneous resolution. Cancer management and research. 2012; 4: 159-169.
- Mooney SJ, Winner M, Hershman DL, et Bowel obstruction in elderly ovarian cancer patients a population-based study. Gynecologic oncology. 2013; 129: 107-112.
- Jia-hong C, Tzu-chuan H, Ping-ying C, et Malignant bowel obstruction A retrospective clinical analysis. Mol clin oncol. 2014; 2: 13-18.
- Oulahrir Cancers du côlon gauche en occlusion à propos de 20 cas thèse de médecine. Fes Université Sidi Mohammed ben abdellah. N°141. 2016 ; 146.
- Alliance des Ligues Africaines et Méditerranéennes contre le cancer Les cancers en Afrique francophone. Brazaville La ligue nationale contre le cancer. 2017; 136.
- World health organization. Cancer prevention and control a strategy for the WHO african region. Yaoundé. 2008 ;
- Bouchra Les occlusions intestinales d’origine tumorale thèse de médecine. Marrakech Université Kadi Ayyad. N°75. 2014 ; 260.
- Soumaya Cancers coliques gauche en occlusion thèse de médecine. Marrakech Université Mohammed V. N° 387. 2019 ; 118.
- Abudu EK, Akinbami OS. Colorectal Carcinomas in Uyo City Southern Geopolitical Zone of Nigeria A Review of Clinicopathological Characteristics and Rare tumors. 2016; 8: 61-75.
- Kouadio GK, Turquin Cancers coliques gauche en occlusion en Côte d’Ivoire. Ann chir. 2003; 128: 364-367.
- Ngowe NM, Ngo NB, Mouafo TF, et al. occlusion du grêle par lipome sous muqueux chez le sujet âgé. Revue africaine de chirurgie et spécialités. 2010; 4: 39-41.
- Cappell MS, Batke M. Mechanical Obstruction of the Small Bowel and The medical clinics of north America. 2008; 92: 575-597.
- Lowell B. Anthony, Aman Chauhan. Diarrhea Constipation and Obstruction in Cancer Management. Dans The MASCC Textbook of Cancer Supportive Care and Second Edition. Adelaide. Springer. 2018; 421-436.
- Miller G, Boman J, Shrier I, et al. Small-bowel obstruction secondary to malignant disease an 11-year audit. Can J Surg. 2000; 43: 353-358.
- Rouibaa F, Bakkar M, Seddik H, et al. Intérêt des prothèses métalliques expansives dans la prise en charge de l’occlusion tumorale colique: expérience d’un service hospitalier Pan african medical journal. 2013; 14: 1-5.
- Engbang JP, Eloumou S, Fewou A, et epidemiological and histopathological features of small intestine cancer in Cameroon about 47 cases. Cancer research journal. 2019; 7: 136-142.
- Engbang JP, Fewou A, Hasigov A, et Colon Cancers epidemiological and histopathological aspects in Cameroon. Journal of cancer and tumor international. 2018; 7: 1-13.
- Tuca A, Martinez E, Güel E, et Malignant bowel obstruction. Med Clin. 2010; 135: 375-381.
- Chakraborty A, Selby D, Gardiner K, et al. Malignant Bowel Obstruction Natural History of a Heterogeneous Patient Population Followed Prospectively Over Two Years. J Pain Symptom 2011; 41: 412-420.
- Dalal MK, Gollub JM, Miner TJ, et Management of Patients with Malignant Bowel Obstruction and Stage IV Colorectal Cancer. Journal of palliative medicine. 2011; 14: 822-828.
- Kim DH, Kim B, Choi HJ, et Tumor characteristics associated with malignant large bowel obstruction in stage IV colorectal cancer patients undergoing chemotherapy. Int J Colorectal Dis. 2016; 31: 1767-1774.
- Delgado S, Momblan D, Salvador L, et Laparoscopic assisted approach in rectal cancer patients. Surg Endosc. 2004; 18: 1457-1462.
- Moolla Z, Thandinkosi EM. Trends in Demographics and Management of Obstructing Colorectal World J Surg. 2014; 38: 2466-2470.
- Bureau central des recensements et des études de 3e recensement général de la population et de l’habitat. Yaoundé. Beta print. 2010; 52.
- Mohd MS, Wei LT, Shahrul AS, et al. Intestinal obstruction predictor of poor prognosis in colorectal Epidemiol Health. 2015; 37: 1-5.
- Hsu J, Sevak Management of malignant large-bowel obstruction. Dis colon rectum. 2019; 62: 1028-1030.
- Prost à la denise J, Douard R, Malamut G, et Small Bowel Obstruction in Patients with a Prior History of Cancer Predictive Findings of Malignant Origins. World J Surg. 2014; 38: 363-369.
- Tsai MS, Liang Surgery is justified in patients with bowel obstruction due to radiation therapy. J Gas Sur. 2006; 10: 575- 582.
- Laval G, Arvieux C, Stefani L, et Protocol for the Treatment of Malignant Inoperable Bowel Obstruction A Prospective Study of 80 Cases at Grenoble University Hospital Center. J Pain Symptom Manage. 2006; 31: 502-512.
- Bento de sousa JH, Bianchi ET, Tustumi F, et al. Surgical Management of Malignant Intestinal Obstruction Outcome and Prognostic Chirurgia. 2019; 114: 343-351.
- Dean E, Khoja L, Clamp A, et Malignant bowel obstruction in advanced ovarian cancer. Future Oncol. 2017; 13: 513-521.
- Ferguson HJM, Ferguson CI, Speakman J, et al. Management of intestinal obstruction in advanced malignancy. Ann Med 2015; 4: 264-270.
- Sidibé MB. Aspects épidémiologiques cliniques et prise en charge des occlusions intestinales aiguës mécaniques dans le service de chirurgie générale et pédiatrique du CHU Gabriel Touré thèse de médecine. Bamako Université de Bamako. 2003; 7-24.