Epidemiology and Tumor Characteristics of Gastrointestinal Stromal Tumors in Kurdistan Region of Iraq
Author'(s): Fahmi M. Salih1* and Kakil Ibrahim Rasul2
1Fahmi Mohammed Salih, M.B.Ch.B, Rizgary Oncology Center, Erbil, Kurdistan Region, Iraq.
2Kakil Ibrahim Rasul, CABM, FRCP, ESMO, National Center for Cancer Care and Research (NCCCR), Weil Cornell Medical College, Qatar.
*Correspondence:
Fahmi Mohammed Salih Fatah, Rizgary Oncology Center, Erbil, Kurdistan Region, Iraq, E-mail: fzebary@yahoo.com.
Received: 26 February 2018 Accepted: 24 March 2018
Citation: Fahmi M. Salih, Kakil Ibrahim Rasul. Epidemiology and Tumor Characteristics of Gastrointestinal Stromal Tumors in Kurdistan Region of Iraq. Gastroint Hepatol Dig Dis. 2018; 1(1): 1-4.
Abstract
Objective: To estimate the incidence and tumor characteristics of gastrointestinal stromal tumors admitted to Kurdish oncology centers located in north of Iraq. Patients & Methods: A retrospective study of 169 patients diagnosed with GIST who have been managed in four oncology centers in Kurdistan region of Iraq during the past eight years. Patient and tumor characteristics were analyzed by a statistician using IBM SPSS 24 to assess the incidence of GIST.
Results: Among one hundred sixty nine patients, 50.3% (n=85) were male and 49.7% (n=84) were female. The most common primary site was stomach while esophagus was the least frequently affected location. The median age was 56.2 years (20-93 years). Morphologically they were Spindle cell type in 68.6%, epithelioid type in 8.9%, mixed type in 20.7%. 53% of cases were categorized as high risk tumors, 23% as intermediate risk, 19% as low risk and 5% were not categorized. There was a steady rise of the number of GIST cases from
2010 (n=7) to 2017(n=30).
Conclusion: The incidence of gastrointestinal stromal tumors in Kurdistan region is increasing. It is not clear whether this is a true increment or is due to a better identification of GIST cases in regional centers and increase in the population.
Keywords
Background
Gastrointestinal stromal tumors (GIST) are rare tumors, yet the most common mesenchymal neoplasm of the GI tract, resulting most commonly from KIT or PDGFRA activating mutations [1]. GISTs can arise along the gastrointestinal tract or outside the tubular GIT [2] including stomach (60%), jejunum and ileum (30%), duodenum (4-5%), rectum (4%), colon and appendix (1-2%), and esophagus (<1%), and rarely as apparent primary extra gastrointestinal tumors (Hereafter referred to as EGIST) [3]. Patients with a suspected GIST may clinically present with a variety of symptoms like early satiety, abdominal discomfort due to pain or swelling, intraperitoneal haemorrhage, GIT bleeding, or anemia related fatigue. Patients may present with an acute abdomen (from tumor rupture, GI obstruction, or appendicitis-like pain), which requires immediate medical attention and occasionally they are asymptomatic or incidentally found at surgery [4]. Liver metastases and/or intra-abdominal dissemination are the most common clinical manifestations of malignancy. GISTs very rarely metastasize to lymph nodes. Metastatic disease to lung or other sites beyond the abdominal cavity may occur in few advanced cases [4].
Most widely used diagnostic tools are contrast enhanced computed tomography scan, endoscopies, ultrasound, and magnetic resonance imaging. Diagnosis is confirmed by histology and immunohistochemistry. Prognosis varies by location and is generally more favorable for patients with gastric tumors than for patients with GIST of the small intestine or other less common locations. Active mutations in KIT (CD117) and PDGFRα are involved with most of the cases of GIST and can be important diagnostic markers with prognostic value [5-7].
There is an estimated 4500 to 6000 new cases of GIST in the United States each year, although incidence is difficult to determine and may vary among studies [8,9]. The reported incidence has increased because of better awareness, improved diagnostic means, and possibly an increase in the true incidence of the disease. Prevalence can also be difficult to determine; one study estimated that 129 per million people are living with GIST.
This study is intended to provide an overview of the epidemiology and tumor characteristics of GIST cases in Kurdistan region of Iraq. By conducting this study, we will gain an insight, for the first time, regarding the burden of disease in this area.
Patients and Methods
A systematic retrospective analysis of all GIST cases that have been admitted in any of the 4 oncology centres located in Kurdistan region of Iraq, namely; Rizgary Oncology center, Nanakaly cancer Hospital, Hiwa cancer center, & Azadi Teaching hospital. By getting a support letter from Kurdistan Board for Medical specialities and local Directorates of health, access granted to patient records and cancer registries in the aforementioned centres to collect the details of patients recorded over last 8 years. Kirkuk data is excluded from this study. All GIST (low or high risk) cases that are confirmed by biopsy or Immunohistochemistry are included in this study. Incomplete data and unconfirmed records were not processed. Histopathology reviewed and confirmed with Rizgary pathology lab, Shorsh hospital and Duhok central lab database. This data was analysed by a statistician form Salahaddin University in Erbil.
Results
A total number of one hundred sixty nine (n=169) patients were recorded in four cancer centres from January 2010 till December 2018. Estimated incidence is 29.6 cases per million populations. 50.3% (n=85) were male and 49.7% (n=84) were female. The median age was 56.5 years (20-93 years) with 65% of patients aged more than 50 years. 7 patients diagnosed on 2010, 11 patients on 2012, 20 patients on 2013, 24 patients on 2014, 30 patients on 2015, 25 patients on 2016 and 30 patients on 2018.
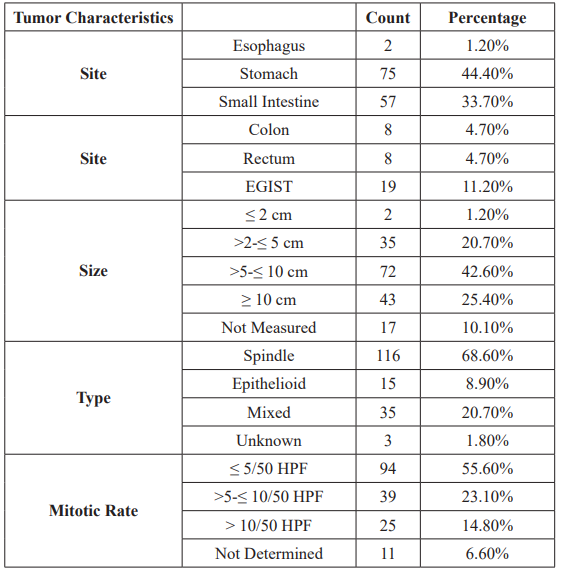
The primary tumor involved stomach in 44.4% (75) of cases, small intestine in 33.7% (57), each colon & rectum involved by 4.7% (8 cases colon, 8 cases rectum) and 11.2% of the tumors (n=19) were located outside the tubular GI tract and considered EGIST*. 68.6% of the tumors were of spindle cell type, 8.9% were Epithelioid, and 20.7% were of mixed morphologic type Table 1 shows tumor characteristics in all GIST cases. 106 tumors were regarded as high risk category, 43 were intermediate risk, 14 low risk and 6 cases were not categorized. 147 of tumors were CD119 positive, 104 were CD34 positive and 32 were S100 positive.
Discussion
Epidemiology and Demographic data
This study estimates for the first time the incidence of gastrointestinal stromal tumours in Kurdistan region of Iraq. The population of the study is distributed in three governorates; Erbil, Sulymania and Duhok, globally recognised as KRG territories. The total population of this area is estimated to be 5,700,000.
There are 169 patients diagnosed with GIST between years 2010 and 2018 with the incidence rate around 8.6 cases per million in 2018 and prevalence rate is estimated at 48.4 cases per million. The number of cases recorded in this study were 7 patients in 2010, 11 patients in 2011, doubled to 22 cases by 2012, in 2013 dropped to 20 cases, 24 cases were recorded in 2014 while 30cases, 25cases and another 30 cases for years 2015, 2016 and 2018 respectively (Figures 1-3). In literature review, the highest incidence of GIST were in Northern-Norway, Hong Kong and Shanghai reporting incidences as high as 19-22 cases per million population, which is regarded the upper range limit reported in the world literature [10- 13]. There is an overt variation in the global epidemiology of GISTs which may be due to; First, methodological issues are at hand, as the diagnostic criteria have been in development and improved over time, and, thus, variation in diagnosis and recording may have occurred. Secondly, few countries have established registries that captured all GISTs, while some cancer registries have collected data on the overt malign cases. Thus, smaller, incidental and low risk tumours may be underrepresented in several studies [10]. These two reasons are possibly attributed to the increase in number of GIST patients in our region as well. Furthermore an increase in the population of Kurdistan region could have reflected on the increase in number of patients reported. When comparing to other regional countries like Qatar for instance the GIST cases were less encountered than our locality [2,14]. The median age was 56.2 years (between 20-93 years). 65% of the patients aged more than 50 years and 35 % were ≤ 50 years. Both males (n=85) and females (84) were fairly equally affected by the tumor with slight male preponderance toward high risk group (56.6 % males versus 43.3 % females from high risk category).
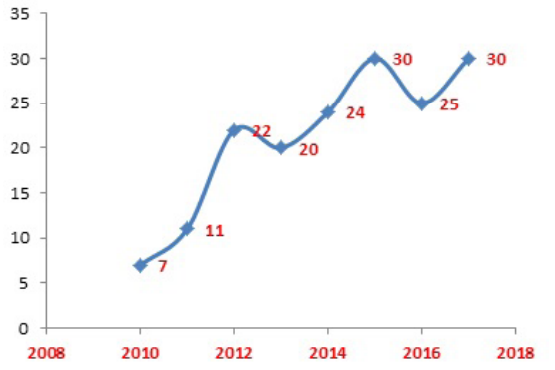
Figure 1: GIST by year of diagnosis.
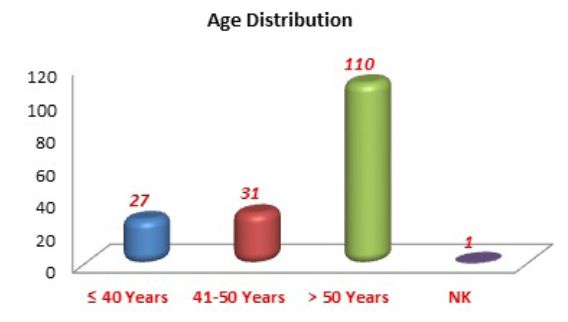
Figure 2: GIST cases by age distribution.
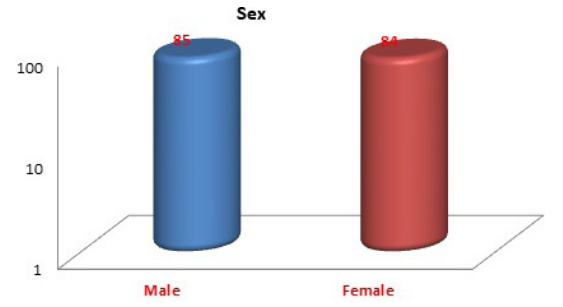
Figure 3: All GIST cases by sex.
Tumor Characteristics
Stomach was the most affected site by GIST, accounting for 44.38% ( n=75) of the cases, small intestine was involved by tumor in 33.73 % (n=57), both colon & rectum were equally affected (4.73%, 8 cases for each site). About 11.24% of the tumors were found outside the tubular GIT (EGIST) and barely 1.18% ( n=2) arise from esophagus. The morphological type, site dependent [2] to lesser degree, was spindle cell in majority of the tumors (68.64 %, n=116), Epithelioid type in 8.88 %, mixed type in 20.71 % and in 3 cases the type was not mentioned. Out of 15 epithelioid cell tumors, 10 (66.6%) involved stomach. Only 1.20% of the tumors were ≤ 2 cm in largest dimension, 20.7% were between >2-≤ 5 cm and the remaining larger number measured > 5 cm (42.60%, 25.40% for both >5-≤ 10 cm and >10 cm respectively) for which a late diagnosis have to be blamed. Table 1 shows tumor characteristics in all patients. Most of the tumors were of low mitotic activity, In 55.60% of specimens the mitotic rate was ≤ 5/50 HPF, in 23.10% ranged between >5-≤ 10/50 HPF, in 14.80% of them was > 10/50 HPF while mitotic rate was not determined in 6.60% of the tumors.
Conclusion
The incidence of gastrointestinal stromal tumours in Kurdistan region is increasing. It is not clear whether this is a true increment or is due to a better identification of GIST cases in regional centres and increase in the population.
References
- Hirota S, Isozaki K, Moriyama Y, et al. Gain-of- function mutations of c-kit in human gastrointestinal stromal tumors. 1998; 279: 577-580.
- Rasul KI, Jassoum SB, Hamad Epidemiology and clinicopathological pattern of gastrointestinal stromal tumors in Qatar. J Chinese Clin Med. 2008; 3: 117-180.
- Miettinen M, Lasota Gastrointestinal stromal tumors: pathology and prognosis at different sites. InSeminars in diagnostic pathology. 2006; 23: 70-83.
- Demetri GD, Von Mehren M, Antonescu CR, et al. NCCN Task Force report: update on the management of patients with gastrointestinal stromal tumors. Journal of the National Comprehensive Cancer Network. 2010; 8: S-1
- Heinrich MC, Corless CL, Duensing A, et PDGFRA activating mutations in gastrointestinal stromal tumors. Science. 2003; 299: 708-710.
- Lasota J, Miettinen Clinical significance of oncogenic KIT and PDGFRA mutations in gastrointestinal stromal tumours. Histopathology. 2008; 53: 245-266.
- Lasota J, Corless CL, Heinrich MC, et al. Clinicopathologic profile of gastrointestinal stromal tumors (GISTs) with primary KIT exon 13 or exon 17 mutations: a multicenter study on 54 Modern pathology. 2008; 21: 476.
- Nilsson B, Bümming P, Meis-Kindblom JM, Gastrointestinal stromal tumors: the incidence, prevalence, clinical course, and prognostication in the preimatinib mesylate era. Cancer. 2005; 103: 821-829.
- Demetri GD, Von Mehren M, Antonescu CR, et al. NCCN Task Force report: update on the management of patients with gastrointestinal stromal tumors. Journal of the National Comprehensive Cancer Network. 2010; 8: S-1.
- Søreide K, Sandvik OM, Søreide JA, et Global epidemiology of gastrointestinal stromal tumours (GIST): A systematic review of population- based cohort studies. Cancer epidemiology. 2016; 40: 39-46.
- Steigen SE, Eide TJ. Trends in incidence and survival of mesenchymal neoplasm of the digestive tract within a defined population of northern APMIS. 2006; 114: 192–200.
- Chan KH, Chan CW, Chow WH, et Gastrointestinal stromal tumors in a cohort of Chinese patients in Hong Kong, World J. Gastroenterol. 2006; 12: 2223-2228.
- Lv M, Wu C, Zheng Y, et al. Incidence and survival analysis of gastrointestinal stromal tumors in shanghai: a population- based study from 2001 to 2010. Gastroenterol. Res Pract. 2014; 834136.
- Al-Thani H, El-Menyar A, Rasul KI, et al. Clinical presentation, management and outcomes of gastrointestinal stromal tumors. International Journal of Surgery. 2014; 12: 1127-1133.