Factors to Consider for Successful Telemedicine Gastroenterology Subspecialty Visits in Disparate Populations
Author'(s): Hamid Ullah1, Landen S. Burstiner2, Lucas B. Buchanan1, Sara Iqbal3, Amor Royer1, Sarah Glover3, and Pegah Hosseini-Carroll3
1Department of Internal Medicine, University of Mississippi Medical Center, USA.
2Nova Southeastern University Dr. Kiran C Patel College of Osteopathic Medicine, Davie, FL, USA.
3Department of Digestive Diseases, University of Mississippi Medical Center, USA.
*Correspondence:
Hamid Ullah MD, Department of Internal Medicine, University of Mississippi Medical Center, USA.
Received: 05 Mar 2022 Accepted: 11 Apr 2022 Published: 16 Apr 2022
Citation: Ullah H, Burstiner LS, Buchanan LB, et al. Factors to Consider for Successful Telemedicine Gastroenterology Subspecialty Visits in Disparate Populations. Gastroint Hepatol Dig Dis. 2022; 5(1): 1-5.
Abstract
Introduction: Telemedicine was put at the forefront of the healthcare delivery process during the coronavirus disease 2019 (COVID-19) pandemic. Pre-COVID-19 research had shown telemedicine to be beneficial in the gastroenterology field with improved quality of life and reduced healthcare cost in the IBD population. However, telemedicine remained underutilized in subspecialty care with constraints at both provider and patient level.
Objective: To analyze the telemedicine encounters in a gastroenterology clinic at a tertiary care hospital and identify factors that facilitate or limit the use of telemedicine modalities.
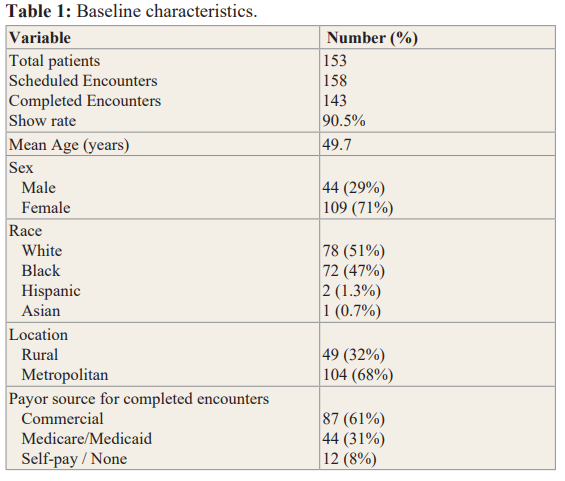
Methods: The project was a retrospective, single-center study with continuous sampling of one hundred and fifty-three patients who scheduled one hundred and fifty-eight telemedicine encounters that included both Inflammatory Bowel Disease (IBD) and general gastroenterology patients. We examined the influence of age, sex, race, geographic location and payer source, on audio or video telemedicine encounters, as well as the show rate.
Results: Our study showed a promising show rate of 90.5% with a majority of the patients preferring video over audio visits; however, increasing age proved to be a barrier in successfully completing video visits. In total, 26.2% of the patients who desired video encounters had to be switched to audio only. We found that race, sex, payor source, and living in a rural zip code did not influence the rate of completed telemedicine encounters or the patients’ preferred modality (audio vs video).
Conclusion: The recurring COVID-19 surge due to different variants provides an opportunity to refine the telemedicine experience in our healthcare. Telemedicine encounters have a promising role in gastroenterology outpatient care and can be utilized to improve access to care and bridge healthcare disparities. In order to increase compliance further work needs to be done to make the digital platform user friendly for the elderly population.
Keywords
Introduction
The foundation of our healthcare system was rocked by the emergence and spread of coronavirus disease 2019 (COVID-19) virus. Health care providers struggled to find safe and practical approaches to delivering care at the outset of the pandemic [1]. Telemedicine has made it possible for patients to safely receive non-COVID-related care and reduced the spread of the COVID virus [2]. However, there is no end in sight with the continued surge due to COVID variants [3]. Implementing telemedicine proactively rather than reactively is more likely to generate greater benefits in the long-term and may also help with other everyday challenges in healthcare. Telemedicine can be especially useful when access to care is limited by location and distance. The site of this study, Mississippi, is not only considered a rural state, but also has the lowest physician to patient ratio of any state [4,5]. Patients in rural areas face access-to-care barriers as there are fewer subspecialists. The under-utilization of telemedicine is surprising, since it is established that increased access to telemedicine services can improve access and decrease costs associated with healthcare [6,7].
Surveys prior to the pandemic showed that the majority of patients in the United States were uncertain about utilizing telemedicine services, furthermore, gastroenterologists ranked second lowest among internal medicine specialties with only 8% of physicians utilizing telemedicine [8,9]. Patients were faced with issues of lack of insurance coverage, inadequate infrastructure and privacy concerns whereas providers had limitations of reimbursements, licensing, malpractice coverage, and workflow uncertainty [10]. Additionally, the poor utilization by subspecialists may be due in part to the overall lack of research in this area [11]. Research that facilitates the incorporation of telemedicine in healthcare centers, especially in the medically underserved areas, can be instrumental in addressing healthcare disparities. The COVID-19 pandemic provided an opportunity for us to observe trends in the use of different modalities in our gastroenterology clinics while identifying variables that aid or impede the success of telemedicine encounters.
Patients and Methods
Study design
This was a retrospective, single-center study at the Gastroenterology and Inflammatory Bowel Disease (IBD) focused clinic at the University of Mississippi Medical Center. The clinic converted solely to telemedicine during the early phase of the COVID-19 pandemic. Inclusion criteria for our study was all adult patients that underwent a telemedicine clinic visit from March 23, 2020 to April 30, 2020. There were no exclusion criteria. Our cohort included one hundred and fifty-three patients who scheduled a total of one hundred and fifty-eight telemedicine encounters.
Methods
Demographic data were collected using age, sex, race, zip code, and payer source. The modality of communication, audio or video, was noted along with the number of patients who switched modality at the time of the actual appointment. Each visit was mapped based on zip code and categorized into urban or rural according to rural-urban commuting area (RUCA) codes which classify U.S. census tracts using measures of population density, urbanization, and daily commuting [12]. The data was analyzed to assess the impact of these predictors on video vs audio preference and completion rates for the encounter. Chi square test was used to analyze association between categorical variables. Significance was set at a p-value of 0.05.
Ethical Considerations
The project was approved by the Institutional Review Board (IRB) at our institution.
Results
Baseline patient characteristics are provided in Table 1. There was a total of 153 patients who scheduled 158 visits during the study period, out of which 143 were successfully completed, yielding a show rate of 90.5%. Modality of appointments was determined by the selection at the time of scheduling. 79 patients (55%) completed video encounters, while 64 patients (45%) completed audio encounters. We used multiple platforms for video encounters including UMMC2YOU (our medical center’s preferred telemedicine platform), Facetime, Zoom, and Skype. 53% of the encounters were completed using UMMC2YOU, 17.5% with Facetime, 17.5% with Zoom and 12% with Skype.
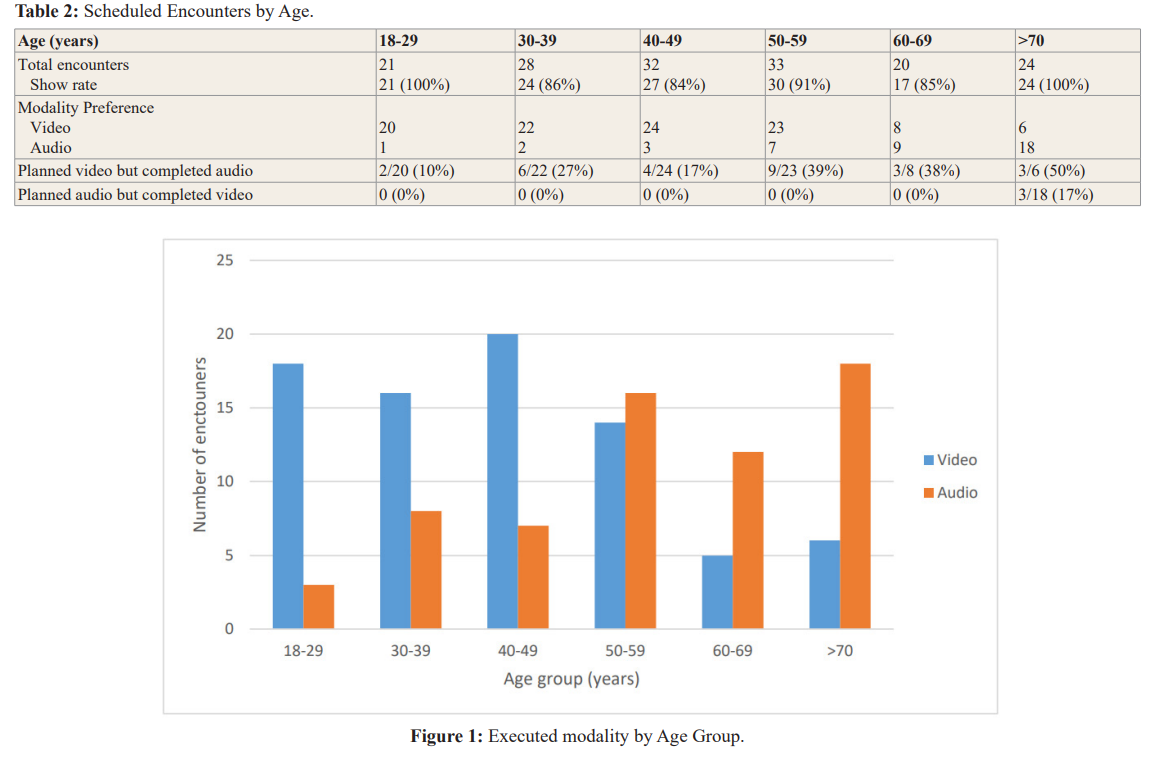
Visits were categorized by age group and modality as shown in Table 2. The mean age for the study sample was 49.7 years. The younger patients in our study had a strong preference for video appointments, 66 out of 72 patients (92%) below age 50 preferred video, while 37 out of 71 patients (52%) age 50 or older preferred video (P<0.001). The likelihood of success of a video encounter also regressed as patients' age increased as depicted in Figure 1. Overall, 26% of the patients who desired video encounters had to be switched to audio only.
There were 109 females (71%) and 44 males (29%) who scheduled a total of 153 visits. Females completed 54 video visits (49%), 46 audio visits (41%) and 13 missed their appointments (11%). 25 males completed video appointments (56%), 18 completed audio (40%), and 2 missed their appointments (4%). There were no significant differences in executed modality of encounters (video vs audio) (P=0.65), nor in show rate based on sex (P=0.17).
Our cohort consisted of 70 (49%) Blacks, 70 (49%) Whites, 2 (1.3%) non-white Hispanics, and 1 (0.7%) Asian patient. Exactly half of the black patients completed video encounters while the other half completed audio. Caucasian patients were more likely to execute video encounters with 61% completing video and 39% completing audio, however, the difference was not significant (P=0.17).
According to RUCA designations, 49 out of the 153 patients (32%) resided in rural zip codes. We found similar proportions of our rural and urban populations preferred video 71% and 62%, respectively (P=0.28). The no show rate was nearly identical with 8% of rural patients missing their telemedicine appointments compared to 10% of urban patients (P=0.62).
Payer source for each visit was also identified. Of the 143 completed visits, 87 patients had commercial insurance (including Veterans Affairs coverage), 44 had Medicare or Medicaid, and 12 were self-pay or had no insurance coverage. Of the commercial, government, and self-pay visits, video encounters were executed 60%, 52% and 58% of the time respectively. Compared to total video and audio visits, there was no statistical difference in modality between commercial, Medicare/Medicaid, or self-pay (P=0.89).
Discussion
The World Health Organization defines telemedicine as the use of information and communication technologies to provide healthcare services for the purpose of diagnosis, treatment and disease prevention [13]. From 2004 to 2017, there has been a significant increase in telemedicine usage, primarily in primary care [14]. Despite this steady growth, the global pandemic caused by the novel coronavirus has increased the use of telemedicine to an even higher degree [15]. In the field of gastroenterology, the role of telemedicine was promising prior to the COVID-19 pandemic. Cross et al showed great feasibility and patient acceptance by utilizing home telemanagement systems in a controlled trial for ulcerative colitis patients [16,17]. Similarly, Elkjaer et al. using a web based telemonitoring system, demonstrated excellent feasibility, patient acceptance and better quality of life with reduced health care cost in IBD patients [18].
Telemedicine provides an opportunity to improve patient access to subspecialty care and reduce healthcare costs. Understanding variables that may impact the success of a telemedicine visit is of utmost importance to physicians looking to integrate telemedicine in this recurring COVID-19 surges. Our study shows an overall good show rate of 90.5%, with no significant difference based on age, sex, race, or rurality, which suggests that most patients, regardless of demographic variables, have the capability to complete some modality of telemedicine encounter. This then turns the attention to understanding which variables can maximize this success. Being able to predict which patients can successfully complete which modality of telemedicine encounter will be important in efficiently integrating telemedicine into busy practices.
The majority of our population prefers video over audio visits, however, there is a linear decrease in the desire and ability to complete a video encounter as the age increases. For our cohort 26.2% of the encounters by patients who desired video had to be switched to audio only. Video adaptation from younger patients is not surprising as a 2019 survey showed that more than 90% of Millennials are likely to embrace digital technology compared to 68% of Baby Boomers [19]. The decreased level of comfort in using newer technology in older populations is likely multifactorial including cognitive ability, effort expectancy, perceived security, and facilitating conditions [20]. Some suggested solutions include asking a caregiver or family member to assist in setting up the encounter. This can be escalated to sending out “healthcare ambassadors” to the patient locations that can set up a device and ensure a seamless video appointment as well as training of the medical service providers to run simulation training to improve effectiveness of video telemedicine encounters [21,22].
While age played a significant role in determining the modality of choice, sex did not. In the pre-covid era, telemedicine has been shown to improve access to healthcare for women in rural areas and during the pandemic telemedicine visits were well received by the female population for COVID-19 diagnostic evaluation [2,23]. However, for subspecialty care we need more data to assess the role of sex in telemedicine encounters.
Our study had a relatively even split between Black and White populations. Prior studies have demonstrated racial disparity in telehealth users with low acceptance and participation by the African American population [24,25]. The source of these racial disparities in telemedicine use is a composite end point of individual, societal and structural inequalities that have built up over time. However, our particular study did not show any significant differences in show rate, or preferred modality (audio vs video) among Blacks and Whites. With a rising incidence of IBD in the nonwhite population, there needs to be a focused effort to improve health technology literacy among the nonwhite patients with attention to address access, privacy and confidentiality [26].
Payer source showed no significant difference in modality of encounter. Centers for Medicare and Medicaid Services made changes to encourage and expand the use of telehealth services [27]. There are different requirements for documentation and billing for audio and video visits therefore being able to plan ahead for each telemedicine encounter can improve efficiency and reimbursement for a busy clinic.
Notably, there was no significant association between the modality of telehealth visit and the rurality of the encounter. There are few places in the United States which have such stark differences between their major metropolitan areas and their surrounding rural counties than Mississippi. Our state has the lowest rural median household income ($40,200) and the highest rate of poverty (24.9%) in the country [28]. Despite these known geographical discrepancies, we found no indication that the location impedes the ability to successfully complete a telehealth encounter. This undoubtedly opens up more avenues for the healthcare community to investigate ways of incorporating telehealth services to patients in rural areas and thereby reducing barriers to healthcare access.
Limitations of our study included a small sample size and performed at a single academic center so findings may not be generalizable. However, our results were consistent with prior findings of increasing age as a hindrance to digital encounters. More in-depth analysis of a myriad of demographic variables is necessary to develop a more complete picture.
Conclusion
Our findings demonstrate a high acceptance rate of telemedicine modality. We found that race, sex, payor source, and residing in a rural area had no significant effect on modality (video vs audio) or show rate. We have established a good success rate of video encounters in younger populations but we need to further reduce the digital barriers for the elderly population like adopting a secure and user-friendly digital platform. The promising telemedicine visit show rate irrespective of physical location is an important finding but needs further investigation with a larger study sample to validate these results. With the recurring COVID-19 surge worldwide, we encourage healthcare centers to take steps to integrate telemedicine visits into subspecialty clinics.
References
- Liu Q, Luo D, Haase JE, et al. The experiences of health-care providers during the COVID-19 crisis in China: a qualitative Lancet Glob Health. 2020; 8: 790-798.
- Chunara R, Zhao Y, Chen J, et Telemedicine and healthcare disparities: a cohort study in a large healthcare system in New York City during COVID-19. J Am Med Inform Assoc JAMIA. 2021; 28: 33-41.
- Callaway Fast-spreading COVID variant can elude immune responses. Nature. 2021; 589: 500-501.
- Marcin JP, Shaikh U, Steinhorn Addressing health disparities in rural communities using telehealth. Pediatr Res. 2016; 79: 169-176.
- deShazo RD, Parker SB. Lessons Learned from Mississippi’s Telehealth Approach to Health Disparities. Am J Med. 2017; 130: 403-408.
- Langabeer JR, Champagne-Langabeer T, Alqusairi D, et al. Cost–benefit analysis of telehealth in pre-hospital J Telemed Telecare. 2017; 23: 747-751.
- Ashwood JS, Mehrotra A, Cowling D, et Direct-To- Consumer Telehealth May Increase Access To Care But Does Not Decrease Spending. Health Aff Proj Hope. 2017; 36: 485-491.
- Survey: Consumers remain skeptical on telehealth citing insurance coverage uncertainty [Internet]. Healthcare IT 2017. https://www.healthcareitnews.com/news/survey-consumers-remain-skeptical-telehealth-citing-insurance-coverage-uncertainty
- The Lancet Gastroenterology Hepatology null. The potential of telemedicine in digestive diseases. Lancet Gastroenterol 2019; 4:185.
- Shah ED, Amann ST, Karlitz JJ. The Time Is Now: A Guide to Sustainable Telemedicine During COVID-19 and Beyond. Am J 2020;10.
- Helsel BC, Williams JE, Lawson K, et al. Telemedicine and Mobile Health Technology Are Effective in the Management of Digestive Diseases: A Systematic Review. Dig Dis Sci. 2018; 63: 1392-1408.
- USDA ERS - Rural-Urban Commuting Area Codes ilable. https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes.aspx
- World Health Organization, Telemedicine: opportunities and developments in member states: report on the second Global survey on eHealth. Geneva, Switzerland: World Health Organization; 2010; 93.
- Barnett ML, Ray KN, Souza J, et al. Trends in Telemedicine Use in a Large Commercially Insured Population, 2005-2017. 2018; 320: 2147-2149.
- Koonin Trends in the Use of Telehealth During the Emergence of the COVID-19 Pandemic — United States, January–March 2020. 2020; 69. 1595-1599.
- Cross RK, Cheevers N, Rustgi A, et al. controlled trial of home telemanagement in patients with ulcerative colitis (UC HAT). Inflamm Bowel 2012; 18: 1018-1025.
- Cross RK, Jambaulikar G, Langenberg P, et TELEmedicine for Patients with Inflammatory Bowel Disease (TELE-IBD): Design and implementation of randomized clinical trial. Contemp Clin Trials. 2015; 42: 132-144.
- Elkjaer M, Shuhaibar M, Burisch J, et al. E-health empowers patients with ulcerative colitis: a randomised controlled trial of the web-guided “Constant-care” approach. Gut. 2010; 59: 1652-1661.
- NW 1615 St, Suite 800Washington, Inquiries D 20036USA202-419-4300 | M-857-8562 | F-419-4372 | M. Millennials stand out for their technology use, but older generations also embrace digital life [Internet]. Pew Research Center. [cited 2020 Nov 14]. Available from: https://www.pewresearch.org/fact-tank/2019/09/09/us-generations-technology-use/
- Cimperman M, BrenÄiÄ MM, Trkman P, et al. Older Adults’ Perceptions of Home Telehealth Telemed J E Health. 2013; 19: 786-790.
- Ikram U, Gallani S, Figueroa JF, et al. 4 Strategies to Make Telehealth Work for Elderly Harvard Business Review. https://hbr.org/2020/11/4-strategies-to-make-telehealth-work-for-elderly-patients
- Clay-Williams R, Baysari M, Taylor N, et Service provider perceptions of transitioning from audio to video capability in a telehealth system: a qualitative evaluation. BMC Health Serv Res. 2017; 17: 558.
- Parajuli R, Doneys P. Exploring the role of telemedicine in improving access to healthcare services by women and girls in rural Telemat Inform. 2017; 34: 1166-1176.
- George S, Hamilton A, Baker How Do Low-Income Urban African Americans and Latinos Feel about Telemedicine? A Diffusion of Innovation Analysis [Internet]. 2012; 715194, 9.
- Weber E, Miller SJ, Astha V, et Characteristics of telehealth users in NYC for COVID-related care during the coronavirus pandemic. J Am Med Inform Assoc. 2020; 27: 1949-1954.
- Aniwan S, Harmsen WS, Tremaine WJ, et Incidence of inflammatory bowel disease by race and ethnicity in a population-based inception cohort from 1970 through 2010. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6376543/
- Bajowala SS, Milosch J, Bansal Telemedicine Pays: Billing and Coding Update. Curr Allergy Asthma Rep. 2020; 20: 60.
- Bureau New Census Bureau Report Analyzes U.S. Population Projections [Internet]. The United States Census Bureau. https://www.census.gov/newsroom/press-releases/2015/cb15-tps16.html