Failure of Locoregional Anaesthesia in Dental Practice: Frequency, Causes and Replacement Strategies
Author'(s): Paul Owono Etoundi1,2*, Marie Elvire Nokam Taguemne3,4, Gouag2, Michele Kamga1, Armandine Beyene Akoa1 and Ze Minkande Jacqueline1
1Department of Surgery and Specialties/Anaesthesiology,University of Yaoundé 1, Cameroon.
2Department of Anaesthesiology, Yaoundé Central Hospital,Cameroon
3Department of Buccal Surgery and Parodontology, University of Yaoundé 1, Cameroon.
4Department of Buccal Surgery, Yaoundé Central Hospital,Cameroon.
*Correspondence:
Owono Etoundi Paul, Department of Surgery and Specialties/Anaesthesiology, University of Yaoundé 1, P.O. Box 1364 Yaoundé,Cameroon, Tel: +237 677 981 951
Received: 02 Jan 2023; Accepted: 25 Jan 2023; Published: 06 Feb 2023
Citation: Etoundi PO, Taguemne MEN, Gouag, et al. Failure of Locoregional Anaesthesia in Dental Practice: Frequency, Causes and Replacement Strategies. Anesth Pain Res. 2023; 7(1): 1-4.
Abstract
Background: Locoregional anaesthesia (LRA) is frequently practiced in odontostomatology. Our aim was to determine the frequency and causes of LRA failures and to evaluate replacement strategies in two peripheral hospitals in Cameroon.
Methodology: A prospective and descriptive study was carried out in the department of odonto-stomatology of the Ebolowa Regional Hospital and Efoulan District hospital of Cameroon from the 1st of January to the 31st of August 31st 2022. Were included, patients presenting an oral pathology requiring LRA. The variables studied were: failure rate of LRA, the reasons of failure, the strategies used after failure and their efficiency. Data analysis was performed using Epi Info 3.5.4 software. The chi-square test was used, the p-value being considered significant if < 0.05.
Results: The study sample consisted of 301 patients. The mean age was 29.9 ± 17.7 years and the sex ratio 1.3. The main pathologies were pulpopathies (47.8%). The most practiced nerve block was the truncal spina Spix anaesthesia (51.8%) with lidocaine and epinephrine. The failure rate of anaesthesia procedure was 73.4% due to the technique used. The strategies employed in case of failure were efficient in 81.4% of cases. Intra-pulpal and intra-septal anaesthesia were particularly mastered.
Conclusion: Failures of LRA in odontostomatology in peripheral hospitals are very recurrent. It’s due to the lack of qualified experienced personnel. Strategies employed in the event of failure are efficient particularly intra-pulpal and intra-septal anaesthesia.
Keywords
Introduction
Locoregional anaesthesia (LRA) is commonly used in odonto- stomatology. The choice of the technique depends essentially on the intervention, the number of teeth to be treated and their mandibular or maxillary location. The practice of LRA requires not only good knowledge in various fields such as anatomy, physiology, pharmacology, but also mastery of the technique and the time factor, which remain decisive elements of success [1- 3]. The most fearful failure by caregivers is a lack of analgesia or incomplete analgesia, which hinders the course of the intervention [3-5]. Our aim was to determine the frequency and reasons of LRA failures and to evaluate replacement strategies in two peripheral hospitals in Cameroon.
Patients et methods
Study Design, Setting and Population
It was a prospective and descriptive study, which was carried out from January 1st to August 31st, 2022, in the departments of odontostomatology of the Ebolowa Regional Hospital and the Efoulan District Hospital in Cameroon after approval by the National Ethics Committee. Our sample was made up of consenting patients who came to consult for dental care requiring LRA. After the consultation, during which the diagnosis was made, patients were taken to the practitioner where the dental care was to be done under LRA. During the dental care, LRA technique was noted. The efficacy of the LRA was assessed by the pulp sensitivity test to cold and pain was assessed using the visual analogue scale (VAS). Any pulpal sensitivity to cold and/or any painful sensation (VAS≥ 3/10) after stimulation of the anesthetised area occurring after the time of onset of the anaesthetic agents used was considered as LRA failure. Replacement strategy was then noted and evaluated according to the same criteria as the first-line LRA technique. Patients with contraindications to the drugs used were not included in the study as well as those who had a psychiatric disease and those who did not understand the VAS.
Study Variables and Data Analysis
The variables studied were sociodemographic data (age, sex), indications for dental care, the type of LRA administered (technique and anaesthetic agents), failure rate recorded, the replacement techniques used and their efficacy. Data analysis was performed using Epi info 3.5.4 statistical software. Means and standard deviations of numerical variables were reported. Categorical variables were analysed using the Fisher's exact test or the Pearson's Chi-square test. Qualitative variables were analysed using the Student t-test or the Kruskal-Wallis test. The threshold for statistical significance was set a p-value less than 0.05.
Results
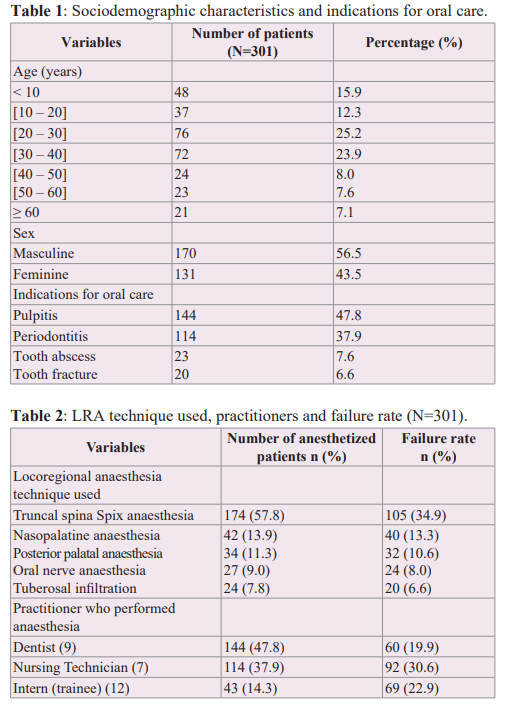
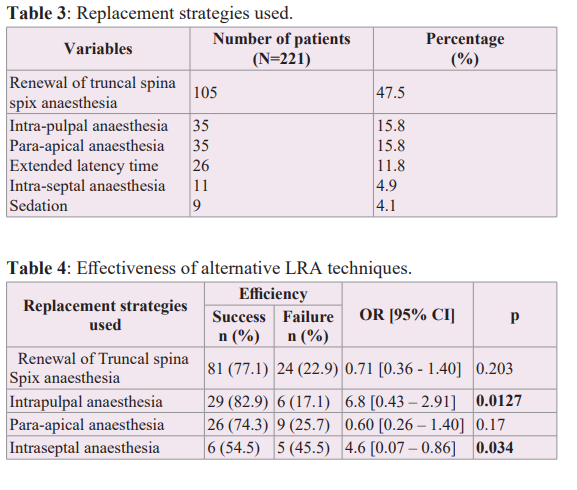
During the study period, 301 patients were included i.e., 153 at Ebolowa Regional Hospital and 148 at Efoulan District Hospital. These hospitals being of the 3rd and 4th category respectively in the healthcare pyramid of Cameroon. The mean age was 29.9 ± 17.7 years. The male gender accounted for 56.5% of cases and 43.5% were females. The indications for dental care were dominated by pulpopathies (Table 1). The most common LRA technique used was the truncal spina Spix anaesthesia (Table 2). Lidocaine 1% or 2% was the main local anaesthetic used: 283 cases and 94% respectively. In 76.1% of cases (229 patients), epinephrine (0.005mg/ml) was added. The health personnel who performed the technique were mainly dentists and odonto-stomatology nurse technicians (Table 2). The latency time was 2 to 3 minutes in 47% of the cases, then greater than 5 minutes in 38% of the LRA performed. The overall failure rate was 73.4% (221 patients) (Table 2), i.e., 84.3% at Ebolowa Regional Hospital and 62.2% at Efoulan District Hospital. Replacement techniques done by dental surgeons themselves (Table 3) resulted in a success rate of 81.4% (180 patients), therefore a failure rate of 18.6%. The techniques that proved to be significantly efficient and well mastered were intra-pulpal anaesthesia and intra-septal anaesthesia (Table 4).
Discussion
LRA in dental practice is a daily procedure for the dental surgeon. He does this in most cases alone, and rarely requests the assistance of an anaesthetist. The success of nerve blocks depends not only on the knowledge of anatomy in odontostomatology and the pharmacology of the drugs used, but also on the mastery of the different anaesthetic procedures. During the study period, 301 patients were included from the 2 hospitals. These were mostly young patients who presented mainly with pulpopathies. Bengono et al [6], Camara et al [7] had diagnosed pulpopathies in 85% and 90% respectively. Indeed, these diseases are due to poor buccal hygiene, which characterizes young people [8,9]. To treat these pulpopathies, the caregivers had opted for nasopalatine anesthesia (13.9%) and posterior palatine anesthesia (11.3%) in maxillary locations and in the mandibular location; the choice in 51.8% of cases was truncal spina Spix or inferior alveolar nerve block. In both cases, procedures frequently used this truncal anaesthesia in odontostomatology whose effect has more or less extensive dental sector. Nevertheless, the overall failure rate observed was 73.4%, i.e., 23.9% in the maxilla and 42.9% in the mandible. This failure rate was high compared to what is usually observed (15 to 20%) [10,11]. The failure rates in our sample were high compared to those of Bengono et al (6.7% in the maxilla and 35.7% in the mandible) [6]. As for Camara et al., the failure rate observed in the mandible was 39.2% [7]. The high failure rate in our series was probably related to the lack of mastery of the technique by the caregiver. Indeed, in 53.5% of cases of failure, LRA was performed by a technician or a trainee (Table 2), with a latency time exceeding 5 minutes in 38% of patients. This situation is frequently encountered in peripheral hospitals in Cameroon: dentists being few in number, they have their tasks being done by technicians and trainees. Bengono et al., and Camara et al also reported that the causes of LRA failure were technical in 60% and 73.3% respectively [6,7]. In most cases, the success of LRA in odontostomatology depends on good bases on anatomy, perfect mastery of pharmacology and procedures [12- 15]. Replacement strategies after the failure of the initial technique were local anaesthesia except the renewal of the nerve block with spina Spix anaesthesia (Tables 3 and 4). The result was a decrease in the failure rate to 18.6%. The experience of a dentist appears to be decisive in the choice of the replacement technique and its implementation. Intra-pulpal and intra-septal anaesthesia appear to be efficient techniques because they are mastered by caregivers. Bengono et al had reported the indication of these techniques in case of failure of LRA and the observation made was that it is easy to perform with a high success rate [6].
Limits
The limits of our study were the subjectivity in the assessment of the pain by patients, the multiple actors intervening in the realisation of the LRA.
Conclusion
The failures of LRA in odontostomatology in peripheral hospitals are considerable. They are due to the lack of experienced qualified personnel. Strategies employed in case of failure are efficient namely intra-pulpal and intra-septal anaesthesia.
Acknowledgement
They go to all the authors who have participated in an active, honest and regular way in the effective realization of this work. Their rigor in the analysis of the data highlighted the results presented. Also, thanks go to all patients who gave their consent for the realisation of this study
References
- Barart JA, Brand Local anaesthesia in dentistry. Springer. 2017: 198.
- Decloux D, Ouanounou A. Local anaesthesia in dentistry: a review. International dental journal. 2021; 71: 87-95.
- Nusstein JM, Reader A, Drum Local Anesthesia Strategies for the patient with a ‘Hot’’ Tooth. Dent clin North Am. 2010; 54: 237-247.
- Ogle OE, Mahjoubi G. local anesthésia: Agents, Techniques, and Complications. Dent Clin North Am. 2012; 56: 138-148.
- Sixou LJ, Marie Cousin Techniques anesthésiques chez les enfants et les adolescents. Traité EMC odontology. 2011; 23: 600.
- Bengono Bengono R, Bengondo C, Amengle AL, et al. Analgésie en Odontostomatologie: Stratégies contre les Échecs d’Anesthésie Locorégionale. Health Sci Dis. 2015; 16: 1-5.
- Camara SA, Fofana L, Bah A, et Anesthesia of mandibular molars in endodontics: study of a series of 306 cases. African journal of dentistry and implantology. 2021; 20: 54-61.
- Zero DT, Zandona AF, Vail MM, et al. Dental caries and pulpal disease. Dent Clin N Am. 2011; 55: 29-46.
- Goldberg S, Reader A, Drum M, et al. Comparison of the anesthetic efficacy of the conventional inferior alveolar Gow- Gates and Vazirani-Akinosi techniques. J Endod. 2008; 34: 1306-1311.
- Kanaa MD, Meechan JG, Corbett IP, et Speed of injection influences efficacy of inferior alveolar nerve blocks: a double blind randomized controlled trial in volonteers. J Endod. 2006; 32: 919-923.
- Kanaa MD, Whitworth JM, Meechan JG. A prospective randomized trial of different supplementary local anesthetic techniques after failure of inferior alveolar nerve block in patients with irreversible pulpitis in madibular J Endod. 2012; 38: 421-425.
- Mejare I, Axelson S, Dahlen G, et al. Caries risk assessment. A systematic review. Acta Odontol Scand. 2014; 72: 81-91.
- Sztark F. Toxicité des anesthésiques locaux. Revue d'Anesthésie-Réanimation et de Médecine d'Urgence. 2009; 11: 1-7.
- Beloeil H, Mazoit Pharmacologie des anesthésiques locaux. EMC Anesthésie Réanimation. 2010; 36: 320-336.
- Giovannitti JA, Rosenberg MB, Phero JC. Pharmacology of local anesthetics in oral surgery. Oral Maxillofac Surg Clin. 2013; 25: 453-465.