Foot Blocad in Foot Day Surgery
Author'(s): Helin Duygun1 , Ibrahim Turan2 and Jan G Jakobsson3*
1Pharmacolog Istanbul Florence Nightingale Hospital, Istanbul Turkey.
2Professor, Department of Orthopaedi Foot &Ankle Surgery section,Istanbul Florence Nightingale Hospital Istanbul Turkey.
3Professor Anaesthesia & Intensive Care, Institution for Clinical Sciences, Karolinska Institutet at Danderyds University Hospital,Stockholm, Sweden.
*Correspondence:
Jan G Jakobsson, Professor Anaesthesia & Intensive Care,Institution for Clinical Sciences, Karolinska Institutet at Danderyds University Hospital, Stockholm, Sweden.
Received: 03 September 2019; Accepted: 24 September 2019
Citation: Helin Duygun, Ibrahim Turan, Jan G Jakobsson. Foot Blocad in Foot Day Surgery. Anesth Pain Res. 2019; 3(2): 1-3.
Keywords
Office based surgery, coming and leaving hospital day of surgery, is associated to several benefits. The risk for nosocomial infections, thromboembolic complications is reduced. Early ambulation and alimentation possibly improve healing. There are obvious benefits reducing hospital stay, reducing cost. The use of loco-regional anaesthesia facilitates the office-based logistics reducing recovery from anaesthesia. Loco-regional anaesthesia with a long acting local anaesthetic combined with an adjunct to further extend the duration have major benefits reducing postoperative pain. It should be used in combination with oral analgesics taken in advance to the weaning of the block to avoid rebound pain.
A majority of minor and intermediate foot surgical procedures can be performed in loco-regional anaesthesia in the office theatre [1,2]. We will give a short presentation of our experience from loco-regional anaesthesia managed office-based foot surgery [3,4].
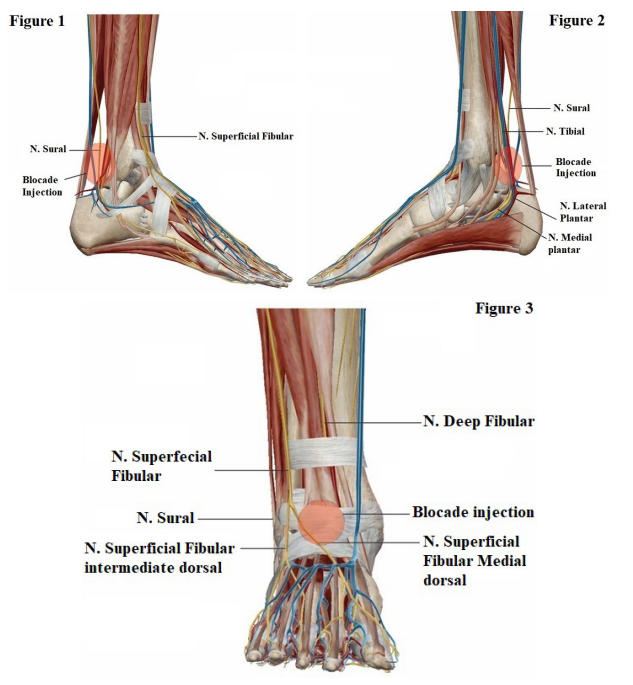
The Ankle Block
Ankle block is a safe technique that is easily learnt and render a high success rate [5]. The basics for performance of the ankle block are; with the use of Lidocaine 10 mg/ml.
- The posterior tibia nerve by injecting 5 cc posterior to the medial malleoli, (Figure 1).
- The peroneal nerve, superficial and deep by injecting 6-8 cc on the dorsum of the foot (Figure 2).
- The Sural nerve by injecting 4 cc posterior to the lateral malleoli (Figure 3).
Local anaesthetics
The choice of local anaesthetic drug is importance.
All the fast acting local anaesthetics lignocaine, mepivacaine or prilocaine can be used for infiltration or provision of the ankle block. A solution with 10 mg/ml is sufficient to provide adequate intra-operative anaesthesia. These 3 amide local anaesthetics provide rapid onset within 3 to 10 minutes.
Lignocaine, mepivacaine and prilocaine have a moderate duration of action (1-2hr). Bupivacaine, levo-bupivacaine, or ropivacaine have a somewhat shower onset but give long lasting local anaesthesia. Pain relief is commonly achieved for up to 6-8 hours. For each individual agent the duration of anaesthesia will be determined by the total dose of the drug given rather than the volume or concentration of drug used.
Fast acting/short duration
lignocaine, mepivacaine, prilocaine
Long acting
Bupivacaine, levo-bupivacaine, ropivacaine
The effect of vasoconstrictors may be preferred to both reduce per operative bleeding and prolong the duration of anaesthesia. The effect on duration, however depends on the local anaesthetic used and the site of the injection. The addition of adrenaline reduces the peak concentration in the blood and thus the risk for systematic toxicity, but the degree of this reduction depends on the site of injection and the specific local anaesthetic agent.
General dose recommendations are given in the table.

Toxicity of local anaesthesia
Local anaesthetic agents are relatively free from side effect when administered in appropriate doses and in the correct anatomical location. However, systemic and localised toxic reactions may occur, usually from accidental intra vascular administration or excessive doses. Systemic reactions to local anaesthetics are primarily associated with central nervous system (CNS) and the cardiovascular system
Postoperative pain management
In day /Office based surgery preoperative information and patient`s understanding of the surgical procedure and the postoperative course is of greatest importance. A motivated and well-informed patient who is aware of the pain pattern, rehabilitation schema and pain medication strategy are much better off than the inadequately informed patient. Patients’ expectations have an important impact on overall satisfaction [6].
Procedure specific pain meditation schemes should be available based on multi modal pain management; local anaesthesia, paracetamol, NSAIDs/Coxibs in adequate doses and dosing scheme [7]. Weak opioids and when needed strong opioids should be considered as rescue analgesics but must be provided/prescribed in amounts that secure that chronic use and addiction is avoided. A procedure specific evidence-based pain management ladder should be the bases for all Day Surgical procedure [8].
An example for ASA I-II patient with no know allergies:
- The basic medication consists of Paracetamol 1 gm up to four times daily.
- The preferred rout of administration is oral.
- The intravenous formulation is an option during the intra operative period if needed.
- The next lever is an NSAID/Coxib providing profound analgesia
- The oral route is effective and should be preferred way of administration.
- The risk for gastro-intestinal side effect when used for longer periods of time should kept in mind [9].
Both Coxibs and traditional NSAID´s should be avoided in patients with instable cardiovascular disease and it may impair healing [10]. When used short term at the lowest effective dose, however, NSAIDs/ Coxibs provide analgesia without significant toxicity [11].
Although nonspecific NSAID`s provide similar analgesia to Coxibs, their use has been limiter in the Perioperative setting because of their side effect on platelet function increasing the risk for bleeding and haematoma. Coxibs may be a safer alternative in that setting, they do not cause less coagulation impairment and almost no increased risk for bleeding /blood loss which has been documented also major orthopaedic cases [12].
Good analgesia effect in combination with minimum side effect such tiredness, nausea, and vomiting is of outmost importance in day surgery. Postoperative pain management should start before or immediately after the end of surgery with an oral dose.
Summary and Conclusion
Information and active coaching of the patient through the entire peri-operative period is of great importance for success. Patient satisfaction is important, and efforts should be focus on obtaining adequate pain relief with minimum side effect. A multi-modal pain management strategy has become Gold Standard; based on a long acting local anaesthetic in the wound or as a block, oral pain medication base paracetamol, NSAID or Coxib for 3-4 days and further availability of an oral opioid as rescue pain medication when needed. The opioids should be provided in minimal amount to avoid any risk for chronic use and addiction.
References
1.Blomgren M, Turan I, Agadir M. Gait analysis in hallux valgus. J Foot Surg. 1991; 30: 70-71.
2.Turan I, Lindgren U, Lundberg I. Surgical treatment of forefoot deformity with special reference to polyarthritis. Clin Orthop Relat Res. 1991; 148-151.
3.Turan I, Hein A, Jacobson E, et al. Sevoflurane requirement during elective ankle day surgery: the effects of etirocoxib premedication, a prospective randomised study. J Orthop Surg Res. 2008; 3: 40.
4.Turan I, Assareh H, Rolf C, et al. Multi-modal-analgesia for pain management after Hallux Valgus surgery: a prospective randomised study on the effect of ankle block. J Orthop Surg Res. 2007; 2: 26.
5.Kocheta A, Agrawal Y. Landmark Technique for a Wrist Block. JBJS Essent Surg Tech. 2018; 8: e7.
6.Jakobsson JG. Recovery and discharge criteria after ambulatory anesthesia: can we improve them? Curr Opin Anaesthesiol. 2019.
7.Jakobsson JG. Pain management in ambulatory surgery-a review. Pharmaceuticals (Basel). 2014; 7: 850-865.
8.Gupta A, Jakobsson J. Acetaminophen, nonsteroidal anti- inflammatory drugs, and cyclooxygenase-2 selective inhibitors: an update. Plast Reconstr Surg. 2014; 134: 24-31.
9.Warren-Stomberg M, Brattwall M, Jakobsson JG. Non- opioid analgesics for pain management following ambulatory surgery: a review. Minerva Anestesiol. 2013; 79: 1077-1087.
10.Cooper C, Chapurlat R, Al-Daghri N, et al. Safety of Oral Non-Selective Non-Steroidal Anti-Inflammatory Drugs in Osteoarthritis: What Does the Literature Say? Drugs Aging. 2019; 36: 15-24.
11.Brattwall M, Turan I, Jakobsson J. Pain management after elective hallux valgus surgery: a prospective randomized double-blind study comparing etoricoxib and tramadol. Anesth Analg. 2010; 111: 544-549.
12.Wickerts L, Warrén Stomberg M, Brattwall M, et al. Coxibs: is there a benefit when compared to traditional non-selective NSAIDs in postoperative pain management?. Minerva Anestesiol. 2011; 77: 1084-1098.