Haemodynamic Responses and Effectiveness of Head Upright Tilt Test in Unexplained Syncope in Children
Author(s): Saji Philip1* and Ajit Thachil2
1Division of Pediatric Cardiology, Tiruvalla Medical Mission Hospital, Kerala.
2Division of Electrophysiology, Lisie Heart Institute. Kochi, Kerala, India.
*Correspondence:
Dr. Saji Philip, Division of Pediatric Cardiology, Tiruvalla Medical Mission Hospital, Kerala, India.
Received: 07 Sep 2023; Accepted: 21 Oct 2023; Published: 27 Oct 2023
Citation: Saji Philip, Ajit Thachil. Haemodynamic Responses and Effectiveness of Head Upright Tilt Test in Unexplained Syncope in Children. Cardiol Vasc Res. 2023; 7(5): 1-5.
Abstract
Background: Vasovagal syncope is a benign condition, defined as a transient loss of consciousness and postural tone due to cerebral hypoperfusion. The Head Upright Tilt Test (HUTT) is widely used and has proven to be a practical tool for the diagnosis and treatment of syncope. In this study, we evaluated various hemodynamic responses obtained from the Head Upright Tilt Test and usefulness of HUTT in training for possible prevention of syncope in pediatric population.
Methods: A total of 75 consecutive subjects aged 5 to 20-years affected by syncope or near syncope underwent head upright tilt testing over a 5-year period, from the single centre data base study between 2015 and 2019. Test results were classified as negative or positive. Positive cases were further classified into vaso-depressive, vasoinhibitory, and mixed hemodynamic reactions and were also followed up prospectively over a 3-year period.
Results: Of the 75 cases studied 50.7% male and 49.3% female. Positives were 69.3% (n=52), and the remaining cases were negative for vaso-vagal syncope. Among HUTT-positive cases, the most common hemodynamic responses in the pediatric population were of the mixed type (52%), followed by the vasodepressive type (40%), vasoinhibitory (6%), and psychogenic causes (2%). HUTT-positive cases were followed up for 3-years, and the majority of patients (77%) had no significant symptoms during the follow-up in our syncope evaluation clinic.
Conclusion: HUTT is an important investigation to differentiate unexplained syncope from other causes of unconsciousness in the pediatric population. The most common hemodynamic reactions obtained in tilt test were of the mixed type, followed by the vasodepressive type. The HUTT test may also be considered as training for possible prevention of further episodes of syncope in children.
Keywords
Introduction
Vasovagal syncope can be defined as a transient loss of conscious- ness and postural tone secondary to cerebral hypoperfusion [1].
Orthostatic tolerance refers to the ability to maintain cardiovascular stability in an upright position against the hydrostatic effects of gravity, thereby maintaining cerebral perfusion and preventing syncope ("simple faint") [2]. In the late 1980s, the head-upright-tilt test (HUTT) was first used to diagnose syncope [3]. An incidence peak occurs at age 15 years, with females more than twice as likely to be affected as males [1,3].
Published results from a survey of college students with an average age of 20 years showed that approximately 20% of males and 50% of females reported experiencing at least one syncopal episode [4]. During the first two decades of life approximately 15% of children experience at least one episode of transient loss of consciousness otherwise known as vasovagal syncope or neural mediated syncope [5]. Several techniques are available to assess orthostatic tolerance and the effects of gravity on the circulation, usually by reproducing a presyncope event, also known as a near fainting episode, in a controlled laboratory setting [2]. In addition to other basic tests that are recommended, the simple HUTT has been used to assess neurally mediated syncope and has been found to be an ideal practical tool in the diagnosis and treatment of syncope [6].
Tilt training, a novel treatment for recurrent vasovagal syncope based on exercise sessions involving prolonged upright posture (or dorsi flexion and extension of your feet while standing), has been shown to be effective in preventing recurrence of vasovagal syncope. The aim of this study was to demonstrate the efficacy of the tilt test in relation to recurrent syncope and the long-term beneficial effects of the tilt test as a training program to prevent further episodes [7]. A combination of peripheral arterial and venous vasodilation, closely followed by relative bradycardia, is the most common physiological scenario observed in spontaneous or induced syncope in young people [7].
Materials and Methods Study population
A total of 75 consecutive children from the data base of a single centre, affected by syncope or near syncope who underwent a Head Upright Tilt Test (HUTT) between 2015 and 2019 were included in this study. In our study population, the HUTT was performed in 5-20 years (n=75) of age group considered as pediatric age group to assess unexplained syncope. In all cases, preliminary examinations such as ECG and echocardiogram were performed before the HUTT. Baseline heart rate, blood pressure, and other symptoms and signs of presyncope and/or fainting were recorded. Performing other preliminary examinations such as Holter test and electroencephalogram before the tilt test was preferred only after reviewing the history and the predominant symptoms reported by the patient or the patient's parents. The common manifestations of HUTT-positive cases were also evaluated.
Diagnostic Head-Upright Tilt Test
Consent was obtained before the tipping experiment, and we had allowed a spectator to watch the experiment being performed, mostly parents. This served to alleviate the anxiety of the children and parents and also to avoid legal issues during the tipping study. A physician and nurse will of course accompany the HUTT. In all cases, an intravenous cannula was placed for emergencies and for the pharmacological provocation test. The resting phase in a recumbent position lasted at least 15 minutes, and then patients were tilted to a standard angle of 70 degrees for at least 30 to 45 minutes. During the procedure, time recording was started, and heart rate, blood pressure, electrocardiogram, respiratory rate, and oxygen saturation were continuously monitored.
If symptoms and signs of presyncope or syncope occurred, such as palpitations, chest discomfort, dizziness, fainting, nausea, sweating, or loss of consciousness, the tilt test was considered positive and the patient was immediately placed in the supine position. If no symptoms occurred during the thirty minutes of passive tilt, the patient was allowed to stand for an additional 15 minutes. The variability in heart rate or blood pressure fall without significant signs and symptoms manifested while doing tilt test may considered as false positive, and further advised other investigations.
Infusion challenge
If no further reactions occurred even after tilting, the patient received an infusion of isoprenaline at our centre IV (5 µg /kg body weight/mt), which was administered in increasing doses (0.02 to 0.08 µg/kg/mt) until the heart rate increased by 30% above the recorded baseline heart rate. Sublingual administration of isosorbide dinitrate or clomipramine was not included in our study protocol, mainly to avoid side effects because the study population were children. The nature of the responses was observed by monitoring blood pressure and heart rate. Sutton's terminology was adopted for classification of neurocardiogenic syncope [8]. Test results were classified as negative or positive. Positive results were further divided into vasodepressive, cardioinhibitory, and mixed. A reduction in arterial blood pressure without a reduction in heart rate was defined as vasodepressive response, and a reduction of heart rate causing 3 seconds or more of asystole was defined as cardioinhibitory response. When a reduction in arterial blood pressure and heart rate, but without a 3 second pause was defined as mixed response.
This protocol for the head-up tilt test was consistent with the class I recommendations of the “European Society of Cardiology Task Force” Report on Syncope [1]. Subjects were followed up prospectively and retrospectively for 3 years. Follow-up was done in person when they visited the hospital and by telephone in those who suffered no further episodes. Categorical variables were presented as frequency and percentage and age, systolic and diastolic blood pressure at baseline and after isoprenaline injection as descriptive statistics. Age was then categorised into the appropriate groups. Median systolic and diastolic blood pressures at baseline and after isoprenaline injection were compared using the Wilcoxon signed rank test. The association between demographic variables (age and sex) and hemodynamic responses was tested for statistical significance using chi-square/Fisher’s exact tests. A p value of less than 0.05 was considered the threshold for statistical significance.
Results
Of the 75 cases examined with the HUTT, 10 cases (13.3%) were in the 5-9 years age group, 31 cases (41.3%) were in the 10-14 years age group, and 34 cases (45.4%) were in the 15-20 years age group. They were 50.7% (n=38) male and 49.3% were females (n=37) and sex incidence were more or less equal (Figures 1 and 2). Positive were 69.3% (n=52) and the remaining were negative. Among HUTT-positive patients, the most common hemodynamic responses in the pediatric population were mixed (n=27, 52%), followed by vasodepressive (n=21, 40%), cardioinhibitory (n=3, 6%), and psychogenic (n=1, 2%) (Figure 3). The most common manifestations of HUTT-positive cases in the paediatric age group occurred after isoprenaline infusion, in the order: near syncope (dryness of tongue, cold and clammy, and pale lips) (85.1%), chest discomfort and palpitation (60.5%), dizziness (54.3%), chest tightness or fatigue (41.9%) and nausea & vomiting (15.6%). Chest discomfort and palpitation alone not considered as positive unless otherwise associated hemodynamic changes seen. Four cases had symptoms on tilt alone without giving medication. All patients who underwent a HUTT were well managed and appropriately counselled during the period of presyncopal episodes on the table, and direct current shock was not required in any of our cases. In all positive cases, good hydration was advised, especially before going to school, office, or other work, and 61 (65.8%) of them had no significant symptoms that would have required a visit to the outpatient clinic. They were well cared for on their own, and knowledge of the warnings they had received from the HUTT prompted them to adapt to a semi reclining or supine posture to prevent overt syncopal episodes. HUTT-negative patients were further evaluated in various specialties to rule out other causes of loss of consciousness.
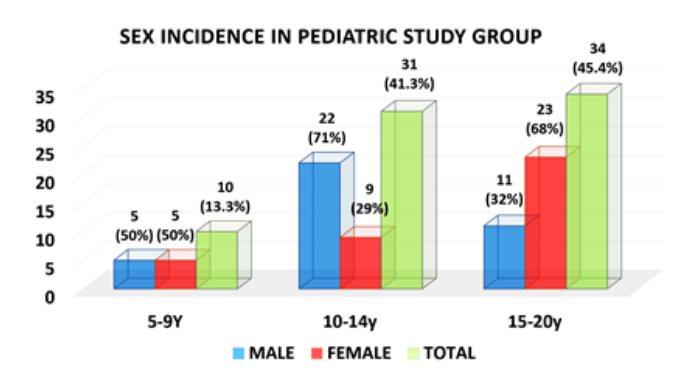
Figure 1: Pediatric study population showing male and female incidence in different age groups with number and percentage in parentheses.
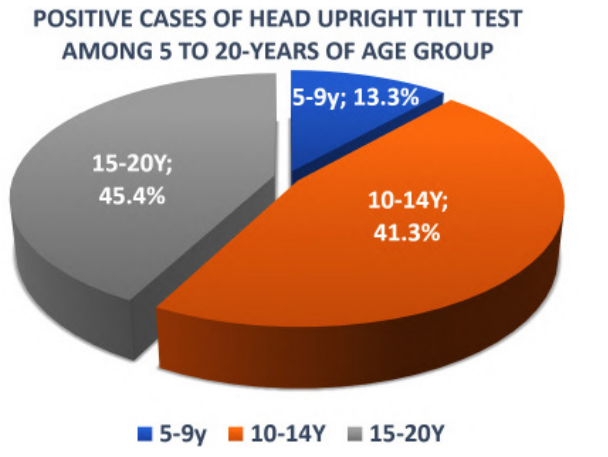
Figure 2: Positive cases in HUT Test in pediatric age groups.
During the 3-year follow-up period, only 23% (n=12) patients reported to the hospital with syncope or loss of consciousness, and 77% (n=40) were asymptomatic or had minor symptoms with near syncope that they managed themselves by adopting a semi-reclining or recumbent posture to avoid overt syncopal episodes based on the warnings they received from the HUTT. Most of the cases responded to short-term beta-blockers in cases with history of palpitation or other appropriate medications such as mineralocorticoid -fludrocortisone or midodrine or both. One of the three-cardioinhibitory cases was referred for permanent pacemaker implantation and two were kept under observation.
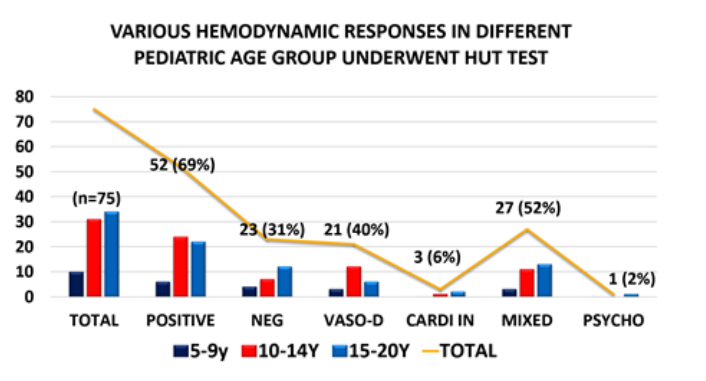
Figure 3: Combo Bar chart figure showed various hemodynamic responses observed in different age group of pediatric population with history of syncope or near syncope (n=75) underwent HUT test. HUTT; Head upright tilt test, VASO-D; Vaso-depressive, CARDI-IN; Cardio inhibitory.
Discussion
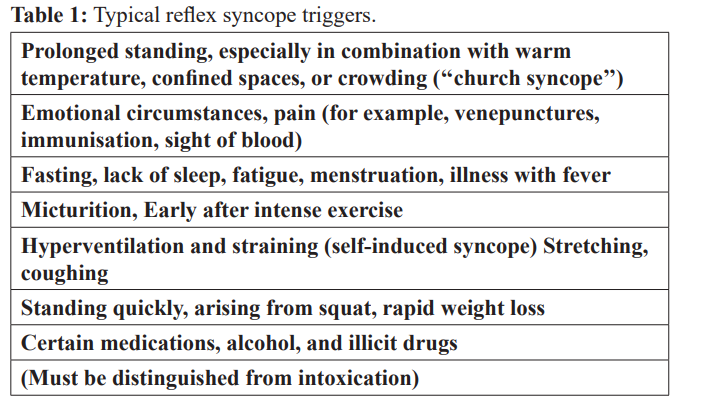
The tilt table test is a diagnostic procedure for patients with syn- cope of unknown cause. The typical triggers leading to vasovagal syncope or neural mediated syncope are given in Table 1.
A combination of peripheral arterial and venous vasodilation, followed closely by relative bradycardia, is the most common physiological scenario observed in spontaneous or induced syncope in the young [9]. A variety of terms have been used to describe such events, including simple fainting, vasovagal, vasodepressive, and neurocardiogenic syncope or neurally mediated syncope. Two clinical scenarios in particular are known to trigger vasovagal fainting. Foremost are situations that increase venous blood pooling below the heart, such as prolonged motionless standing, especially in combination with elevated ambient temperatures. In young people, prodromal signs and symptoms often occur when spontaneous vasovagal syncope is imminent. Typical premonitory symptoms observed in reflex syncope are light-headedness, dizziness, palpitations, weakness, dimming or blurred vision, nausea, epigastric distress, feeling warm or cold facial pallor, sweating and dilated pupils.
These prodromes are reported to be more intense than in older people and may be related to more robust autonomic control. However, some young people have no or few prodromal symptoms, and collapse occurs without warning. The second scenario is syncope at the time of a stressful emotional situation or pain, which is also more common in young people. A typical example is an event during a blood draw. Other emotional triggers reported in young people include hair cutting or brushing, eye examinations or manipulations, dental procedures, or watching television shows about medical topics or animal biology [10].
A conversion reaction is a rare cause of what appears to be a temporary loss of consciousness in young people. However, it can occur in adolescents, and more commonly in females. The diagnosis should be considered when the number of syncopal events is high (up to several times daily) and there is no physical injury [10]. The duration of loss of consciousness is often long (10-30 minutes) despite supine position, a finding that is not consistent with hypotension/hypoperfusion-induced syncope. During a pseudo-syncope, the eyes may be tightly closed, fluttering of eyelids and sometimes with fast and deep respirations can be seen. Unusual body posture may be assumed. Passive lifting and dropping of an extremity rarely show flaccidity or lack of consideration of pain [11]. Most importantly, blood pressure is always normal or elevated during monitoring. If cerebral blood flow is monitored and is also normal, physiologic syncope is excluded. Typically, patients use the events to consciously or unconsciously avoid an unpleasant emotional situation. Simulated convulsions (pseudo cramps) have also been reported in young people as a cause of transient loss of consciousness. Finally, abuse of illicit substances, especially alcohol and cocaine, may be associated with unexplained syncope. In our cases, one case was psychogenic and was successfully treated with appropriate counseling. Postural orthostatic tachycardia syndrome (POTS) has received much attention recently. It is defined by symptoms of cerebral and retinal hypoperfusion (i.e., light headedness, fatigue, weakness, blurred vision) and an excessive increase in heart rate in the upright posture with arterial blood pressure values in the lower limit of normal [11,12]. Decreased cerebral blood perfusion has been documented with transcranial Doppler techniques. We did not observe POTS in our limited number of HUTT cases.
When questioned, many syncope patients turn out to be salt and/ or fluid avoiders. In addition, a number of patients and/or their parents report a very low frequency of urination and the occurrence of concentrated urine. Each of these findings can be addressed. A low-salt diet should be avoided. Hydration status can be improved by "superhydration" achieved by adequate fluid intake so that colourless urine is produced twice in the morning and twice in the afternoon. Beverages containing electrolytes and/or sugar are most helpful. Hydration is especially important on the hottest days, before and during exercise, or when symptoms are frequent. In addition, passive leg exercises such as cross over legs, sideways or up & down movements of the feet while prolonged standing may be used as a preventive measure under stressful conditions before presyncopal symptoms occur. In highly motivated patients with recurrent symptoms, progressively prolonged upright posture or "tilt training" may reduce the occurrence of recurrences [13]. The exact mechanism underlying its efficacy is unknown but is likely related to a reduction in vascular compliance in the compartments most responsible for venous congestion. Patient compliance may limit its use in the young. Psychological counseling is the first choice of treatment in syncope with blood phobia. In one or more sessions, patients are exposed to phobic stimuli and should learn counter manoeuvres. The prognosis after psychological counselling seems to be very good.
Beta-blockers are most commonly prescribed in adults, but are no more effective than placebo in most studies and often have tolerable side effects. The mineralocorticoid fludrocortisone is most commonly used in young people to increase blood volume. It may be most effective in combination with high salt and fluid intake. Mild fluid retention and occasional hypertension are generally the only significant side effects, so fludrocortisone is best tolerated in paediatric patients. Most children responded well to counselling, the recommendation to drink plenty of fluids, passive or active exercise movements of leg and feet while prolonged standing, especially in the school assembly to prevent both presyncope and syncopal episodes in children [14]. In persistent low BP cases, both mineralocorticoid and alpha-adrenergic agonist, midodrine will be effective in such situation. Whereas children with mitral valve prolapse presented with palpitation and syncope, majority were well responded to beta blockers and some were to mineralocorticoid. All pharmacotherapy were given in children only for a short-term period, maximum two to three months, and then they were instructed to take medication at the time of board examination period or attending interviews or drawing the situations where anxiety and palpitation occur.
Conclusion
The head upright tilt test may be an important investigation for the diagnosis of unexplained syncope to distinguish other causes of loss of consciousness in children. Determining the types of hemodynamic responses is also important for appropriate treatment of syncope. Among HUTT-positive patients, the most common hemodynamic reactions were of the mixed type, followed by the vasodepressive type. Most children were responded to the recommendation of plenty of fluid intake and passive exercise of legs while prolonged standing, and with or without short- term appropriate medications. In the positive group, HUTT may also be considered as training test to prevent further episodes of unexplained syncope in certain extend.
Acknowledgement
Ms Nisha Kurian, Assistant Professor, Department of community Medicine, Pushpagiri Medical College, Thiruvalla for the statistical analysis. Cardiology department, St. Gregorios Cardio Vascular Centre, Parumala for syncope case registry.
Limitations
Since our study is a single center study, a multicentre research with more number of cases may be needed to validate the usefulness of HUTT as a training to prevent further episodes of syncope.
Financial support and sponsorship: Nil.
Conflicts of interest: There are no conflicts of interest.
References
- Task force for the diagnosis and management of syncope, Practice guidelines (version 2009). Eur Heart J 2009; 30:2631-
- doi: 10.1093/eurheartj/ehp298. Epub 2009 Aug 27.
- Clare L. Protheroe, Henrike (Rianne) J.C. Ravensbergen, Jessica A. Inskip, et al. Tilt Testing with Combined Lower Body Negative Pressure: a "Gold Standard" for Measuring Orthostatic Tolerance. J Vis Exp. 2013; 73: e4315.
- Ganzeboom KS, Colman N, Reitsma JB, et Prevalence and triggers for syncope in medical students. Am J Cardiol. 2003; 91: 1006-1008.
- Ozan Kinay, Mehmet Yazici, Cem Nazli, et al. Tilt training for recurrent neurocardiogenic syncope: effectiveness, patient compliance, and scheduling the frequency of training Sessions. Jpn Heart J. 2004; 45: 833-843.
- Scott WA. Evaluating the child with syncope. Pediatr Ann.1991; 20:350-359.
- Alboni P, Bringnole M, Menozzi C, et Syncope in children and adolescents. J Am Coll Cardiol. 1997; 29: 1039-1045.
- Saul Syncope: etiology, management, and when to refer. J South Carolina Med Assoc. 1999; 95: 385-387.
- Sutton R, Petersen ME. The clinical spectrum of neurocardiogenic syncope. J Cardiovasc Electrophysiol. 1995; 6: 569-576.
- Stephenson JBP, McLeod KA. Reflex anoxic seizures. In: David TJ, ed. Recent advances in pediatrics 18. Edinburgh: Churchill Livingstone. 2000.
- Van Dijk JG. Conditions which mimic syncope. In: Benditt DG, Blanc JJ,Brignole M, Sutton R, The evaluation and treatment of syncope: a handbook for clinical practice. Blackwell / Futura. 2003.
- Low PA, Sandroni P, Singer W, et al. Postural tachycardia syndrome - an Clin Autonom Res. 2002; 12: 107-109.
- Dijk N, Velzeboer SCJM, Destree-Vonk A, et Psychological treatment of malignant vasovagal syncope due to bloodphobia. PACE. 2001; 24: 122-124.
- Azizi Malamiri R, Momen AA, Nikkhah A, et Usability of the head upright tilt test for differentiating between syncopal and seizure-like events in children. Acta Neurol Belg. 2015; 115: 575-579.
- Yozgat Y, Karadeniz C, Ozdemir R, et al. Different haemodynamic patterns in head-up tilt test on 400 paediatric cases with unexplained syncope. Cardiol Young. 2015; 25: 911-917.