Health Related Quality of Life Following Coronary Revascularization: A Prospective Cross-sectional Study
Author'(s): Mohamed Salah, Hussein Wamdha and Musa Yagoub*
*Correspondence:
Dr. Yagoub Musa, Consultant Cardiologist and Head of the Heart Failure Unit at Alshab Hospital, Khartoum, Sudan, Tel: +249912338899; E-mail: yagoobelshaikh@yahoo.com
Received: 19 October 2018; Accepted: 15 November 2018
Citation: Mohamed Salah, Hussein Wamdha, Musa Yagoub. Health Related Quality of Life Following Coronary Revascularization: A Prospective Cross-sectional Study. Cardiol Vasc Res. 2018; 2(4): 1-5.
Keywords
Introduction
Coronary Artery Bypass Grafting (CABG) and percutaneous coronary intervention (PCI) are invasive options for managing patients with coronary artery disease (CAD). CABG was first introduced in 1964 and it has been firmly recognized since then as a key surgical intervention for patients with intractable angina pectoris despite medications and myocardial infarction [1,2]. Percutaneous transluminal coronary angioplasty (PTCA) or percutaneous coronary intervention (PCI) established in 1979 by Andreas Gruentzig in Switzerland to treat stenotic coronary lesions of coronary arteries, the procedure then progressed technically and introduced devices like stents which improve not only long-term patency of treated lesions but also the prognosis of patients [3,4]. With the use of both revascularization methods (CABG and PCI), the relief of symptom and survival rates have increased [5]. The relative efficacy, benefits and risks of the two procedures have been compared in several studies [6-12]. In the latest published European and American guidelines, both CABG and PCI are accepted revascularization methods to reduce mortality and improve morbidity [13,14].
Health is not only a biomedical but also a biopsychosocial issue according to the World Health Organization’s definition of health [15]. Among patients with cardiovascular disease, in addition to survival and symptom relief, health related quality of life (HRQoL) is of para-amount [16]. Although no consensus definition exists, HRQoL includes physical, psychological and social well-being [17,18].
Several studies [19-23] have investigated the effect of CABG and PCI on HRQoL. Generally, both interventions improved HRQoL, however, many points drown from these studies. Firstly, compared to CABG, PCI favorably affects HRQoL in the period immediately following the procedure, on the other hand, CABG is better than PCI on the long term but the benefits of both diminished over time. secondly, concerns remained about repeat procedure after PCI and neuro-cognitive decline following CABG. Thirdly, age is not a barrier to the improvement in HRQoL offered by revascularization, while women had less benefit compared to men and finally, comorbidities affect the overall benefits of both procedures [19-23].
Consequently, it is important to assess and compare HRQoL outcomes after PCI and CABG surgery, because any significant differences may influence physician’s and /or patient’s choice of the revascularization procedure.
Materials and Methods
This prospective, cross-sectional, descriptive, hospital- based study is sought to assess health related quality of life in patients with CAD who had undergone CABG or PCI at Alshaab Teaching Hospital (Khartoum, Sudan) in the period from April – July 2017.
Patients Twenty years and more who have been diagnosed with CAD and subsequently undergone revascularization procedures, either CABG or PCI during the study period were included, while Patients undergoing simultaneously another surgical cardiac procedure in addition to CABG, like CABG plus valve replacement/repair, Patients with history of previous CABG or PCI, Patient undergoing CABG or PCI because of heart failure., Patient with rheumatic heart disease., Patient with other significant residual valvular diseases and those who refused to participate in the study have been excluded.
Convenient sampling was used and a total coverage of study population was done i.e. all patients that happened to be available at the time of data collection period were covered and included.
Interviewing questionnaire was used to collect data on study variables which include demographic variables, physical, emotional and social components of CAD HRQoL. The questionnaire was developed and adapted based on Medical Outcomes Study Short Form (SF-36) and Seattle Angina Questionnaire (SAQ).
Statistical Analysis
Data were entered into the Statistical Package for the Social Sciences (IBM SPSS Statistics for windows version 21.0, IBM Corp Armonk, NY, USA).
Descriptive statistics were conducted for all variables (e.g., frequencies, percentages, minimum, and maximum), data were presented as mean ± standard deviation for continuous variables, and proportions for categorical data. Parametric or nonparametric tests were used for continuous variables. Chi squared test was used to compare means for categorical variables.
P value of less than 0.05 was considered statistically significant. Data were presented in form of frequency distribution tables, cross tabulation tables, figures and narrative illustration.
Ethical Consideration
Ethical clearance was obtained from the ethical review committee at Alshaab teaching hospital. A written consent was obtained from each participant after explaining the study. Confidentiality of data as well as anonymity of individual identity was adhered to as far as possible.
Results
A total of 100 subjects were included, 70% of them are male. 59% of these 100 subjects are at the age group 40 to 65 years, 31% at age more than 65 years and only 10% are at age of less than 40 years. Out of 100, 80 subjects (80%) undergone PCI while 20% undergone CABG (Figure 1).
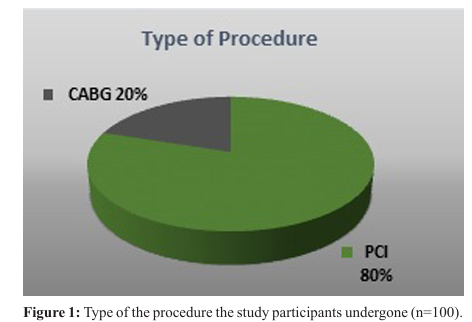
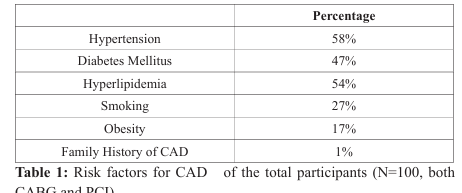
Table 1 shows the medical background and risk factors for CAD in these 100 subjects.
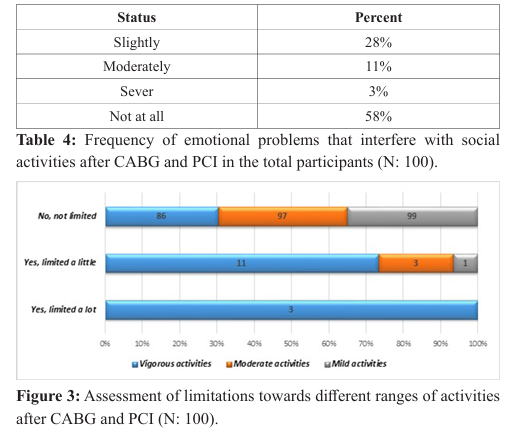
In assessing the physical component of HRQoL, as shown in figure 2, 8% of the total patients experienced chest pain after revascularization with CABG or PCI, while 5% and 1% experienced SOB and palpitations respectively but no one had syncope. Table 2 shows the frequency of recurrence of these symptoms, table 3 shows the frequency of tiredness and figure 3 illustrates the assessment of limitations towards different ranges of activities.

When assessing the Emotional and Social Components of HRQoL, 3% reported to have emotional problems that severely interfere with their social activities while 58% reported to have never had had emotional issues (Table 4).
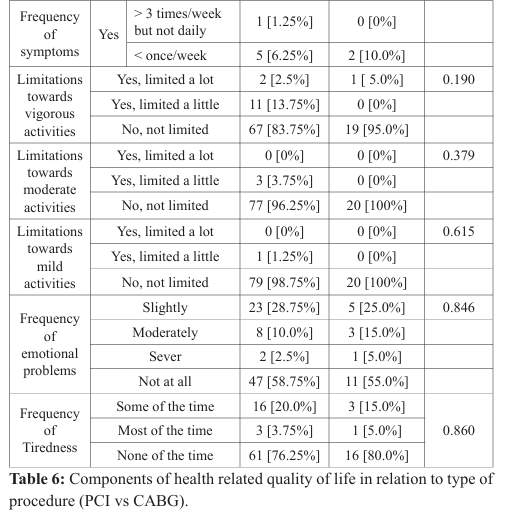
Compared to those who underwent CABG, patients who underwent PCI are significantly younger (p value: 0.019) and hypertensive (p value 0.001). In addition, they are insignificantly more likely to be diabetic (p value of 0.089). No significant difference in both groups in relation to gender and other risk factors for CAD (Table 5).

Discussion
Percutaneous coronary intervention (PCI) and coronary-artery bypass grafting (CABG) are both accepted and well recognized methods of revascularization in patients with Coronary Artery Disease (CAD). The clinical outcomes of both strategies have been demonstrated extensively and both proved to be better than medical therapy alone in well selected patients including the elderly. Treating Physicians use many tools and consider many other aspects, not only, coronary anatomy to decide which revascularization (CABG or PCI) individual’s patient to undergo, but also patient’s preference are considered equally important in this decision making process ,therefore, from a patient’s perspective, other considerations, like relief from angina, return to work and quality of life, may play a critical role in selecting a revascularization strategy .This study aimed at assessing health related quality of life (HRQoL)in patients with CAD who had undergone CABG or PCI at Alshaab Teaching Hospital(Khartoum, Sudan) and to the best of our knowledge there are no published study that investigate the same topic in Sudan or Sub-Saharan African (SSA) region.
Participants in this study are predominantly males and this is not different from what reported in different recent studies regrading gender make up of patients undergone revascularization procedures [12,24,25], about 60% of the total participants are of middle age (40–65 years) which in line with what’s believed-despite lack of convincing statistical data- that heart disease in Africa and SSA region particularly affects people at younger age.
80% of patients in this study had undergone PCI while only 20% had CABG. This can be explained by the fact that PCI is more frequently performed than CABG in clinical practice and considering also, this is a non-randomized and non-matched study.
In our study, we found no significant differences between PCI and CABG patients regarding demographics and background of risk factors except that patients who had PCI are younger and more likely to be hypertensive (p value: 0.019 and 0.001 respectively). It’s not strange as elderly more likely to have multi-vessels disease and hence CABG is more suitable alternative while younger are likely to have less extensive or severe CAD disease, hence, PCI is more attractive. In addition, younger, productive and active people might have preferred less invasive procedure like PCI.
In this study, we found no significant differences for all HRQoL components between patients who had undergone PCI or CABG. This finding is not surprising as noted before in a systemic review and meta-analysis that included Thirty-Four longitudinal studies published from January 2000 to December 2012 with a total of 15,992 patients (8,027 had undergone PCI, 6,348 CABG and 1,617 patients received medications), in which, both revascularization procedures (CABG and PCI) significantly improved HRQoL than medication. However, no significant difference observed between PCI and CABG [26]. In a quality-of-life sub study of Synergy between PCI with Taxus and Cardiac Surgery (SYNTAX), both CABG and PCI resulted in significant relief from angina and improvements in overall health status over the first year of followup. At both 6 and 12 months, there was a small but significant reduction in angina frequency with CABG as compared with PCI but these symptomatic benefits of CABG were counterbalanced by the more rapid recovery and improved short-term health status achieved with PCI [27].
More recently, HRQoL were significantly more favorable at 1year after PCI than with CABG in patients with unprotected left main CAD in the pre-specified quality-of-life analysis of the landmark EXCEL (Evaluation of Xience Versus Coronary Artery Bypass Surgery for Effectiveness of Left Main Revascularization) trial. A difference that no longer significant by 3 years of follow-up [28].
Our study has many limitations, firstly it’s a cross - sectional design with small sample. Longitudinal study with more participants and long follow-up period would have been better. Secondly, this study reports the post-procedural results without baseline preinterventional assessment to compare with. Finally, the study only had a general measure of HRQoL, it would be ideal to evaluate both general and disease-specific HRQoL.
Conclusion
In this study, we found no significant difference between PCI and CABG patients concerning physical, emotional and social components of HRQoL.
References
- Favaloro RG. Saphenous vein autograft replacement of severe segmental coronary artery occlusion: operative technique. Ann Thorac Surg. 1968; 5: 334-339.
- Garret HE, Dennis EW, De Bakey ME. Aortocoronary bypass with saphenous vein graft. Seven-year follow up. JAMA. 1973; 223: 792-794.
- Grüntzig AR, Senning A, Siegenthaler WE. Nonoperative dilatation of coronary- artery stenosis: percutaneous transluminal coronary angioplasty. N Engl J Med. 1979; 301: 61-68.
- Sigwart U, Puel J, Mirkowitch V, et al. Intravascular stents to prevent occlusion and restenosis after transluminal angioplasty. N Engl J Med. 1987; 316: 701-706.
- Jeremias A, Kaul S, Rosengart TK, et al. The impact of revascularization on mortality in patients with nonacute coronary artery disease. Am J Med. 2009; 122: 152-161.
- BARI Investigators. Five year clinical and functional outcome comparing bypass surgery and angioplasty in patients with multivessel coronary disease. A multi- center randomized trial. JAMA. 1997; 9: 715-721.
- Serruys PW, Unger F, Sousa JE, et al. Comparison of coronary artery bypass surgery and stenting for the treatment of multivessel disease. N Engl J Med. 2001; 344: 1117-1124.
- SoS Investigators. Coronary artery bypasses surgery versus percutaneous coronary intervention with stent implantation in patients with multivessel coronary artery disease (the Stent or Surgery trial): a randomized controlled trial. Lancet. 2002; 360: 965-970.
- Serruys PW, Ong AT, van Herwerden LA, et al. Five-year outcomes after coronary stenting versus bypass surgery for the treatment of multivessel disease: the final analysis of the Arterial Revascularization Therapies Study (ARTS) randomized trial. J Am Coll Cardiol. 2005; 46: 575-581.
- Bravata DM, Gienger AL, McDonald KM, et al. Systematic review: the comparative effectiveness of percutaneous coronary interventions and coronary artery bypass graft surgery. Ann Intern Med. 2007; 147: 703-716.
- Hlatky MA, Boothroyd DB, Bravata DM, et al. Coronary artery bypass surgery compared with percutaneous coronary interventions for multivessel disease: a collaborative analysis of individual patient data from ten randomised trials. Lancet. 2009; 373: 1190-1197.
- Serruys PW, Morice MC, Kappetein AP, et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009; 360: 961-972.
- Kolh P, Windecker S, Alfonso F, et al. 2014 ESC/ EACTS guidelines on myocardial revascularization: the Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for CardioThoracic Surgery (EACTS). Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur J Cardiothorac Surg. 2014; 46: 517-592.
- Fihn SD, Blankenship JC, Alexander KP, et al. 2014 ACC/ AHA/AATS/PCNA/SCAI/STS focused update of the guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines, and the American Association
- for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2014; 64: 1929-1949.
- Official records of the world health organization. In: WHO. 1948. Geneva.
- Sawatzky JA, Naimark BJ. Coronary artery bypass graft surgery: exploring a broader perspective of risks and outcomes. J Cardiovasc Nurs. 2009; 24: 198-206.
- Bowling A. Measuring Disease. New York: Open University Press Inc. 2001.
- Patrick DL, Burke LB, Powers JH, et al. Patient-reported outcomes to support medical product labeling claims: FDA perspective. Value Health. 2007; 10: 125-137.
- Jokinen JJ, Hippelainen MJ, Turpeinen AK, et al. Healthrelated quality of life after coronary artery bypass grafting: a review of randomized controlled trials. J Card Surg. 2010; 25: 309-317.
- Sun JH, Wu XY, Wang WJ, et al. Cognitive dysfunction after off-pump versus on-pump coronary artery bypass surgery: a meta-analysis. J Int Med Res. 2012; 40: 852-858.
- Cormack F, Shipolini A, Awad WI, et al. A meta-analysis of cognitive outcome following coronary artery bypass graft surgery. Neurosci Biobehav Rev. 2012; 36: 2118-2129.
- Blankenship JC, Marshall JJ, Pinto DS, et al. Effect of percutaneous coronary intervention on quality of life: a consensus statement from the Society for Cardiovascular Angiography and Interventions. Catheter Cardiovasc Interv. 2013; 81: 243-259.
- Soo Hoo SY, Gallagher R, Elliott D. Systematic review of healthrelated quality of life in older people following percutaneous coronary intervention. Nurs Health Sci. 2014; 16: 415-427.
- Abdallah MS, Wang K, Magnuson EA, et al. for the FREEDOM Trial Investigators. Quality of life after PCI vs CABG among patients with diabetes and multivessel coronary artery disease: a randomized clinical trial. JAMA. 2013; 310: 1581-1590.
- Stone GW, Sabik JF, Serruys PW, et al. for the EXCEL Trial Investigators. Everolimus-eluting stents or bypass surgery for left main coronary artery disease. N Engl J Med. 2016; 375: 2223-2235.
- Takousi MG, Schmmer S, Troop NA , et al. for the HealthRelated Quality of Life after Cornonary Revascularization: A systematic review with meta-analysis. Hellenic Journal of Cardiology. 2016; 57: 223-237.
- Cohen DJ, Van Hout B, Serruys PW, et al. for the SYNTAX Investigators. Quality of life after PCI with drug-eluting stents or coronary-artery bypass surgery. N Engl J Med. 2011; 364: 1016-1026.
- Baron SJ, Kappetein P, Cohen DJ, et al. for the Quality-ofLife After Everolimus-Eluting Stents or Bypass Surgery for Left-Main Disease: Results From the EXCEL Trial. J Am Coll Cardiol. 2017; 25: 3113-322.