Idiopathic Aortic Thrombosis and Thromboembolism in Young Women
Author(s): Suyue M. Zhang M.D, Gaurang Joshi M.D, Rym El Khoury M.D, Benjamin Parker B.S, Andrii Labchuk M.D, Chad E. Jacobs M.D, John V. White M.D and Lewis B. Schwartz M.D*
Department of Surgery, Advocate Lutheran General Hospital, Park Ridge, IL.
*Correspondence:
Lewis B. Schwartz, M.D, Clinical Professor of Surgery, University of Illinois, Department of Surgery, Advocate Lutheran General Hospital, 1775 Dempster St., Park Ridge, IL 60068, Tel: 847-384-1420
Received: 01 Mar 2022; Accepted: 30 Mar 2022; Published: 04 Apr 2022
Citation: Zhang SM, Joshi G, El Khoury R, et al. Idiopathic Aortic Thrombosis and Thromboembolism in Young Women. Cardiol Vasc Res. 2022; 6(2): 1-4.
Abstract
Introduction: Spontaneous aortic thrombosis causing distal embolization and acute limb ischemia is an ominous medical condition with a poor prognosis. Herein are reported the clinical courses of two women who presented with severe lower extremity ischemia caused by distal embolization of spontaneous aortic thrombus without obvious antecedent arterial disease. This unusual diagnosis should be expected in patients presenting with persistent lower extremity pain and numbness even in the absence of overt physical findings.
Case 1: A 42 year-old woman with mild hyperlipidemia complained of left leg numbness and weakness. She was treated with analgesia but her symptoms worsened. Lower extremity ultrasound revealed a significant infra-inguinal perfusion defect; computed tomography revealed mural thrombus in a normal aorta along with extensive thrombotic occlusion of the left popliteal and tibial arteries. Attempts at endovascular recanalization were unsuccessful; the patient underwent successful left popliteal-to-plantar artery bypass with autologous vein.
Case 2: A 57 year-old woman without medical history presented to a local Emergency Room with a five-day history of numbness in the right lower extremity. Computed tomographic angiography revealed complete infrarenal aortic occlusion in a 3 cm diameter area of mild aortic ectasia along with iliac and distal right infrainguinal thromboembolism. The patient was treated with aortobifemoral bypass grafting with right leg fasciotomy, which restored perfusion and function.
Conclusion: Spontaneous aortic thrombosis causing distal embolization and acute limb ischemia is an ominous medical condition with a poor prognosis. Episodes of embolization may be intermittent and asymptomatic such that, when symptoms finally occur, the distal thrombus is often chronic and inaccessible. The diagnosis should be suspected in patients with unexplained lower extremity symptoms and pulse deficits; it can be readily established with computed tomography.
Keywords
Introduction
Aortic mural thrombus and/or thrombosis is an uncommon but serious medical condition that can generate significant morbidity and mortality [1-12]. Its causes are many and include aortic pathology as well as hematologic disorders. Rarely, the syndrome of aortic thrombosis occurs spontaneously in the absence of an obvious etiology. Reported herein are two cases of aortic thromboembolism that occurred in relatively young women without underlying arterial or serologic pathology.
Case Reports
Case 1
A 42-year-old woman with a history of smoking, oral contraceptive use, mild hyperlipidemia, endometriosis and possible radiation exposure (living in Poland at the time of the Chernobyl nuclear disaster) complained of left leg numbness and weakness. She ascribed the problem to her employment wherein she spent long hours seated at a computer. Lower extremity venous duplex was negative except for mild varicosity. Historical lower extremity arterial Doppler revealed ankle-branchial indices >1.0 bilaterally at rest. MRI of the left leg was normal. Two-view radiographic evaluation of the lumbar spine demonstrated multilevel disc degeneration and spondylosis without acute abnormality.
She was treated with analgesics but her condition worsened. She noticed cramping in the left calf after walking inclines or short distances. Computed tomographic angiography of the aorta and runoff within a month of initial presentation revealed mural thrombus in a normal-appearing aorta along with left popliteal occlusion in a normal-appearing distal vasculature (Figure 1). Contrast diagnostic angiography revealed a widely patent left femoral bifurcation, abrupt occlusion of the left popliteal artery and reconstitution of the left plantar artery via the posterior tibial artery (Figure 2). Echocardiogram revealed normal wall motion and valves with left ventricular ejection fraction of 65% and the absence of atrial thrombus. An attempt at endovascular treatment of the popliteal occlusion was unsuccessful.

Figure 1: Computed tomographic angiography in a 42-year-old female showing aortic mural thrombus (Left panel) along with left popliteal artery occlusion (Right panel).
The patient subsequently underwent left superficial femoral artery- to-distal posterior tibial artery bypass grafting using non-reversed, translocated, left great saphenous vein. The procedure was uncomplicated but the foot was not sufficiently re-perfused and Doppler signals suggested poor outflow or occlusion. Therefore, the patient was returned to the Operating Room on post-operative day #2 and re-explored. Acute graft thrombosis was discovered. A graft thrombectomy was performed and a more distal pedal target procured. A composite vein graft using the previous left saphenous vein graft and a segment of the right great saphenous vein with distal anastomosis to the left plantar artery was created (Figure 3). This effectively re-perfused the left foot. The patient was discharged on long-term anticoagulation on post-operative day #5.
Follow-up after two years demonstrated a widely patent femoro- pedal bypass.
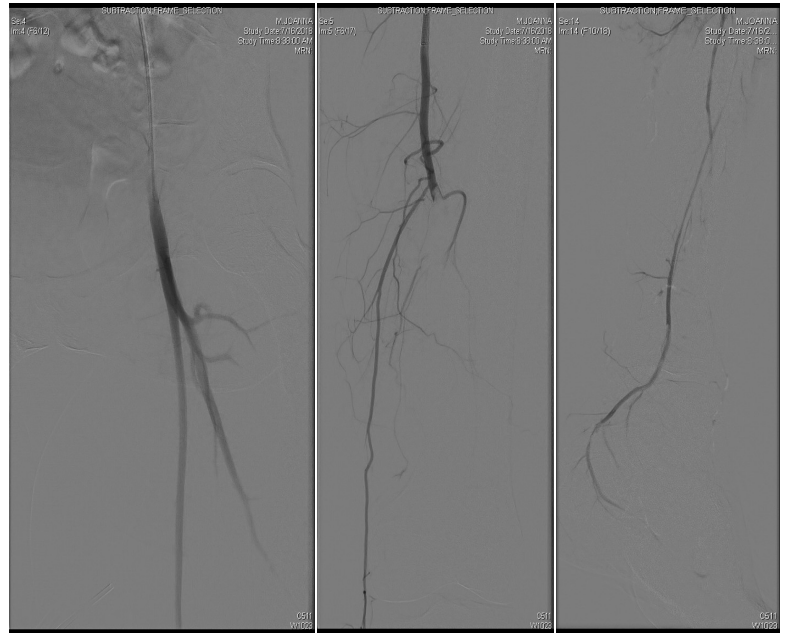
Figure 2: Contrast diagnostic angiography in a 42-year-old female showing a widely patent left femoral bifurcation (left panel), abrupt occlusion of the left popliteal artery (middle panel) and reconstitution of the left plantar artery via the peroneal artery (right panel).
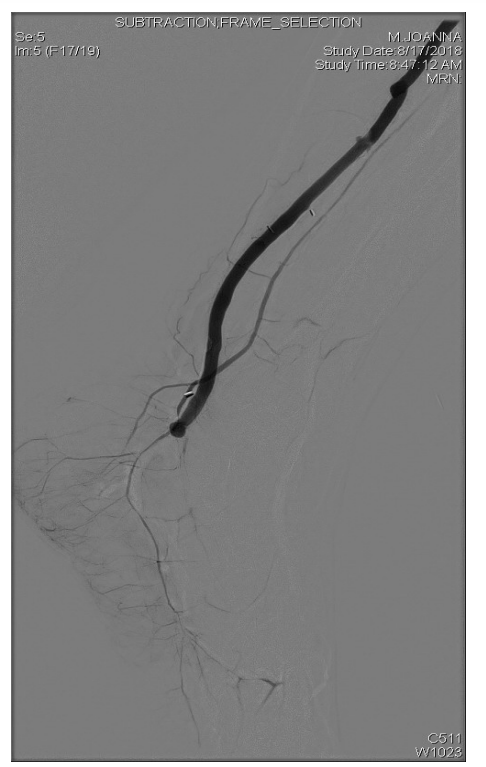
Figure 3: Intra-operative completion angiography following left superficial femoral artery to left plantar artery bypass using composite saphenous vein. Note the distal anastomosis to the left plantar artery.
Case 2
A 57-year-old woman with a smoking history noted the insidious onset of numbness in the right lower extremity along with pain and cramping. Initially her symptoms were intermittent, however, the pain worsened so she sought attention in a local Emergency Room. Doppler ultrasound revealed monophasic pedal waveforms bilaterally with a parvus tardus pattern suggestive of inflow occlusion. Computed tomographic angiography revealed complete occlusion of the infrarenal abdominal aorta with large, inferior epigastric and intercostal collaterals reconstituting the common femoral arteries bilaterally (Figure 4).

Figure 4: Acute aortic occlusion in a 57-year-old female. Note the complete occlusion of the infrarenal aorta (Left panel) as well as reconstitution of the femoral arteries bilaterally via collateralization (Right panel).
The patient was transferred to our institution and anticoagulated with heparin. She was explored via a midline incision, the retro peritoneum entered and the infrarenal aorta isolated. Small, pulseless common femoral arteries were exposed and isolated via bilateral groin incisions. Her infrarenal aorta was divided revealing occlusion by fresh thrombus. The thrombus was gently removed from the proximal aorta with the aid of a 7 French embolectomy catheter. After restoration of inflow, a previously positioned infrarenal aortic clamp was applied. End-to-end aortobifemoral bypass was performed uneventfully using a bifurcated 16 mm x 8 mm Dacron graft. Upon removal of the surgical drapes, the left foot appeared well perfused and warm and pedal pulses were palpable. However, the right foot remained cool and slightly mottled prompting re-exploration of the right groin. Strong pulses were identified in the right aortofemoral graft limb, native superficial femoral and profunda femoris arteries. There was no retained thrombus. A 4 French embolectomy catheter advanced to the level of the ankle easily. No thrombus was returned. The arteriotomy and groin were closed and four-compartment fasciotomy of the right calf was performed through two longitudinal incisions.
In recovery, the right leg re-perfused slowly. Its color and Doppler signals eventually returned and the patient’s symptom resolved. She was orally anticoagulated and discharged to home after five days. Her right foot remained warm although she complained of some residual foot drop and numbness.
The patient recovered completely and returned to walking and gardening. She remains well and asymptomatic two years after aortobifemoral bypass. She is being treated with rivaroxaban indefinitely.
Discussion
Primary aortic thrombosis and thromboembolism can be difficult to recognize, engender substantial morbidity and mortality, and be challenging to effectively treat [3,13]. Most cases are due to underlying aortic pathology such atherosclerosis, abdominal aortic aneurysm, aortic dissection, blunt trauma and/or penetrating aortic ulceration. Occasionally, aortic mural thrombus or complete thrombosis may be a sequela of a severe, systemic illness or malignancy [2,7]. Truly idiopathic aortic thrombosis is a rare clinical entity; only a few hundred reports can be found within the English literature [1-12].
The diagnosis of aortic thrombosis is made either incidentally during radiographic evaluation for another medical condition or as a result of symptomatic distal embolization to abdominal viscera or the lower extremities [13]. Interestingly, several authors have noted a female predilection for this rare clinical entity [2,3,13]. As the two cases presented herein illustrate, the condition may be insidious as embolism to end-arteries with small angiosomes may be subclinical. These episodes may generate only minor and vague symptoms which may be discounted by primary physicians following young patients [14]. One could hardly expect any primary physician to correctly identify a complaint of intermittent foot numbness as aortic thrombosis. Nonetheless, if non-specific symptoms persist and are unresponsive to medical therapy, the diagnosis of this unusual syndrome is easily established through computed tomography.
Treatment is aimed at relief of the associated ischemic syndrome, most commonly in the lower extremities [13]. In this regard, chemo-mechanical thrombolysis, surgical thrombectomy and bypass grafting have all been found to be effective. Although chronic anticoagulation has often been utilized to good effect (and was the chosen treatment in the first case presented herein), open aortic surgical thrombectomy is probably the most durable and effective approach [2,6,7].
Even more controversial is the treatment of primary aortic mural thrombus (PAMT) when diagnosed in the asymptomatic patient, most often by tomographic imaging performed for other indications. As the cases presented herein imply, peripheral embolization from seemingly quiescent aortic clot can generate profound ischemia with significant loss of functionality in young, previously healthy patients. It is reasonable therefore, in the endovascular era, to consider minimally invasive coverage of potentially threatening lesions, similar to the burgeoning field of atrial appendage closure in patients with atrial fibrillation [15]. Indeed, some authors have suggested that only an aggressive approach to ominous PAMT will meaningfully reduce morbidity [11,13].
Conclusion
Idiopathic aortic mural thrombus and thromboembolism is an uncommon but potentially dangerous medical condition that can create significant morbidity and mortality. Reported herein are two cases of aortic thromboembolism that occurred in relatively young women without underlying obvious arterial or serologic pathology. This unusual diagnosis should be expected in patients presenting with persistent lower extremity pain and numbness even in the absence of overt physical findings.
References
- Rossi PJ, Desai TR, Skelly CL, et al. Paravisceral aortic thrombus as a source of peripheral embolization-Report of three cases and review of the literature. J Vasc Surg. 2002; 36: 839-843.
- Fayad ZY, Semaan E, Fahoum B, et al. Aortic mural thrombus in the normal or minimally atherosclerotic aorta. Ann Vasc Surg. 2013; 27: 282-290.
- Meyermann K, Trani J, Caputo FJ, et al. Descending thoracic aortic mural thrombus presentation and treatment strategies. J Vasc Surg. 2017; 66: 931-933.
- Patrício C, Silva MM, Silva PE, et al. Massive organ embolization from primary aortic thrombosis. Rev Port Cardiol. 2018; 37: 447.e1-e6.
- Hahn TL, Dalsing MC, Sawchuk AP, et al. Primary aortic mural thrombus: Presentation and treatment. Ann Vasc Surg. 1999; 13: 52-59.
- Valdivia AR, Santos AD, Urena MG, et al. Anticoagulation alone for aortic segment treatment in symptomatic primary aortic mural thrombus patients. Ann Vasc Surg. 2017; 43: 121- 126.
- DeKornfeld GM, Boll J, Ziegler KR, et al. Initial and intermediate-term treatment of the phantom thrombus (primary non-occlusive mural thrombus on normal arteries). Vasc Med. 2018; 23: 549-554.
- Marin-Acevedo JA, Koop AH, Diaz-Gomez JL, et al. Non- atherosclerotic aortic mural thrombus: a rare source of embolism. BMJ Case Rep. 2017.
- Stranges D, Lucerna A, Espinosa J. Primary aortic mural thrombus presenting with multiple simultaneous embolic phenomena. Vis J Emer Med. 2017; 8: 63-64.
- Machleder HI, Takiff H, Lois JF, et al. Aortic mural thrombus: an occult source of arterial thromboembolism. J Vasc Surg. 1986; 4: 473-478.
- Borghese O, Pisani A, Di Centa I. Symptomatic aortic mural thrombus treatment and outcomes. Ann Vasc Surg. 2020.
- Tsilimparis N, Hanack U, Pisimisis G, et al. Thrombus in the non-aneurysmal, non-atherosclerotic descending thoracic aorta - an unusual source of arterial embolism. Eur J Vasc Endovasc Surg. 2010; 41: 450-457.
- Verma H, Meda N, Vora S, et al. Contemporary management of symptomatic primary aortic mural thrombus. J Vasc Surg. 2014; 60: 1524-1534.
- Buccia F, Fiengob L, Hamatia S, et al. Abdominal aortic occlusion of young adults. Interactive CardioVascular and Thoracic Surgery. 2012; 14: 99-101.
- Reddy VY, Sievert H, Halperin J, et al. Percutaneous left atrial appendage closure vs warfarin for atrial fibrillation: A randomized clinical trial (PROTECT AF). JAMA. 2014; 312: 1988-1998.