Immune-Modulators and Thyroid Function in Oncological Patients with Hashimoto 'S Thyroiditis
Author'(s): Matozza Francesco1, Artero Guillermo H2, Artero Guillermo2, Levy Daniel4 and Carvallo Héctor5
1Service du Neuroradiologie, Hopital Henri-Mondor, Creteil,France.
2Farmacéutico, Biopharmacie, France.
3Former Chief, Dept. Oncology, Htal. Rivadavia, Argentina.
4Endocrinologist, Member of S.A.E.M., Prof. Internal Medicine,Argentina.
*Correspondence:
Hector Carvallo, Endocrinologist, Member of S.A.E.M., Prof. Internal Medicine, Argentina.
Received: 08 May 2021; Accepted: 10 June 2021
Citation: Francesco Matozza, Guillermo Artero H, Guillermo Artero, et al. Immune-Modulators and Thyroid Function in Oncological Patients with Hashimoto S Thyroiditis. Cancer Sci Res. 2021; 4(2): 1-3.
Abstract
Hashimoto's thyroiditis (HT) is a form of chronic lymphocytic thyoriditis, of autoimmune origin and multiple physiopathogenic pathways, which may or may not be associated with other autoantibody diseases, both endocrinological (P.A.S.) and non-endocrinological (M.A.S.). Likewise, HT can coincide -in the same patient- with very varied oncological pathologies, with which it can interact in a usually negative way. In this article, the benefit achieved in cancer patients who also had HT is evaluated through the use of immune-modulators.
Keywords
Introduction
Hashimoto's thyroiditis (HT) is the most common cause of hypothyroidism worldwide (0.3-1.5 cases per 1,000 individuals per year) [1]. It is 7 times more frequent in the female sex. It is considered a disease of autoimmune origin, although a large number of dissimilar factors affect its physiopathogenesis [2,3]. Likewise, an increased incidence of cancer has been observed and confirmed in patients with autoimmune diseases [4].
Laboratory Findings at HT (Figure 1)
1- Subclinical hypothyroidism (SCH)
Normal T3 and T4 Increased TSH Increased ATG (antithyroglobulin)
2- Clinical hypothyroidism (CH)
Decreased T3 and T4 Increased TSH
Increased anti-thyroid peroxidase (anti-TPO)
Increased antithyroglobulin (anti-Tg)
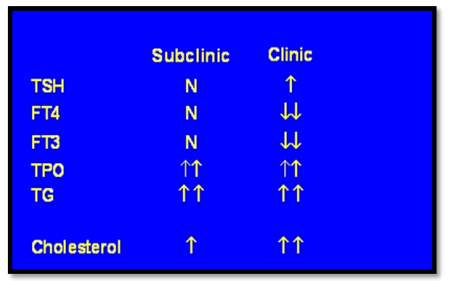
Figure 1: HT Laboratory Findings.
Objectives
We proceeded to demonstrate the beneficial effect of immunemodulators in patients with Hashimoto's Thyroiditis, who had different types of oncological pathologies.
Patients and Methods
161 patients with Hashimoto's thyroiditis and different types of tumors were retrospectively evaluated in a multicenter study (Figure 2). Their age ranged from 40 to 70 years; 90% female. 98 patients received cancer treatment plus immune-modulators and levothyroxine for 8 months.63 patients received only cancer treatment and levothyroxine as a control group, during the same period (Figure 3).
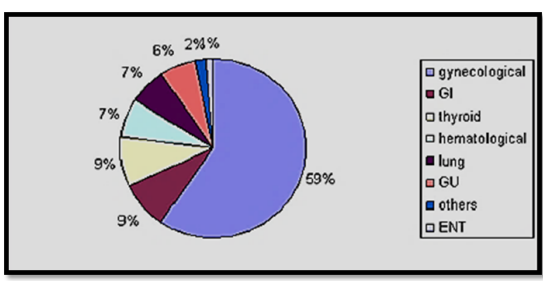
Figure 2: Types of tumors in the subjects that were controlled.
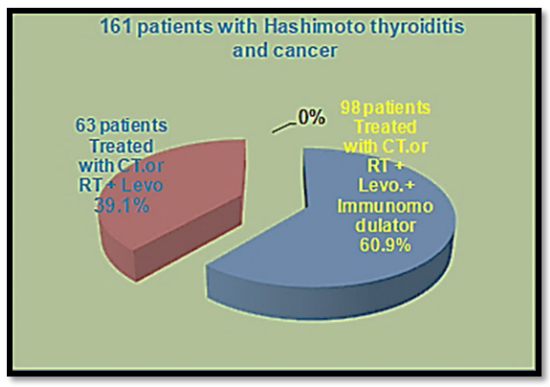
Figure 3: Distribution of patients with and without immune-modulators.
Immune-Modulator
The immune-modulator, which was used, is composed of Zinc, Selenium, Magnesium and Astragalus extract (Astragalus membranaceus) [5,6]. The constituents of this last compound are: glycosides, polysaccharides, isoflavone-type flavonoids, sucrose, phytosterols, such as beta-phytosterol. Astragalus has immune stimulating properties; it increases immune response, increases the activity of T lymphocytes and the absolute number of lymphocytes, stimulates the natural production of interferon and enhances its activity (Figure 4 and 5).

Figures 4 & 5: A. membranaceus flowers and roots
Simultaneously, it decreases immune hyperactivity in patients with systemic lupus erythematosus and myasthenia gravis. Selenium decreases antiperoxidase levels in patients with Hashimoto's thyroiditis [7].
Method
T3, T4, TSH, TPO and TG antibodies were measured before, during, and up to 8 months after treatment with immune-modulators. The immune-modulators were administered orally, sublingually, at a dose of 4 ml per day.
Results
87 patients (78.5%) treated with Immunomodulators showed an increase in T3, T4 and a decrease in TSH, TPO and TG antibodies, two months after starting treatment. 8 (8.16%) patients showed no changes in thyroid function. 3 patients (3.06%) abandoned the treatment. Objectively, an increase in white blood cells, red blood cells, improvement of dry skin, asthenia, depression and intolerance to cold were observed. Subjectively, we observed a better quality of life in these patients treated with Immune- modulators (Figure 6).
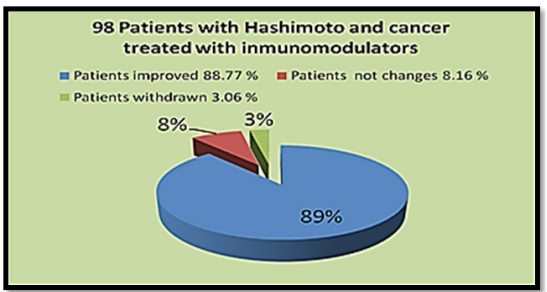
Figure 6: Results.
The control group did not show changes in thyroid function or variations in antibody levels (Figure 7).
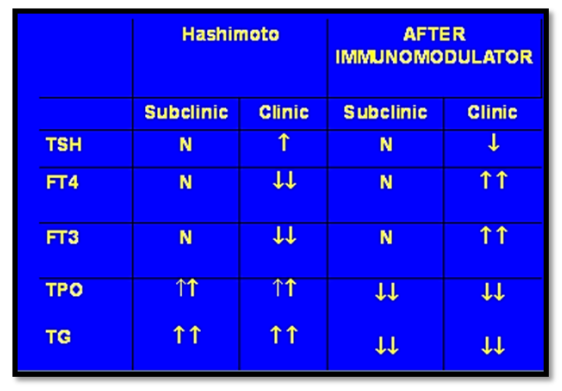
Figure 7: Subjects´lab findings during study.
Conclusions
Immune-modulators are well tolerated and have no side effects.
They improve thyroid function in patients with Hashimoto's thyroiditis.
In cancer patients, immune-modulators also improve red blood cells, white blood cells, regulate platelets and improve the disease- free period.
As secondary findings, we may say that women with Hashimoto's thyroiditis should have gynecological and imaging examinations (mammography, breast ultrasound, transvaginal ultrasound, and PAP) more frequently, since they are more likely to develop benign or malignant gynecological lesion
On the other hand, in patients with uterine fibroids, ovarian cysts, and / or mammary dysplasia, thyroid function (T3, T4, TSH, APTO, and ATG) should be studied routinely to rule out Hashimoto's disease.
Immune-modulators are the best allies of cancer patients during and after chemo or radiotherapy treatment.
They stimulate the immune system and improve the quality of life of these patients. In patients with coexisting Hashimoto's thyroiditis, immune-modulators show a marked clinical and laboratory improvement, with a marked reduction in supplementary hormone therapy.
References
- Piraino, Patricia N, Sepúlveda, et al. Hashimoto chronic thyroiditis. Retrospective analysis of 228 patients. Revista Medica de Chile. 2018; 138: 827-831.
- Kahaly GJ. Polyglandular autoimmune síndromes. European Journal of Endocrinology. 2009.
- Ben-Skowronek, Michalczyk A, Piekarsk R. Type III Polyglandular Autoimmune Syndromes in children with type 1 diabetes mellitus I. 2013.
- Angela Lopomo, Sonia Berrih-Aknin. Autoimmune Thyroiditis and Myasthenia Gravis. Front Endocrinol Lausanne. 2017; 8: 169.
- Mazokopakis EE, Papadakis JA, Papadomanolaki MG, et al. Effects of 12 months treatment with L-selenomethionine on serum anti-TPO Levels in Patients with Hashimoto's thyroiditis. Thyroid. 2007; 17: 609-612.
- Mazokopakis EE, Chatzipavlidou V. Hashimoto's thyroiditis and the role of selenium. Current concepts. Hell J Nucl Med. 2007; 10: 6-8.
- Kaprara A, Krassas GE. Selenium and thyroidal function the role of immunoassays Hell J Nucl Med. 2006; 9: 195-203.