Ketamine plus Cervical Sympathetic Blockade (CSB) Seems to be Significantly More Effective in Reducing the Symptoms of PTSD and Depression than CSB alone in a PTSD Cohort
Author'(s): Eugene Lipov1,2*, Hunter Rolain3 and Luke Lammers3
1Stella Center, Westmont, IL, USA.
2Department of Surgery, University of Illinois, Chicago, IL, USA.
3Midwestern University - Chicago College of Osteopathic Medicine, Downers Grove, IL, USA.
*Correspondence:
Eugene Lipov, Stella Center, 1 Oak Hill Dr, Unit 100, Westmont,IL 60559, USA.
Received: 03 May 2024; Accepted: 12 Jun 2024; Published: 20 Jun 2024
Citation: Eugene Lipov, Hunter Rolain, Luke Lammers. Ketamine plus Cervical Sympathetic Blockade (CSB) Seems to be Significantly More Effective in Reducing the Symptoms of PTSD and Depression than CSB alone in a PTSD Cohort. Anesth Pain Res. 2024; 8(2): 1-5.
Abstract
Purpose: A significant number of Americans have symptoms of Post-Traumatic Stress Disorder (PTSD) and depression. Cervical sympathetic block (CSB) combined with sub-anesthetic ketamine infusions (KI) have been shown to reduce the symptoms of PTSD and depression via a synergistic effect. We aim to report a significant improvement of PTSD and depressive symptoms by concordant use of CSB and KI as compared to CSB alone.
Methods: 26 consecutive patients were recruited to study the effects of KI and bilateral CSB vs bilateral CSB alone on sleep via a WHOOP band analysis. Patients were randomized to receive CSB alone vs KI and CSB. Patients received KI and CSB via clinic protocol.
Results: Patients (n=11) that received CSB only, demonstrated a PCL reduction of 56.1% and BDI reduction of 59.5%. Patients (n=12) that received CSB and KI together, demonstrated a PCL reduction of 76.9% and a BDI reduction of 83.7%.
Conclusion: Bilateral CSB combined with KI seems to be more effective in treating PTSD and depression symptoms as compared to bilateral CSB alone. Considering the size of the study, a larger scale evaluation would be necessary to confirm our findings.
Keywords
Introduction
More than 10% of Americans will develop Post-Traumatic Stress Disorder (PTSD) at some point in their lives, with 3.7% experiencing PTSD during any given year [1]. According to the World Health Organization, approximately 5% of the global population suffers from depression [2]. Cervical Sympathetic Blockade (CSB) has shown recent promise for controlling the symptoms of PTSD and depression [3-6]. Ketamine, an NMDA- antagonist, has been utilized at low-doses for the treatment of mental health disorders, such as treatment-resistant depression [7] and PTSD [8]. A case report has demonstrated the synergistic impact of KI and CSB modalities as related to the treatment of PTSD and depressive symptoms as well as a possible mechanism of the effect [9]. The patients included in the current report were recruited for a study titled, “The Impact of stellate ganglion block (SGB) on subjective and physiological measures of sleep quality and wellbeing.” Protocol # 2021/HE002777. The main findings of the above study were a significant improvement in subjective sleep quality, without documented physiological changes of sleep as measured by WHOOP wristband analysis. The focus of this current report is the improvement of PTSD and depression symptoms following bilateral CSB and KI as opposed to bilateral CSB treatment alone. The impact of the above therapies on sleep will be published at a different time. With the current therapeutic modalities of psychotherapy and pharmaceuticals to treat PTSD having low efficacy and low compliance rate [10], more effective treatment modalities are highly required and should be researched.
Methods Patients and Setting
All patients consented to IRB Protocol #2021/HE002777. A total of 26 consecutive patients with a diagnosis of PTSD using the PTSD Checklist (PCL-5), consented to participate in a WHOOP study from 2022 to 2023. These individuals were included across various Stella Centers across the USA. Routine collection of pre- and post-intervention psychiatric assessment tools were collected.
Cervical Sympathetic Blockade
Detailed informed consent was obtained prior to all procedures for CSB on the right side. The patient was placed in the supine position with the head rotated slightly to the contralateral side, with monitoring per clinic protocol. The skin of the neck was cleaned with chlorhexidine-isopropyl alcohol preparation and 2 g of sterile ultrasound gel was applied. The neck was scanned using a broadband linear transducer (8-13 MHz from the level of the 6th to the 4th cervical vertebrae in transverse view). The skin at the injection site on the lateral neck was anesthetized with 1.5 mL of 1% lidocaine. Utilizing an in-plane approach, under real-time ultrasound guidance, a 22-gauge echogenic needle was placed just dorsal to the ventral fascia of the longus coli, medial to the longus capitus. After attempted aspiration, while monitoring the patient, 0.5 mL of 0.5% bupivacaine was injected, and after observing the patient for 30 s, a second 4 mL aliquot was injected. The patient was monitored for an additional 30 s. After the patient verbally confirmed an absence of any concerning symptoms, an additional 4 mL of 0.5% bupivacaine was slowly injected over 1 min for a total injection volume of 8 mL for a single-level block. This was repeated at the 4th cervical level, with a total of 4 mL of bupivacaine. Left-sided CSB was performed at a later date.
Ketamine Infusion
Detailed informed consent was obtained prior to all infusions following a consultation. The initial infusion of racemic ketamine hydrochloride (0.5 mg/kg) was administered over 45 min. Premedication with ondansetron 4 mg IVP was used for all sessions and an anesthesiologist was present until discharge. During the infusion, a nurse recorded vital signs (heart rate, blood pressure, respirations, pulse oximetry) and clinical status every 5 min. Any concerning or intolerable treatment-emergent side effects (e.g., hemodynamic instability, severe dissociation, worsening depression or anxiety) prompted intervention or discontinuation of the infusion. At the end of each infusion, the patient was clinically monitored for at least 1 h by the nursing staff. Subsequent infusions utilized escalating doses of ketamine of 0.1–0.2 mg/kg titrated to induce mild to moderate dissociation. A total of 4 KI were performed.
Psychiatric Outcome Measures
PTSD Checklist for DSM-V (PCL-5)
The PTSD Checklist for DSM-V (PCL-5) is a 20-item self- reported questionnaire that assesses PTSD symptomatology based on 20 symptoms outlined in the DSM-5. The purposes of this test include screening, diagnosis, and monitoring of symptomatology over a period of time. The patient is to self-report a score based on a 5-item Likert scale from 0 to 4, which is described by the following: 0) “Not at all”; 1) “A little bit”; 2) “Moderately”; 3) “Quite a bit”; and 4) “Extremely”. It should be noted that there are a number of differences between PCL-5 and PCL-4 (based on DSM-IV), hence they can neither be compared nor interchanged. The total symptom severity is a sum of the patient responses and may range from 0 to 80. A change in PCL-5 score by 5–10 points is considered reliable, and by 10–20 points is considered clinically significant. The optimally efficient minimum cutoff score that is considered diagnostic ranges from 31 to 33 [11].
Beck Depression Inventory
The Beck Depression Inventory (BDI) is a 21-item, self-report rating inventory that measures characteristic attitudes and symptoms of depression for the purpose of evaluating symptom severity [12]. The patient is to self-report a score based on a 4-item Likert scale from 0 to 3, which is described by the following: 0) “Symptom Absent”; and 4) “Severe Symptoms Present”. Score interpretation is dependent on a previous diagnosis of depression. A score greater than 20 without a previous diagnosis indicates depression. If a diagnosis of depression has already been made, the following score ranges can indicate the severity of symptoms: 0–13= minimal depression; 14–19 = mild depression; 20–28 = moderate depression; and 29–63 = severe depression [13]. According to the National Institute for Health and Care Excellence (NICE), a BDI score change greater to or equal than 3 signifies a clinically effective treatment for normal depression, and a BDI score change of 2 or greater for treatment-resistant depression [14].
Results
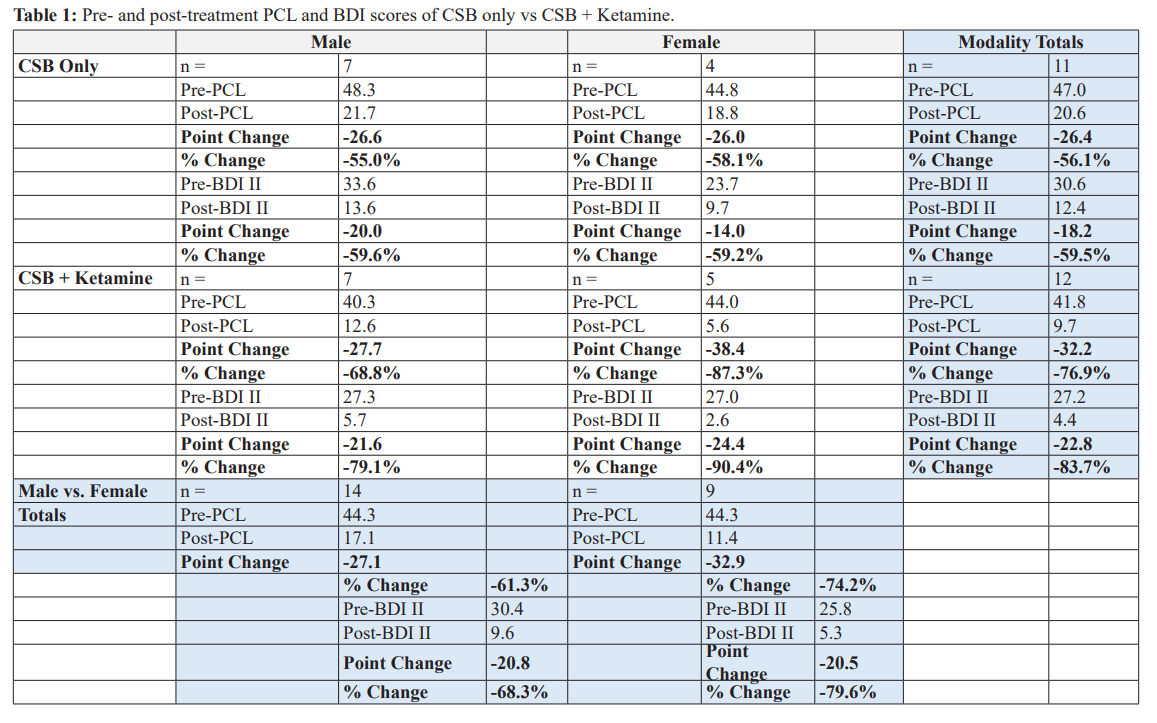
In a total of 11 patients (n = 11) who received bilateral CSB only, pre-PCL and pre-BDI scores were 47.0 and 30.6, respectively. Post-PCL and post-BDI scores were 20.6 (56.1% reduction) and 12.4 (59.5% reduction), respectively (Table 1).
In a total of 12 patients (n = 12) who received bilateral CSB plus ketamine, pre-PCL and pre-BDI scores were 41.8 and 27.2, respectively. Post-PCL and post-BDI scores were 9.7 (76.9% reduction) and 4.4 (83.7% reduction), respectively (Table 1).
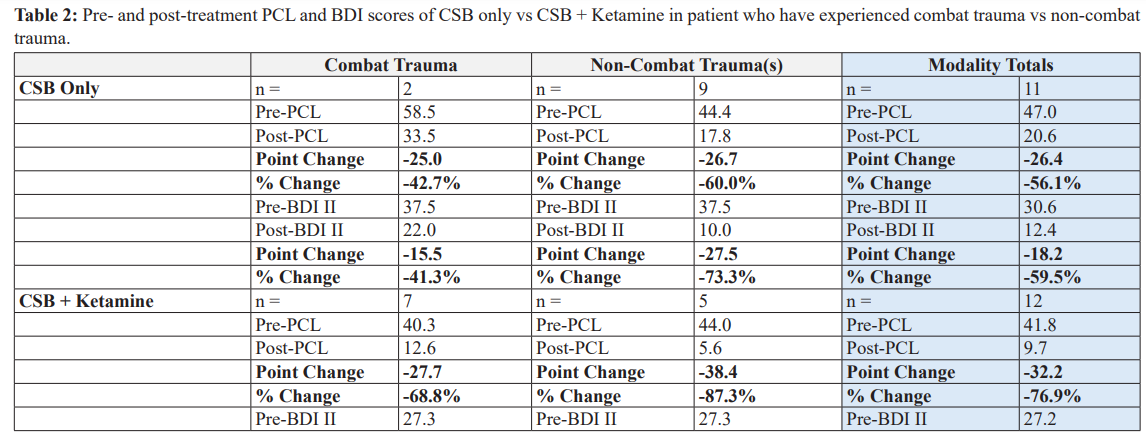
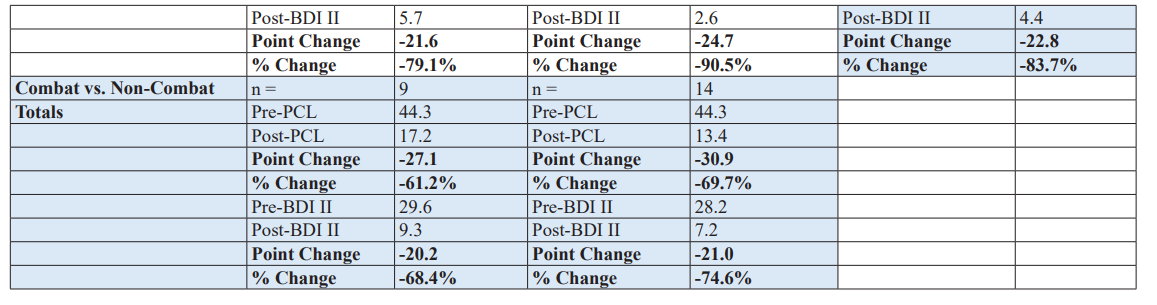
In a total of 2 patients (n = 2) who experienced combat trauma and received bilateral CSB only, pre-PCL and pre-BDI scores were 58.5 and 37.5, respectively. Post-PCL and post-BDI scores were 33.5 (42.7% reduction) and 22.0 (41.3% reduction), respectively(Table 2).
In a total of 7 patients (n = 7) who experienced combat trauma and received bilateral CSB plus ketamine, pre-PCL and pre-BDI scores were 40.3 and 27.3, respectively. Post-PCL and post-BDI scores were 12.6 (68.8% reduction) and 5.7 (79.1% reduction),respectively (Table 2).
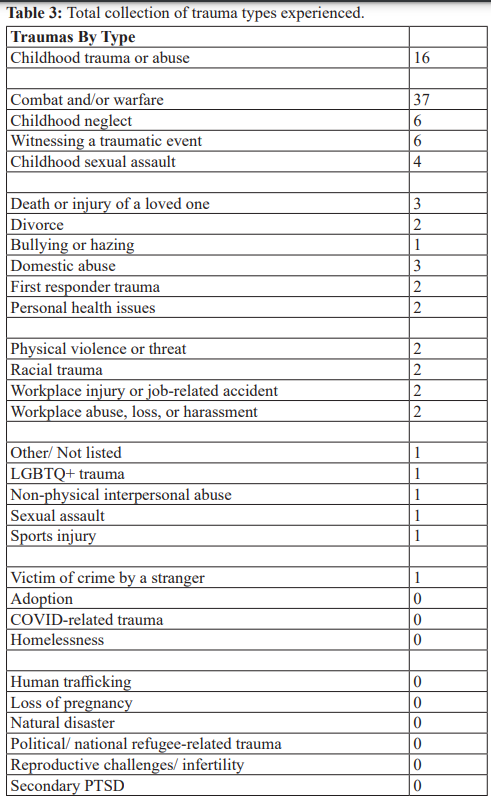
In a total of 9 patients (n = 9) who have experienced trauma, but not combat trauma, and received bilateral CSB only, pre-PCL and pre-BDI scores were 44.4 and 37.5, respectively. Post-PCL and post-BDI scores were 17.8 (60.0% reduction) and 10.0 (73.3% reduction), respectively (Table 3).
In a total of 5 patients (n = 5) who have experienced trauma, but not combat trauma, and received bilateral CSB plus ketamine, pre- PCL and pre-BDI scores were 44.0 and 27.3, respectively. Post- PCL and post-BDI scores were 5.6 (87.3% reduction) and 2.6 (90.5% reduction), respectively (Table 3).
In summary of the results, ketamine plus bilateral CSB treatment led to greater reduction of both PTSD and depression scores compared to bilateral CSB treatment alone.
Conclusion
Prior research has shown a mechanistic linkage of PTSD and depression symptoms to the over activation of the sympathetic nervous system (SNS) [15-20]. After trauma, sympathetic sprouting occurs due to increased neuronal growth factor (NGF) release. This ultimately leads to increased levels of norepinephrine (NE) which have been found in both the rat brain and human cerebrospinal fluid (CSF) of trauma patients [16-20]. This increase in sympathetic nerve fibers leads to the increase of NE concentration eventually producing the hyperarousal symptoms of PTSD [17] and depression[15] CSB is presumed to reverse NE levels, which was discussed in prior publication [17]. Theoretically, CSB affects depression via a similar mechanism. The mechanism of ketamine on reduction of PTSD and depression symptoms is currently still debated.
The theoretical reason for the observation of KI and CSB synergy was discussed in prior publication [9]. Essentially, KI is known to both induce sympathetic overgrowth, as well as reduce PTSD symptoms. CSB is believed to reduce sympathetic overgrowth by “pruning” the sympathetic sprouting and reducing NE. Thus, preventing the effects on the sympathetic fibers by KI, yet not affecting the positive effects of KI.
The current study demonstrated that combining KI and bilateral CSB has a more significant impact in treating PTSD and depression symptoms compared to bilateral CSB treatment alone. This study is limited by the small number of participants, the mechanism of this effect has not been fully elucidated. Further study is needed to determine the true promise of combined KI/CSB technique.
References
- Kessler RC, Petukhova M, Sampson NA, et Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. Int J Methods Psychiatr Res. 2012; 21: 169-184.
- Institute of Health Metrics and Evaluation. Global Health Data Exchange (GHDx). 2024.
- Summers MR, Nevin RL. Stellate Ganglion Block in the Treatment of Post-traumatic Stress Disorder: A Review of Historical and Recent Pain Pract. 2017; 17: 546-553.
- Olmsted KL, Bartoszek M, Mulvaney S, et al. Effect of Stellate Ganglion Block Treatment on Posttraumatic Stress Disorder Symptoms: A Randomized Clinical Trial. JAMA Psychiatry. 2020; 77: 130-138.
- Lipov EG, Jacobs R, Springer S, et al. Utility of Cervical Sympathetic Block in Treating Post-Traumatic Stress Disorder in Multiple Cohorts: A Retrospective Pain Physician. 2022; 25: 77-85.
- Sussman D, Tassone VK, Gholamali Nezhad F, et al. Local Injection for Treating Mood Disorders (LIFT-MOOD): A Pilot Feasibility RCT of Stellate Ganglion Block for Treatment- Resistant Chronic Stress (Thousand Oaks). 2023; 7: 24705470231160315.
- Murrough JW, Iosifescu DV, Chang LC, et Antidepressant efficacy of ketamine in treatment-resistant major depression: a two-site randomized controlled trial. Am J Psychiatry. 2013; 170: 1134-1142.
- Feder A, Parides MK, Murrough JW, et al. Efficacy of intravenous ketamine for treatment of chronic posttraumatic stress disorder: a randomized clinical JAMA Psychiatry. 2014; 71: 681-688.
- Lipov E, Sethi Z, Nandra G, et al. Efficacy of combined subanesthetic ketamine infusion and cervical sympathetic blockade as a symptomatic treatment of PTSD/TBI in a special forces patient with a 1-year follow-up: A case report. Heliyon. 2023; 9: 14891.
- Hoge CW. Interventions for war-related posttraumatic stress disorder: meeting veterans where they JAMA. 2011; 306: 549-551.
- Bovin MJ, Marx BP, Weathers FW, et al. Psychometric properties of the PTSD checklist for diagnostic and statistical manual of mental disorders–fifth edition (PCL-5) in Psychol Assess. 2016; 28: 1379-1391.
- Beck AT, Ward CH, Mendelson M, et An inventory for measuring depression. Arch Gen Psychiatry. 1961; 4: 561-571.
- Beck AT, Steer RA, Brown Psychological Corporation San Antonio TX. 1996.
- National Collaborating Centre for Mental Health (UK). Depression: The Treatment and Management of Depression in Adults (Updated Edition). Leicester (UK): British Psychological Society. 2010.
- Veith RC, Lewis N, Linares OA, et al. Sympathetic nervous system activity in major depression. Basal and desipramine- induced alterations in plasma norepinephrine kinetics. Arch Gen Psychiatry. 1994; 51: 411-422.
- Geracioti TD Jr, Baker DG, Ekhator NN, et al. CSF norepinephrine concentrations in posttraumatic stress disorder. Am J Psychiatry. 2001; 158: 1227-1230.
- Lipov EG, Joshi JR, Sanders S, et al. A unifying theory linking the prolonged efficacy of the stellate ganglion block for the treatment of chronic regional pain syndrome (CRPS), hot flashes, and posttraumatic stress disorder (PTSD). Med Hypotheses. 2009; 72: 657-661.
- Southwick SM, Krystal JH, Morgan CA, et al. Abnormal noradrenergic function in posttraumatic stress disorder. Arch Gen Psychiatry. 1993; 50: 266-274.
- Bremner Traumatic stress: effects on the brain. Dialogues Clin Neurosci. 2006; 8: 445-461.
- Hendrickson RC, Raskind MA, Millard SP, et al. Evidence for altered brain reactivity to norepinephrine in Veterans with a history of traumatic stress. Neurobiol Stress. 2018; 8: 103-