Local-Regional In-Country Differences of Ischaemic Heart Disease – Forgotten or Overlooked
Author'(s): Bhavsar R1 and Jakobsen CJ2*
1Department of Anaesthesiology and Intensive Care, South Jutland hospital, Aabenraa, Denmark.
2Heart, lung and vascular, Aarhus University Hospital, Aarhus, Denmark.
*Correspondence:
Carl-Johan Jakobsen, Heart, lung and vessel, Aarhus University Hospital, Denmark, Telephone: +45 40105200
Received: 30 Nov 2022; Accepted: 24 Dec 2022; Published: 29 Dec 2022
Citation: Bhavsar R, Jakobsen CJ. Local-Regional In-Country Differences of Ischaemic Heart Disease - Forgotten or Overlooked. Cardiol Vasc Res. 2022; 6(6): 1-5.
Abstract
Objective: The number of cardiac interventions has increased massively and improved the outcome after cardiac events. The efforts during the last decades have proven effective with a falling incidence of new cardiovascular diseases. In a relatively uniform country with free tax supported medical treatment and a fully developed ambulance and helicopter service, percutaneous cardiac intervention (PCI) after acute coronary syndrome (ACS) or overall revascularization must be a good indicator of ischaemic heart disease (IHD) and geographical differences must reflect the area frequency of IHD. Thus, so far there has not been much focus on local in country differences, which could reveal new focus for treatments.
Material and Methods: The mandatory Western Denmark Heart Registry (WDHR) was used to identify all adult cardiac procedure performed in 3 Danish regions from 2000-2020. The registry included 282,883 new patients entries of which 232,592 was grouped as IHD.
Results: Steady increase in number of investigations was observed over 15 years with stabilization of the absolute number of interventions after 2005 with subsequent decrease in treatment fraction. Data demonstrated a comparable regional activity, but significant differences in the incidence of IHD between individual municipalities.
Conclusion: The screening, investigation and intervention initiative during the last two decades has proven effective which is demonstrated by the falling incidence of new cardiovascular diseases. However, for further and faster achievements, rapidly growing use of prevention and treatment resources should be allocated to focussed areas by taking in-country differences in consideration.
Keywords
Introduction
During the last 4 decades, most countries in both developed and un-developed regions, have used a lot of efforts to temper the increasing frequency of cardiovascular diseases. The development of surgical procedures and especially the introduction of percutaneous coronary interventions (PCI) radically changed the treatment opportunities and quality. The introduction of cardiac multi-slice computed tomography (CMCT / CT-CAG) increased the screening possibilities and further, the focus of prevention added to improved results.
Following, the incidence and mortality of cardiovascular and especially ischaemic heart disease (IHD) declined profoundly in many countries during the last decades [1-3]. However, according to World Health Organization (WHO) estimates [4], IHD is still the main global cause of death, accounting for more than 9 million deaths in 2016.
It is well known that rates are different between countries and are falling in many countries, indicating a large potential for future additional gains on the global level. Further, the focus seems to be oriented towards the challenges for developing countries, which gradually acknowledge the Western lifestyle. On the horizon, future improvements may become curtailed by increasing hypertension in some developing countries and more importantly global growth in obesity. However, the overall approach of resource allocation for prevention and treatment efforts have traditionally used the helicopter perspective with the risk of overlooking local regional in-country differences. Since 1999 the Western Denmark Heart Registry (WDHR) have collected information on risk factors, diagnosis, and revascularization treatment of all cardiac procedures in 3 Danish regions, covering approximately 60% of Denmark, with a population of 3.1 million inhabitants [5-7].
Despite the general improvement, the WDHR data indicated discrete possible in-country differences and the aim of this study was to evaluate possible in-country differences in incidence and treatment of ischaemic heart disease.
Material and Methods
This study was a retrospective study based on prospectively collected data on adult patients undergoing cardiac procedures from 2000-2020 and were obtained from the mandatory Western Denmark Heart Registry (WDHR), covering approximately 60% of the Danish uptake area. The WDHR started with coronary angiography (CAG), percutaneous coronary interventions (PCI) and cardiac surgery. Transcatheter aortic valve implantation (TAVI) was added in 2007, cardiac multi-slice computed tomography (CMCT / CT-CAG) in 2008 and finally single photon emission computed tomography (SPECT) and positron emission tomography (PET) in 2016. At the end of 2020 the WDHR holds 288,300 patients with 597,754 procedures.
The municipalities in Western part are relatively small and uniform with 621 (507-722) km2 and a population of 69 (62-90) inhabitants per km2 [8]. However, regions and municipalities might be very different in inhabitant composition due to differences in ages, primarily due to educational and working possibilities. To attenuate, we calculated the results as rates based on number per 100,000 inhabitants aged 40 or older, thus minimizing differences in the age composition in regions and municipalities.
In a relatively uniform country with free tax supported medical treatment and a fully developed ambulance and helicopter service, patients with ACS are presumed to receive the same treatment regardless of residence. Following, PCI after ACS or the overall revascularization rate, must be a valuable indicator of IHD and any geographical differences must reflect the area prevalence and frequency of IHD.
The focus of the current data set was new patients submitted to PCI and coronary artery bypass grafting (CABG) divided on regions and municipalities. The study was registered by the Danish Data Protection Agency (1-16-02-587-20). The Agency's rules for the use and handling of data are met. Written consent or ethical approval is not required for registry-based studies according to Danish legislation. Frequencies (proportions / rates) are compared with chi-squared test and relationships at municipal level was assessed with ANOVA-test.
Result
The basis for the study was the WDHR at the end of 2020 the WDHR, holding 288,300 patients with 597,754 procedures. From early 00’s resources allocated to the cardiovascular area increased and investigations and interventions amplified markedly from 2000 to 2005, after which interventions have been more or less constant, while investigational procedures continued to increase. With this huge increase in investigational procedures the treatment fraction declined from 44.9% in 2003 to 20.7% in 2020 (Figure 1). The incidence of new patients with cardiac disease and more specific IHD over the period is given in figure 2. The incidence has increased up through the last decades until 2017 where it continued further with a gentle decline.
The incidence of new patients with acute coronary syndrome (ACS) and overall re-vascularization rates divided as per regions and communes is given in figure 3. In the period 2015-2019 the regions showed only discrete differences as the incidence was at a median of 185 (173-194) in South, 187 (175-196) in Mid and 204 (186-218) in North. The later marginally significantly higher than South (P=0.046, χ2-test). However, at the commune level the difference was more pronounced. The overall incidence of new patients exposed for PCI after ACS in a 5-year period varied with a difference of 48.1% in the Western part of Denmark from 148 to 215 per 100.000 inhabitants older than 40 years. Similarly, the distribution was uneven i.e. 171, 191 and 214 per 100.000 in 3 neighbouring municipalities in the northern region with a difference of more than 25.1% in relatively small area (Figure 3a).
Discussion
Through this overview of data spread over two decades of cardiovascular patients in western Denmark, multiple observations such as consistent increase in number of investigations over 15 years, stabilization of the absolute number of interventions after 2005 with simultaneous decrease in treatment fraction and increase in new IHD cases, were revealed. Furthermore, variable incidence of the disease was observed in different municipalities irrespective of population profile and location despite robust screening, investigation, and intervention efforts. As a global initiative, to control the mortality secondary to cardiac diseases, an extensive screening, investigation and intervention drive for potential
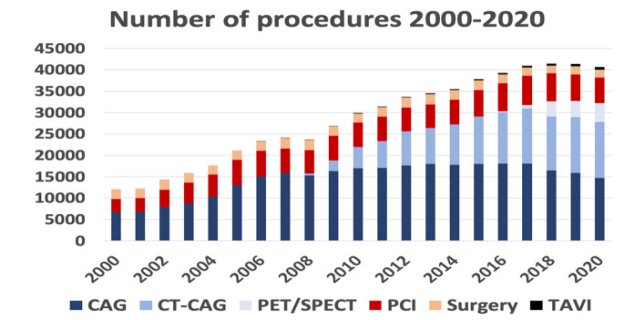
Figure 1: The number of procedures from 2000 to 2020. The fraction of treated patients (PCI, CBG and TAVI) decreased from 44.9% (2003) to 20.7% (2020) as the absolute number was almost constant.
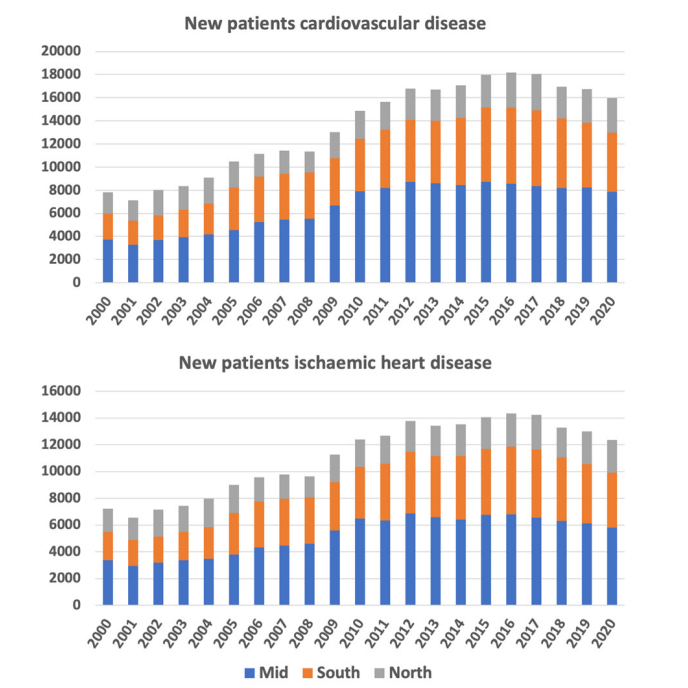
Figure 2: New patient entries in WDHR 2000-2020 of patients with cardiovascular disease (top panel) and patients with ischaemic heart diseases (lower panel) divided on regions.
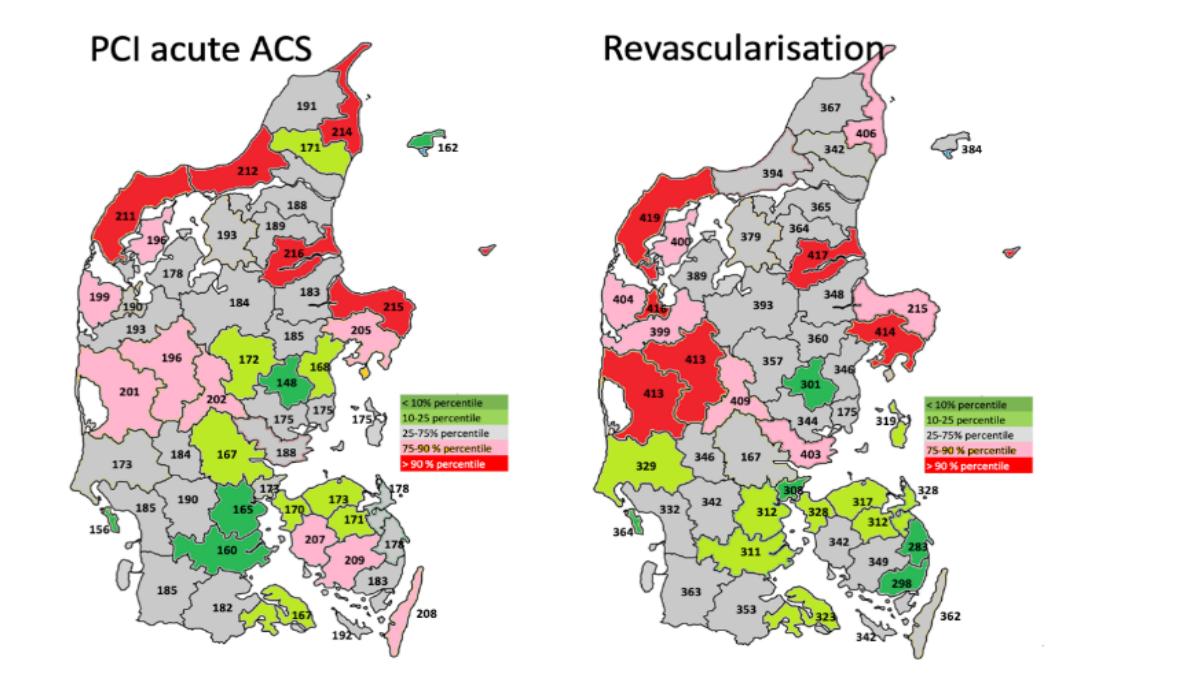
Figure 3: Patients with 1) first time PCI per 100,000 inhabitants aged ≥40 years on indication acute coronary syndrome (ACS) (left panel) and 2) first time revascularization (PCI or CABG) on all indications (right panel). in Western Danish municipalities. The colour codes refer to the 0-25, 25-50, 50-90 and 90-100 percentiles for Western Denmark. There were significant differences between individual municipalities (PCI, p<0.048, 25/90% percentiles; Revascularization, p<0.021, 25/75 percentiles).
Cardiac patients has been implemented during the last two decades in various countries including Denmark [9]. The motive clearly was to locate patients with cardiac disease and treat them before occurrence of adverse acute cardiac events. This initiative targeted both existing and potential high-risk patients.
Initial rise in number of patients in need of cardiac investigation and intervention may appear to be the reflection of cumulated undiagnosed cases over the last few years. Subsequent stabilisation of the number of interventions after 2005, may mirror the completion of the excess. Over the next few years, with the increase in the proportion of at-risk patients in the target population, in the presence of same screening criterion, number of investigations increased proportionately without increase in the proportion of actual treatment demanding IHD patients [8]. The incidence of investigations, however, is reduced slightly during 2019 to 2020 which may reflect corona pandemic related decline [10].
The observation of steady increase in new IHD cases until 2016, despite screening, investigation, and intervention efforts, may reflect several factors which include, natural time delay in the establishment of the screening, investigation, and treatment infrastructure to its fullest potential along with simultaneous rise in hypertension, diabetes and obesity in the target population [11-14]. However, since 2016, the frequency of both new overall cardiovascular and IHD patients has declined (Figure 2), reflecting that the increase in screening, investigation and intervention efforts have proven effective. It also demonstrated that increased use of resources to locate cardiovascular disease were needed. Despite this fact, it cannot be ignored that, this decline occurred after almost one and half decade of intensive efforts which triggers need of further reflection.
Further, it is to be noted that the observation of regional and intermunicipal variation in the incidence of IHD is based on the understanding that, PCI and revascularization reflect the area frequency, as ACS treatment is aimed to be uniform and in accordance with international treatment guidelines [15,16], regardless of residence in Denmark, especially when there is free tax supported medical treatment and a fully developed ambulance and helicopter service.
The observations of regional and intermunicipal variation along with prolonged delay in achieving decline in incidence of IHD may be explained on the grounds of multifactorial etiology of IHD. Similar to other developed countries, Denmark also has robust public and private sector initiatives for primary and secondary prevention of the IHD. However, as majority of the etiological factors are related to lifestyle and local culture, it is difficult to achieve sudden and uniform changes, which, therefore may take longer period and the results may show variation. Overall, one could imagine that a more proactive preventive handling based on extended indications followed by earlier PCI or CABG, could have a positive impact with lower number of new ACSs patients. However, evaluating PCI after ACS (Figure 3, left) and all re-vascularisations (Figure 3, right) does not support a clear association and in opposite, it is more likely that there are basic differences in incidence of IHD between the communes, as upper and lower quartiles is almost identical in the figures. Thus, the role of primary prevention by lifestyle and culture modification in focused areas becomes prominent and should be the area of interest in future planning of resource allocation.
Conclusion
The screening, investigation and intervention initiative during the last two decades has proven effective with the falling incidence of new cardiovascular diseases. However, for improved and faster achievements, the rapidly growing use of resources in prevention and treatment of cardiac patients and next step in prevention and treatment must be focused on in-country differences.
References
- Haunsø S, Vad OB, Amtorp O. Evident decline in mortality from ischaemic heart disease in Denmark from 1970 to Ugeskr Laeger. 2020; 182: V02200113.
- Nowbar AN, Howard JP, Finegold JA, et al. 2014 global geographic analysis of mortality from ischaemic heart disease by country, age and income: statistics from World Health Organisation and United Nations. Int J Cardiol. 2014; 174: 293-298.
- Nowbar AN, Gitto M, Howard JP, et al. Mortality from ischemic heart disease. Analysis of data from the World Health Organization and coronary artery disease risk factors from NCD Risk Factor Collaboration. Circ Cardiovasc Qual Outcomes. 2019; 12: e005375.
- Global Health Estimates 2016: Deaths by Cause, Age, Sex, by Country and by Region, 2000- Geneva, Switzerland: World Health Organization. 2018.
- Rasmussen LA, Bøtker HE, Jensen LO, et Quality assurance of the Western Denmark Heart Registry, a population-based healthcare register. Dan Med J. 2017; 64: A5414.
- Thuesen L, Jensen LO, Tilsted HH, et Event detection using population-based health care databases in randomized clinical trials: a novel research tool in interventional cardiology. Clin Epidemiol. 2013; 5: 357-361.
- Schmidt M, Maeng M, Madsen M, et The Western Denmark Heart Registry: Its Influence on Cardiovascular Patient Care. J Am Coll Cardiol. 2018; 71: 1259-1272.
- https://www.dst.dk/en/Statistik/emner/borgere/befolkning/befolkningstal
- Chris Kypridemos, Kirk Allen, Graeme L Hickey, et al. Cardiovascular screening to reduce the burden from cardiovascular disease: microsimulation study to quantify policy options. BMJ. 2016; 353: i2793.
- Christensen DM, Butt JH, Fosbøl E, et al. Nationwide cardiovascular disease admission rates during a second COVID-19 lockdown. Am Heart J. 2021; 241: 357.
- Kronborg CN, Hallas J, Jacobsen IA. Prevalence, awareness, and control of arterial hypertension in Denmark. J Am Soc Hypertens. 2009; 3: 19-24.
- Hoffmann-Petersen N, Lauritzen T, Bech JN, et al. High Prevalence of hypertension in a Danish population telemedical home measurement of blood pressure in citizens aged 55-64 years in Holstebro Am J Hypertens. 2016; 29: 439-447.
- Carstensen B, Rønn PF, Jørgensen ME. Components of diabetes prevalence in Denmark 1996-2016 and future trends until 2030. BMJ Open Diabetes Res Care. 2020; 8: e001064.
- https://www.sst.dk/-/media/Udgivelser/2003/Publ2003/National_Action_Plan,-d-,pdf.ashx.
- Collet JP, Thiele H, Barbato E, et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment Eur Heart
- 2021; 42: 1289-1367.
- Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018; 39: 119-177.