Lumbar Dorsal Root Ganglion Pulsed Radiofrequency for Spinal Stenosis with an Atypical Fluoroscopic Neurogram: A Case Study
Author'(s): Ahilraj Siva1,2*, Marc Price-Morris2 and Shayan Khimji3
1Staff, Hamilton Health Sciences, Michael G. DeGroote Pain Centre,Assistant Clinical Professor, Division of Physical Medicine and Rehabilitation, Department of Medicine, McMaster University,Canada.
2Afiya Spine and Pain Institute, Canada.
3University College Dublin School of Medicine, Ireland
*Correspondence:
Dr. Ahilraj Siva MD, Department of Medicine, McMaster University, 1280 Main Street West, Hamilton, Ontario, Canada,Tel: 905-521-2100.
Received: 01 Oct 2023; Accepted: 09 Nov 2023; Published: 15 Nov 2023
Citation: Ahilraj Siva, Marc Price-Morris, Shayan Khimji. Lumbar Dorsal Root Ganglion Pulsed Radiofrequency for Spinal Stenosis with an Atypical Fluoroscopic Neurogram: A Case Study. Anesth Pain Res. 2023; 7(2): 1-3.
Abstract
Background: We present a case of an atypical fluoroscopic neurogram pattern for complex chronic axial low back pain during a lumbar dorsal root ganglia (DRG) pulsed radiofrequency stimulation.
Case Report: A 70 year old female with a history of complex chronic axial low back pain with radicular leg pain. Initially her pain was described as intermittent, burning, and sharp with an intensity of 9/10 on the Numeric Rating Scale (NRS). This pain worsens with ambulation, lumbar extension, turning, weight bearing and spinal loading activities. MRI imaging noted lumbar anterolisthesis, moderate to severe central spinal stenosis, and mild bilateral neural foraminal space narrowing. From these findings, her pain is likely secondary to components of sacroiliac (SI) joint dysfunction, lumbar facetogenic pain, lumbar radiculitis, and spinal stenosis with neurogenic claudication. A multimodal and multidisciplinary rehabilitation approach involving minimally invasive interventional procedures and medication management was implemented with varying pain relief. She responded to L5 transforaminal epidural nerve root injections, SI joint prolotherapy, and sacral lateral branch radiofrequency ablation. She completed bilateral L5 DRG pulsed radiofrequency stimulation, which did not provide radicular pain relief. We performed a unilateral L4 DRG pulsed radiofrequency stimulation, which revealed an atypical L4 fluoroscopic neurogram pattern. At the 3 month follow up she reported the pain severity to have a NRS between 7-8/10. At 4 months, the pain severity was reported to have a NRS between 4-6/10 with subjective improvements with her daily activities.
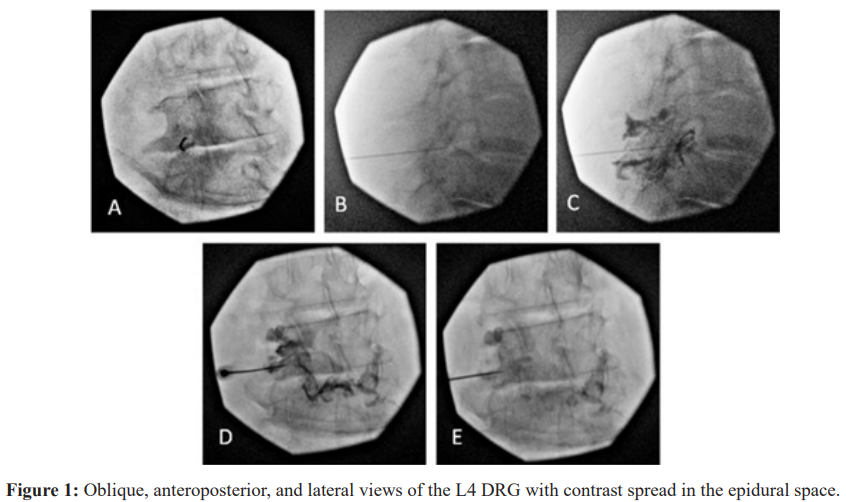
Conclusion: In a normal transforaminal epidural fluoroscopic neurogram, the anteroposterior view should demonstrate contrast spread medially around the pedicle and laterally following the exiting nerve root. In the case of this patient the combined anatomical presentation of anterolisthesis, central spinal canal stenosis, and circumferential disc bulging are all potential reasons for insufficient contrast passage resulting in the atypical neurogram.
Keywords
Introduction
Approximately 5% of all adults will experience radicular lumbar pain during their lifetime [1]. Symptoms of lumbar radiculopathy can vary depending on the location and severity of the nerve compression, but commonly includes localized pain, paresthesia,lower limb radiating pain, and numbness. Other symptoms may include muscle weakness, reduced mobility, impaired spinal reflexes, decreased function and activity tolerances. The most common causes for developing lumbar radiculopathy are degenerative spondyloarthropathies, spondylolisthesis, disc bulging, and disc herniation [1]. Management for lumbar radiculopathy initially involves conservative treatment strategies such as back care education, physical therapy, and oral nonsteroidal anti-inflammatory drugs (NSAIDs)
Symptoms that are resistant to conservative therapies require further investigation and minimally invasive interventions such as epidural corticosteroid injection, facet medial branch blocks, and facet joint injections [2]. Ongoing research continues to highlight pulsed radiofrequency stimulation as an innovative and novel treatment modality for pain management, especially lumbar radiculopathy [3]. To optimize management strategies and improve therapy outcomes, research studies investigate combined conservative treatments with minimally invasive interventions. Some studies have shown that pulsed radiofrequency stimulation combined with transforaminal epidural corticosteroid injections can improve pain severity reporting at 3 months post-procedure for chronic lumbosacral radicular pain [3].
We present a case study to highlight the treatment efficacy of unilateral pulsed radiofrequency stimulation of the L4 DRG combined with a nerve root block for lumbar radiculopathy with an atypical neurogram.
Case Presentation
History
A 70 year old female was referred with a 10 year history of intermittent pain described as burning and sharp that worsens with ambulation, twisting, and spinal loading activities. She initially rated her pain intensity as 9/10 on the Numeric Rating Scale (NRS). Pertinent positive physical examination findings were lumbar facet loading, sacroiliac (SI) joint provocation, and straight leg raise neural tension maneuvers. MRI imaging results noted anterolisthesis of L4 vertebrae on L5 measuring 5mm, mild bilateral L5/S1 neural foramen space narrowing, and moderate to severe central spinal stenosis at L4/5 secondary to circumferential L4 and L5 disc bulging, mild facet and moderate ligamentous hypertrophy. From these findings, her pain is likely secondary to components of SI joint dysfunction, lumbar facetogenic pain, lumbar radiculitis, and spinal stenosis with neurogenic claudication.
Preliminary interventions targeted the pain component associated with SI joint dysfunction by performing bilateral SI joint lateral branch denervation with radiofrequency thermal ablation combined with intra-articular SI joint dextrose prolotherapy injection. She reported moderate pain reduction for approximately 3 months, with persistent lumbar radicular symptoms. She responded to diagnostic L5 transforaminal epidural nerve injection and selective nerve root block, and underwent bilateral L5 DRG pulsed radiofrequency stimulation which provided radicular pain reduction for approximately 8 weeks with a reported 5/10 on the NRS. At 3 months follow up, she reported improvements with her function and ability to perform activities. However, her lumbar radicular symptoms were more pronounced on the left side compared to the right. Subsequently, she underwent a left L4 DRG pulsed radiofrequency stimulation with selective nerve root block. Prior to the procedure she reported the pain severity to be between 7-8/10 on the NRS. At 4 months post-procedure, the pain severity was reported to have a NRS between 4-6/10 with subjective improvements with her daily activities.
Description of the Procedure
Using intermittent fluoroscopy in the anteroposterior (AP) position, needle entry point was landmarked and anesthetized locally with 1cc of 1% lidocaine subcutaneously. Continuing with intermittent fluoroscopy guidance in oblique views, the 20 gauge 10 cm radiofrequency cannula with a 10 mm curved active tip was directed to the left L4 mid-pedicular line (Figure 1A). In the lateral view, the cannula was positioned to be in the intervertebral foramen (Figure 1B). The radiofrequency generator was adjusted to 0.6V of sensory stimulation. Next, 3cc of 300 omnipaque contrast was injected for visual epidural space confirmation in a lateral (Figure 1C) and AP (Figure 1D) positions. Then 1cc of 0.125% bupivacaine was injected, with contrast washout seen in AP view (Figure 1E). Next, the pulsed radiofrequency stimulation was performed for 10 minutes with the parameters set to 42°C, 45V, 10ms pulse width, and 10Hz.
Discussion
This case is a unique example of an atypical contrast pattern for a nerve root block. Typically, a L4 transforaminal epidural injection should have the injectate spread medially around the pedicle and laterally with the exiting nerve root. As shown in Figure 1, there is insufficient passage of injectate through the target nerve root. Insufficient passage of injectate is believed to be as a result of the anatomical changes and characteristics rather than a procedural error.
Currently, there is limited literature on the potential causes of radiographical anomalies during selective nerve root blocks. However, Yeom et al. performed a prospective, controlled and blinded study to determine the accuracy of diagnostic lumbar selective nerve root blocks as well as analyze potential causes of false results. This study found that the identifiable false-negative results on radiographs included insufficient infiltration and passage of the injectate, and intraepineural injections. False-positive results were due to injectate overflow from the injected asymptomatic level into the epidural space or the symptomatic level. Inadequate blocks were attributed to 10 out of the 20 false-negative cases, and classified into 3 types: insufficient infiltration, insufficient passage, and intraepineural injection. Insufficient infiltration refers to the injectate leaking into the surrounding tissues instead of the target location. Insufficient passage resulted from the herniated disc blockade preventing spread due to nerve root compression. Intraepineural injection occurred when the injectate temporarily aggravated the radiating pain instead of alleviating it. There were 4 out of 8 false-positive cases that were attributed to lidocaine overflow from the control level into the epidural space or into the symptomatic level. The other 4 false positives were not identifiable on the spot radiographs [4].
In this case, the MRI presented evidence of anterolisthesis involving the L4 and L5 vertebrae, bilateral L5 neural foramen space narrowing, moderate to severe central spinal canal stenosis at L4/5, and circumferential disc bulging at L4 and L5. The combination of these anatomical changes are potential causes for insufficient passage and atypical spread of contrast. As noted by Yeom et al., this case would be an example of insufficient passage false-negative radiographical anomaly. For this case, additional follow-up would be imperative to assess the response to the interventions, as well as additional imaging studies to track the anatomical changes.
This case highlights the anatomical characteristics that can be present in complex chronic lumbar radiculopathy patients. As evident by the contrast spread pattern in Figure 1, injectable interventions such as corticosteroids may not localize to the targeted nerve root. With the implementation of minimally invasive pulsed radiofrequency stimulation interventions, the targeted nerve root can be accurately localized. Also, further developments and techniques should continue to be explored for optimal management of patients with complex chronic lumbar radiculopathy. In addition, for future investigations further evaluation of the pulsed radiofrequency stimulation outcome measures should have in conjunction with the Numeric Pain Rating Scale, the Roland Morris (lumbar spine) and Neck Pain and Disability Index (cervical spine) which are standardized tests with reliability and validity.
References
- Dydyk A, Khan MZ, Singh Radicular Back Pain. Stat Pearls Treasure Island. 2023.
- Berry JA, Elia C, Saini HS, et A Review of Lumbar Radiculopathy Diagnosis and Treatment. Cureus. 2019; 11: 5934.
- Çaliskan DK, Akesen S, Türker YG, et The effect of combined pulsed radiofrequency treatment to dorsal root ganglion with transforaminal epidural steroid injection on pain. Agrı. 2021; 33: 223-231.
- Yeom JS, Lee JW, Park KW, et Value of Diagnostic Lumbar Selective Nerve Root Block: A Prospective Controlled Study. AJNR Am J Neuroradiol. 2008; 29: 1017-1023.