Optical Coherence Tomography Analysis of Des In-Stent Restenosis Presenting As Stable and Unstable Angina: A Comparison - A Case Series
Author'(s): Mody Rohit1*, Dash Debabrata2, Mody Bhavya3, Saholi Aditya4 and Khullar Akshit5
1Department of Cardiology, MAX Super specialty hospital, Bathinda, Punjab, India, ORCID - https://orcid.org/0000-0001-8977-5803.
2Department of Cardiology, Aster Hospital, Dubai, Al Quasis, UAE, ORCID - https://orcid.org/0000-0003-1354-3808.
3Department of Medicine, Kasturba medical college, Manipal, Karnataka, India, ORCID - https://orcid.org/0000-0001-8944-9418.
4Department of Cardiology, Adesh Institute of medical sciences and Research, Bathinda, Punjab, India, ORCID - https://orcid.org/0000-0001-7545-5833.
5Department of Medicine, Adesh Institute of Medical sciences and Research, Bathinda, Punjab, India, ORCID - https://orcid.org/0000-0001-8461-1770.
*Correspondence:
Dr. Rohit Mody, Department of Cardiology, MAX Super specialty hospital, H.no- 438, Model Town phase 2, Bathinda, Punjab, India. Pin-151001, Tel: +91-9888925988.
Received: 25 February 2021; Accepted: 19 April 2021
Citation: Rohit M, Debabrata D, Bhavya M, et al. Optical Coherence Tomography Analysis of Des In-Stent Restenosis Presenting As Stable and Unstable Angina: A Comparison – A Case Series. Cardiol Vasc Res. 2021; 5(2): 1-4.
Abstract
Rationale: Drug-eluting stents (DES) have been demonstrated to successfully reduce the rate of instant restenosis and Target Vessel Revascularization (TLR) at least during short term follow up, and instant restenosis (ISR) is generally considered to be a stable process. However, recent studies have reported 1/3rd of patients with ISR present with Acute coronary syndrome (ACS).
Objective: We report in this case series, two patients, one presenting with stable angina and another presenting with unstable angina. We compared Optical Coherence Tomography (OCT) analysis of these two subsets of patients.
Findings: In case of stable angina patients the Optical Coherence Tomography (OCT) findings suggested homogenous character of restenotic plaque with high back scatter in majority of tissue, regular lumen shape, no micro vessels, no intraluminal material. There was nothing suggestive of intimal rupture, no Thin Cap Fibrous Atheroma (TCFA) containing neo intima.
In case of unstable angina patients, OCT characterization further reveals both homogenous layered and heterogeneous characteristic of restenotic plaque with mixed high and low backscatter along with irregular lumen shape in between. Presence of micro vessels was also noted, and areas of lipid core were noted. There are areas of intimal rupture, TCFAs and presence of macrophages.
Conclusion: In patients of DES instant restenosis, the presentation as stable or unstable patient can be analysed by OCT characterization of the resultant plaque.
Keywords
Case Presentations
Case 1
59 years old female, a case of post percutaneous traluminal coronary angiography (PTCA) to left anterior descending artery (LAD) done with second generation DES (Cobalt-chromium everolimus eluting stent; Expedition; Abbott Vascular, Santa Clara, California) previously done one year back. Patient is a known case of hypertension, diabetes, severe left ventricular (LV) dysfunction (Ejection Fraction (EF) - 20%), came with stable angina on exertion since one month (class 3).
Coronary angiography was done which revealed long diffuse restenosis starting from native proximal LAD and involving the stent. Pre PTCA-OCT run was taken which revealed that the diameter of previously deployed stent was from 1.9mm to 2mm in proximal part. The possible cause of ISR was under expansion in mid part and landing in proximal diseased segment. The OCT findings (Figure 1B) revealed homogenous character of restenotic plaque with high back scatter in majority of tissue, regular lumen shape, no micro vessels, no intraluminal material. There was no intimal rupture, no thin Cap Fibrous Atheroma (TCFA) containing neo intima. The lesion was crossed with Balance Middle Weight (BMW) wire. Then distal DES (Promus Element Everolimus Eluting Coronary Stent, Boston Scientific, Massachusetts, USA) 3*36mm deployed at 10 atm. Post dilatation done with 3*15 mm NC voyager balloon at 18 atm. Then a proximal DES (Promus Element Everolimus Eluting Coronary Stent, Boston Scientific, Massachusetts, USA) 3.5*23mm was deployed from proximal to mid dilated and procedure completed with post dilatation with 3.5*15 mm NC voyager balloon at 20 atm. (Figure 1A)
Case 2
On the other hand, second case presented to us with rest angina since 15 days, diagnosed as unstable angina. He was a post PTCA patient, LAD PTCA was done 3 years back with onyx DES (Resolute onyx Zatarolimus-Eluting coronary stent, Medtronic, Dublin, Ireland) resolute 3 years back. Patient is a known case of hypertension, non-diabetic, LV dysfunction (EF 35%). Coronary Angiography (CAG) revealed tight diffuse instent restenosis of LAD. Pre PTCA OCT was done. OCT run revealed (Figure 2B) diameter of proximal and distal stent was between 3-3.5mm, which was adequately expanded. The OCT characterization further reveals both homogenous layered and heterogeneous characteristic of restenotic plaque with mixed high and low backscatter. There was irregular lumen shape in between. Presence of micro vessels was also noted, and areas of lipid core were noted. There are areas of intimal rupture, TCFAs and presence of macrophages.
The procedure was completed with predilatation followed by two DES (Cobalt-chromium everolimus eluting stent; Expedition; Abbott Vascular, Santa Clara, California) and (Promus Element Everolimus Eluting Coronary Stent, Boston Scientific, Massachusetts, USA) .One in proximal to mid LAD, another from LAD to left main. After stent deployment post dilatation in left main with 5*8mm NC balloon (Mozec NC; Meril) at 24 atm was done to complete the procedure. (Figure 2A).

Figure 1a: CAG shows instent restenosis of LAD.
Figure 1b: ISR – Homogenous/Layered- Fibrotic with lipidic spurts.
Previous Stent dimensions: Diameter: distal- 2.40mm, MID-2.00mm, Tight point – 1.90mm, proximal edge- 2.40mm. Probable cause of ISR; Stent Under expansion in mid part. Landing in proximal disease segment.
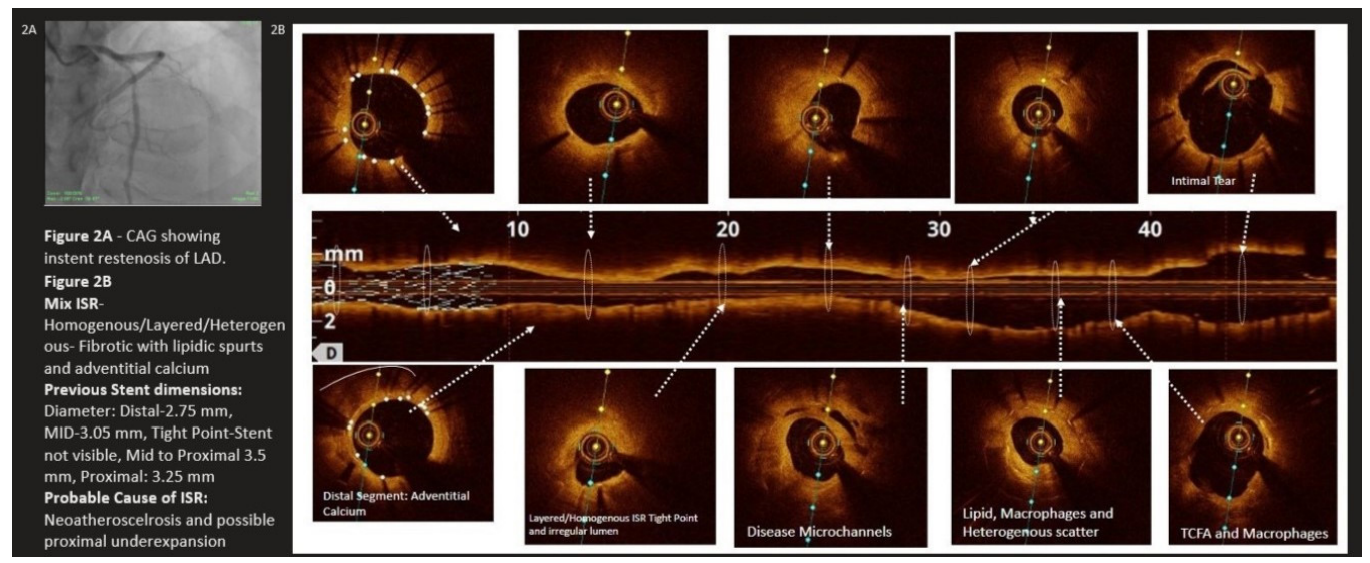
Figure 2a: CAG showing instent restenosis of LAD.
Figure 2b: Mix ISR – Homogenous/Layered/heterogeneous- fibrotic with lipidic spurts and adventitial calcium.
Previous Stent dimensions: Diameter; distal- 2.75mm, MID- 3.05mm, Tight Point- Stent not visible, Mid to Proximal 3.5mm, Proximal: 3.25mm. Probable cause of ISR: Neoatherosclerosis and possible proximal under expansion.
Discussion
1/3rd of patients with instent restenosis present with acute coronary syndromes [1,2]. Furthermore, there is emerging histological and angioscopic evidence of late de novo instent new atherosclerosis [3-7]. Recently Takano et al suggested that TCFA neointimal disruption and thrombus are detected by OCT were more frequently found late , greater than 5 years in comparison with earlier less than 6 months. In our patients also, the second case presented with unstable angina had stent implanted 3 years back with OCT features of neoatherosclerosis. The higher incidence of instent TCFA containing neo intima macrophages, neo intimal rupture in unstable angina patient supported the concept that these OCT findings were similar to vulnerable plaque in the native coronary artery [8,9]. In our case, we do not have histopathological correlation but we can hypothesize that the patients who present as unstable angina have heterogeneous character of restenotic plaque as it correlates with aging plaque. Also characters like irregular lumen shape, micro vessels, TCFAs and areas of intimal rupture with presence of macrophages are more frequent in patients who present with unstable angina.
Conclusion
The present case report identifies the ability of the OCT to identify differential patterns of restenotic tissue after stenting. It also generated a hypothesis that with time instent neo atherosclerosis produces unstable characteristics into the plaque and that can be possible cause of late stent thrombosis seen in DES patients. This hypothesis needs to be confirmed in larger studies comparing unstable with stable patients.
References
- Fineschi M, Gori T, Pierli C, et al. Outcome of percutaneous hybrid coronary revascularization: Bare metal stents jeopardize the benefit of sirolimus-eluting stents in the real world. Can J Cardiol. 2005; 21: 1281-1285.
- Chen MS, John JM, Chew DP, et al. Bare metal stent restenosis is not a benign clinical entity. Am Heart J. 2006; 151: 1260-1264.
- Kimura T, Abe K, Shizuta S, et al. Long-term clinical and angiographic follow-up after coronary stent placement in native coronary arteries. Circulation. 2002; 105: 2986-2991.
- Appleby CE, Bui S, Dzavík V. A calcified neointima: “stent” within a stent. J Invasive Cardiol. 2009; 21: 141-143.
- Habara M, Terashima M, Suzuki T. Detection of atherosclerotic pro- gression with rupture of degenerated in-stent intima five years after bare-metal stent implantation using optical coherence tomography. J Invasive Cardiol. 2009; 21: 552-553.
- Hasegawa K, Tamai H, Kyo E, et al. Histopathological findings of new in-stent lesions developed beyond five years. Catheter Cardiovasc Interv. 2006; 68: 554-558.
- Higo T, Ueda Y, Oyabu J, et al. Atherosclerotic and thrombogenic neointima formed over sirolimus drug-eluting stent: an angioscopic study. JACC Cardiovasc Imaging. 2009; 2: 616-624.
- Takano M, Yamamoto M, Inami S, et al. Appearance of lipid- laden intima and neovascularization after implantation of bare-metal stents extended late-phase observation by intracoronary optical coherence tomography. J Am Coll Cardiol. 2009; 55: 26-32.
- Soo-Jin Kang, Gary S Mintz, Takashi Akasaka, et al. Optical coherence tomographic analysis of in-stent neoatherosclerosis after drug-eluting stent implantation. Circulation. 2011; 123: 2954-2963.