Pathogenetic Mechanisms of Development of Peripheral Angiopathy (Diabetic Foot) and Development of a Method of Complex Treatment with a Metabolically Corrective Drug
Author'(s): Dzugkoev SG, Mozhaeva IV, Margieva OI, Dzugkoeva FS
Institute of Biomedical Research - Branch of the Federal Scientific Center "Vladikavkaz Scientific Center of the Russian Academy of Sciences", Russia.
*Correspondence:
Dzugkoeva FS, Institute of Biomedical Research - Branch of the Federal Scientific Center "Vladikavkaz Scientific Center of the Russian Academy of Sciences", Russia, Republic of North Ossetia-Alania, 362911, Tel: 8-901-497-20-14, E-mail: patbiochem@mail.ru.
Received: 25 June 2017 Accepted: 21 July 2017
Citation: Dzugkoev SG, Mozhaeva IV, Margieva OI, et al. Pathogenetic Mechanisms of Development of Peripheral Angiopathy (Diabetic Foot) and Development of a Method of Complex Treatment with a Metabolically Corrective Drug. Diabetes Complications. 2017 1(2); 1-4.
Abstract
In order to study the pathogenetic mechanisms of vascular complications (peripheral angiopathy), 39 patients with type 1 diabetes mellitus were diagnosed with the phenomena of the beginning diabetic foot and changes in metabolism of different degrees of compensation: decompensated, subcompensated and compensated, and also on 20 healthy individuals. All patients received basic therapy with insulin preparations of short and intermediate action, and some patients with a subcompensated form received coenzyme Q10 simultaneously with hypoglycemic therapy. The parameters of lipid peroxidation and antioxidant system, concentration of total metabolites of nitric oxide, low density lipoproteins, activity of organo-specific enzymes: alanine aminotransferase, aspartate aminotransferase, gamma-glutamyl transpeptidase were determined. The change in blood flow in the vessels of the lower extremities (shin and foot segments) was judged by the rheovasogram determined by the "Valenta" diagnostic system. The obtained data testified to the presence of oxidative stress in patients with diabetes mellitus decompensated with subcompensated forms. At the same time, the concentration of nitric oxide and its bioavailability decreased due to an increase in the blood of atherogenic lipoproteins: low-density cholesterol and high-density cholesterol. These biochemical changes in the blood were accompanied by a violation of hemodynamics in the vessels of the shin and foot. Against the background of traditional treatment, there were positive changes in carbohydrate and lipid metabolism, but the indicators were significantly different from the control level, and hemodynamic changes in the segments of the shin and foot were preserved. Inclusion of coenzyme Q10 in the complex treatment of antioxidant led to a decrease in malonic dialdehyde content, an increase in the activity of antioxidant defense enzymes, and a concentration of total metabolites of nitric oxide. Bioavailability of nitric oxide also increased, due to a decrease in the concentration of low-density atherogenic lipoproteins. In the vessels of microcirculation, the tone of arterioles and precapillaries decreased, the modulus of elasticity increased, pulse blood filling increased in the segments of the shin and foot, and venous congestion decreased.
Keywords
Introduction
The problem of diabetes mellitus and its vascular complications is topical, as the incidence increases and every 10-15 years - doubles [1-4]. At present, there are more than 300 million people with diabetes mellitus in the world, which is 6.6%. In the genesis of vascular complications of type 1 diabetes mellitus, endothelial dysfunction plays a pathogenetic role, which leads to systemic hemodynamic disorders, including microangiopathies: nephropathy, retinopathy, diabetic foot, etc. Its role in the development of vascular complications is caused by activation of lipid peroxidation, disturbance of the metabolism of nitric oxide and non-enzymatic glycosylation of proteins [5-12]. Endothelial dysfunction develops, the ability of endothelial cells to synthesize nitric oxide - the most important vasodilator [13,14]. On the other hand, the development of effective comprehensive methods for treating type 1 diabetes mellitus with peripheral angiopathies is topical and these questions are not enough in the literature.
The purpose of this study was to study the mechanisms of endothelial dysfunction in patients with type 1 diabetes mellitus of varying degrees of compensation and the effectiveness of complex therapy with coenzyme Q10.
Material and Methods
The investigations were carried out on the basis of the Republican Endocrinology Dispensary of the Republic of North Ossetia- Alania and the Department of Pathobiochemistry of IBMI VSC RAS. The analysis was carried out in 39 patients with type 1 diabetes with duration of disease on average 1-35 years (aged 18 to 40 years) with the phenomena of peripheral diabetic angiopathy and metabolic disorders of various degrees of compensation before, after basic and complex therapy and 20 healthy persons without sugar Diabetes, constituting the control group. Among the surveyed: men - 26, women - 13 patients with type 1 diabetes mellitus. Assessment of the severity and phase of compensation for type 1 diabetes mellitus was carried out according to clinical and laboratory criteria recommended by the endocrinology research center of the Russian Academy of Medical Sciences [15].
Patients were divided into 3 groups depending on the compensation of metabolism:
- Decompensated patients - before treatment (n = 12 people).
- Patients with a subcompensated form of diabetes mellitus, who received basic therapy with insulin preparations - short- acting (actrapid) and intermediate action (protopid, monotard, actress, humulin) (n = 15 people).
- Patients with a subcompensated form of diabetes mellitus who received complex treatment: insulin preparations + coenzyme Q10 2 capsules 0.5 g each. (Evalar ZAO) per day with meals (n = 12).
Blood sampling for analysis was performed in the morning on an empty stomach from the ulnar vein. Serum was obtained by centrifugation at 4°C for 15 minutes at 2500 rpm. Glucoso E-D (Vitale Diagnostics SPB), glycated Hb (HbAlc) colorimetry method (Lachema kit), lipid peroxidation concentration by malonic dialdehyde concentration (Asacawa T method) was determined in blood by glucose oxidase method. [16], catalase activity by the method of Korolyuk MA [17] and superoxide dismutase - the autooxidation of epinephrine [18], the concentration of total metabolites of nitric oxide [19], the activity of transaminases, the content of total cholesterol ("Fluitest Chol", "Cholesterin Chool- Papu", "Fluitest HOL-D Direct HOL-Cholesterol" Respectively, the company "BIOKON".
The indices of diabetic angiopathy were changes in hemodynamics in the segments of the shin and foot, determined using the diagnostic system "Valenta". According to the rheovasogram, the following indices were determined:
- Rheographic index; B / p.
- Modulus of elasticity; %.
- Time of maximum systolic filling; Sec
- Diastolic index.
- Venous outflow; %.
Statistical processing was carried out using the Microsoft Excel program. The results are presented as the mean (Mean) and the mean error (Sem). The reliability of the differences between these patients with type 1 diabetes and the control group was checked using Student's t-test, the level of statistical significance was considered to be p <0.05.
Results and Discussion
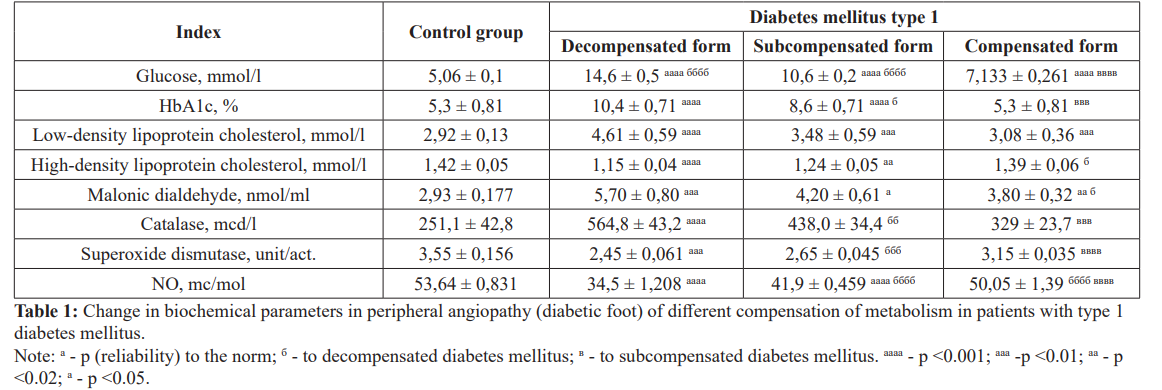
The data presented in Table. 1 indicate that in patients with type 1 diabetes mellitus with decompensated and subcompensated forms, there is a statistically significant increase in blood glucose and glycated hemoglobin content, respectively, to 10.4 ± 0.71% and 8.6 ± 0.71% (p < 0.001), in comparison with the control (HALAC, 5.3 ± 0.81%). Metabolic disorders, including glycated hemoglobin, lead to activation of lipid peroxidation in patients in a state of decompensation, which is accompanied by the accumulation of malonic dialdehyde in the blood. The antioxidant system is disrupted - the activity of superoxide dismutase decreases with decompensated and subcompensated forms of type 1 diabetes mellitus, and catalase activity rises. Oxidative stress develops, against which there is a decrease in the content of total metabolites of nitric oxide in the blood serum. The intensification of the processes of free radical oxidation contributes to the disruption of the activity of eNOS (NOS III), through the effect on the cofactors: Tetrahydrobiopterin and Nicotinamide adenine dinucleotide phosphate +.
The radical (O2-) formed in this superoxideidion reacts with NO, producing peroxynitrite, which has a damaging effect on the vascular endothelium. Reducing the bioavailability of NO contributes to the violation of cholesterol metabolism and atherogenesis. In patients with type 1 diabetes mellitus, the content of total cholesterol, triacylglycerides, low-density cholesterol and high-density cholesterol decrease. These data indicate the prevalence of atherogenic lipoproteins in the blood, also contributing to the development of endothelial dysfunction and a decrease in the bioavailability of NO, which is consistent with the literature data [20-22]. All these patients had cardiopathy, arterial hypertension, a decrease in the concentration of total metabolites of NO and peripheral angiopathy of the lower extremities (Table 1).
Analysis of data characterizing hemodynamic changes in the lower extremities showed that in patients with decompensated and subcompensated forms of type 1 diabetes mellitus, the pulse blood filling of the shank segments (left and right) and the foot (left and right) decreased, as a result of vascular elasticity, Arterial network of the lower leg and foot, as well as arterioles and precapillaries. In the process of statistical processing of rheovasogram indices in 51,3-70,3% of patients with decompensated and subcompensated forms of type 1 diabetes mellitus, the rheographic index (by 122% and 127%), the elastic modulus (by 132% and 143%), respectively, characterizing the state of the vascular wall of microcirculatory vessels and the nature of hemodynamics. These changes in the condition of the arterial network were accompanied by venous congestion by 374.6% and the indicator subject to outflow through the venous system increased in 37.8-45.9% of patients, while in the other part of the patients it did not differ significantly from the level of normative indices. The maximum systolic filling rate was increased by 126.4% in 62.29-72.97% of patients; the diastolic index was increased by 196% in 70.3-86.5%. Comparing the nature of changes in the hemodynamics of the left segments of the shin, the foot with the right, asymmetry is often noted. Infringement of microcirculation of the lower extremities (shin, foot) is accompanied by hyperperfusion in the main arterial vessels and an increase in the value of arterial blood pressure by 131%.
Along with this, in patients with type 1 diabetes mellitus with cardiopathic disorders and angiopathies as a result of activation of lipid peroxidation, there is a violation of the permeability of cardiomyocyte cell membranes and an increase in the activity of transaminases: alanine aminotransferase (by 236.3%), aspartate aminotransferase (by 125%) And the membrane enzyme gamma- glutamyl transpeptidase 7-fold.
Chain reactions involving free radicals are the cause of endothelial dysfunction, accompanied by organ-systemic disorders in type 1 diabetes mellitus, which served as the basis for the use of complex antioxidant treatment with coenzyme Q10 [23]. This drug was taken by patients 2 capsules 1 time per day during meals for 14-20 days along with traditional therapy, including insulin preparations. All general clinical, biochemical and functional studies were performed 14-20 days after the beginning of the course of therapy,i.e. at an extract from a hospital. In contrast to the data obtained against the background of traditional therapy, complex treatment in combination with the antioxidant coenzyme Q10 showed a more statistically significant decrease in the final product of lipid peroxidation - malonic dialdehyde in the blood, the values of which remained statistically significantly elevated in patients with a subcompensated form of diabetes mellitus, Who received therapy with insulin preparations. The activity of superoxide dismutase increased against the background of complex therapy and almost reached the control level after 14-20 days of complex treatment, whereas the catalase activity decreased, but remained elevated compared to the control group. The concentration of total metabolites of NO - the main vasodilating factor was increased.
Thus, after the course of treatment, complex therapy led to a significant positive shift in the lipid peroxidation system- antioxidant protection, there was a significant increase in superoxide dismutase activity and a decrease in catalase activity, i.e. an imbalance was eliminated in this system. Reduction of oxidation-reduction processes led to an increase in the nitroxide- forming function of the endothelium: vessels and an increase in the serum concentration of total NO metabolites. Positive dynamics of metabolic and functional indices was detected in some patients with a subcompensated form of type 1 diabetes mellitus receiving complex therapy: hypoglycemic drugs and coenzyme Q10. Against the background of complex treatment, peripheral hemodynamics normalized, due to the restoration of the elasticity of the microcirculation vessels, a decrease in the tone of arterioles and precapillaries, or an insignificant increase in the segments of the shin. These changes are indicated by a decrease in the rheographic index and the modulus of elasticity of the wall of arterioles and precapillaries. The tone of the venous network either fully recovered or the hypotension was negligible, in accordance with which the volume of venous outflow decreased. In the segments of the foot against the background of a hypoglycemic and metabolic correcting drug, there is also an improvement in pulse blood filling, due to a decrease in vascular tone, since the modulus of elasticity decreases. There is a decrease in the volume of venous outflow due to an increase in the tone of the venous network.
Conclusion
Thus, coenzyme Q10, regulating the function of the respiratory chain, inhibits the formation of free radicals, promotes the complete restoration of oxygen to the water molecule and energy formation. The effectiveness of the action of coenzyme Q10 was confirmed by correlation analysis, a direct correlation was found between malonial dialdehyde and catalase activity (r = + 0.57), negative correlation (r = -0.46) between the reduction level of malonic dialdehyde concentration and the increase of superoxide dismutase activity, the relationship between the concentration of NO and malonic dialdehyde (r = -0.51). Considering the dynamics of metabolic indicators against the background of complex treatment, more significant changes in the level of glycated hemoglobin, total cholesterol, and low and high density lipoprotein cholesterol were noted.
These biochemical changes were accompanied by restoration of the elasticity of the vessels of microcirculation, a decrease in the tone of arterioles and precapillaries, a modulus of elasticity and an increase in pulse blood filling in the segments of the shin and foot, and a decrease in venous stasis. Reduction of vascular resistance in the microcirculatory bed was accompanied by normalization of arterial pressure.
References
- Dedov Diabetes. 1998; 1: 2-18.
- Severina AS, Shestakova MV. New on the mechanisms of development, diagnosis and treatment of diabetic Diabetes. 2001; 3: 59-60.
- Ametov AS, Demidova T.Yu, Kosykh SA. Synthesis of nitric oxide in the vascular endothelium in patients with type 2 Klin med. 2005; 28: 62-68.
- Balabolkin I. Diabetology. M: Medicine. 2000; 672c.
- Aleksandrovsky Ya. A Diabetes Experiments and M: SIP RIA, 2005; 220.
- Bondar IA, Klimentov VV, Porshennikov Oxidative modification of proteins in diabetic microangiopathies. Diabetes. 2000; 3: 9-11.
- Kulagin. Pharmacological correction of alloxan diabetes and factors that cause the development of its complications. Chelyabinsk. 2000; 36c.
- Kokoreva Experimental substantiation of the effectiveness of some antioxidants in diabetes mellitus. Saransk. 2002; 19c.
- Rosca MG, Mustata TG, Kinter MT, et Glycation of mitochondrial proteins from diabetic rat kidney is associated with excess superoxide formation. Am J Physiol Renal Physiol. 2005; 289: F420-F430.
- Yin X, Zhang Y, Yu J, et al. The antioxidative effects of astragalus saponin I protect against development of early diabetic J Pharmacol Sci. 2006; 101: 166-173.
- Dunlop Aldose reductase and the role of the polyol pathway in diabetic neuropathy. Kidney Jut. 2000; 77: 3-12.
- Setter Stephan M. Biochemical pathways for microvascular complication of diabetes mellitus. Am Pharmacother. 2003; 37: 1858-1866.
- Yarek-Martynovskaya Ya, Shestakova MV. Diabetes mellitus and endothelial dysfunction. Diabetes. 2004; 2: 248-51.
- Dedov II, Shestakova Diabetes mellitus (Diagnosis, treatment, prevention). Honey Inform Agency M. 2011; 801c.
- Dedov II, Shestakova Diabetes M, 2003.
- Asakawa T, Matsushita Lipids, 1980; 15: 137-140.
- Korolyuk MA. Method for determination of catalase activity. Lab a business. 1988; 1: 16-19.
- Orphaned TV Method for determining the antioxidant activity of superoxide dismutase and chemical compounds. PatentN° 2144674. Patent class: G01N33 / 52, G01N33 / 68. Application number: 99103192/14.
- Metelskaya VA, Gumanova Nitric oxide: role in regulation of biological functions, methods of determination in human blood. Lab honey. 2005; 7: 19-24.
- Bitar MS, Wahid S, Mustafa S. et al. Nitric oxide dynamics and endothelial dysfunction in type II model of genetic Eur J Pharmacol. 2005; 511: 53-64.
- Shabab A. Why does diabetes mellitus increase the risk of cardiovascular disease? Asta Med 2006; 38: 33-41.
- Triggle CR, Ding H. A review of endotelian dysfunction in diabetes; A focus on the contribution of a dysfunctional eNOS, J Am Soc 2010; 4: 102-115.
- Kapelko VI, Ruuge Study of the action of coenzyme Q10 (ubiquinone) in ischemia and reperfusion of the heart. The use of the antioxidant drug kudesan (coenzyme Q10 with vitamin E) in cardiology. Moscow. 2002.