Patterns of COVID-19 Vaccination and Protective Equipment Usage in Endoscopy: A Survey of Endoscopy Providers
Author'(s): Kenneth W. Chow1, Matthew T. Bell1, Phoenix Nguyen2, Mary L. Krinsky3, and Sofiya Reicher1,4*
1Department of Medicine, Harbor-UCLA Medical Center, Torrance, California.
2Division of Gastroenterology, Hoag Medical Center, Newport Beach, California.
3Division of Gastroenterology, University California, San Diego, San Diego, California.
4Division of Gastroenterology, Harbor-UCLA Medical Center, Torrance, California.
*Correspondence:
Sofiya Reicher MD, Clinical Professor of Medicine, David Geffen School of Medicine at UCLA; Director of Endoscopy, Harbor-UCLA Medical Center; 1000 W Carson St, Torrance, California, 90502, Tel: 424-306-4210.
Received: 25 Aug 2022 Accepted: 23 Sep 2022 Published: 28 Sep 2022
Citation: Chow KW, Bell MT, Nguyen P, et al. Patterns of COVID-19 Vaccination and Protective Equipment Usage in Endoscopy: A Survey of Endoscopy Providers. Gastroint Hepatol Dig Dis. 2022; 5(2): 1-6.
Abstract
Background: Endoscopic procedures have an increased risk for COVID-19 transmission due to their production of respiratory droplets and aerosolized particles. Early case reports and surveys suggest that transmission risk during endoscopy is low given proper personal protective equipment (PPE) usage. However, the advent of new virus variants led to renewed concern regarding infection risk. We examined how these recent trends have affected patterns of COVID-19 positivity, endoscopy center pre-procedure screening protocols, PPE usage, and healthcare provider perceptions of safety in endoscopy.
Methods: We surveyed gastroenterologists, nurses, technicians, and other endoscopy unit personnel throughout the United States. The survey was sent on November 1, 2021 and November 15, 2021.
Results: Seventy-two individuals responded to the survey with a self-reported vaccination rate of 100%. Nine individuals (13%) reported testing positive for COVID-19, all of whom tested positive before vaccination. Fifty-one (71%) endoscopy workers received the booster dose, and 13 (18%) endoscopy workers planned to in the future. Seven (10%) had not received a booster dose and did not plan to, even if available. Fortythree (60%) individuals reported that their endoscopy center mandated routine COVID-19 testing for all patients undergoing endoscopy. Sixty-one respondents (85%) reported feeling safer performing endoscopic procedures after vaccination.
Conclusion: In our cohort, most endoscopy workers received the booster dose or planned to once available, and most reported feeling safer during endoscopy post-vaccination. Although the American Gastroenterological Association had recommended against routine COVID-19 screening prior to elective endoscopy, 60% of respondents reported that their endoscopy center mandated routine pre-procedural screening. Even with the advent of the highly transmissible Delta variant in early 2021, COVID-19 transmission during endoscopy remained low given vaccination and proper PPE utilization. Further data is needed to shape practicechanging guidelines regarding booster vaccine mandates and pre-procedural screening in high-risk fields such as endoscopy.
Keywords
Introduction
COVID-19 is believed to spread through respiratory droplets and aerosolized particles secreted by infected individuals [1]. Endoscopy is associated with the generation of respiratory droplets and aerosols [2], and endoscopic procedures are typically performed in relatively small and enclosed suites that contain multiple providers such as endoscopists, anesthetists, nurses, and technicians. Thus, without appropriate personal protective equipment (PPE), endoscopy poses a significant risk for COVID-19 transmission. In a cohort of 368 healthcare workers, it was found that the department of gastroenterology had the second-highest prevalence of COVID-19 viral exchange [3]. Although there have been case series and cross-sectional studies that examined the extent of COVID-19 transmission in endoscopy, these studies were performed early in the pandemic and results varied from 1% to 13.5% of endoscopy workers who reported testing positive and attributed this to endoscopy [4,5].
Subsequent society guidelines suggest that disease transmission is relatively low given proper PPE utilization [6]. Regardless, the COVID-19 pandemic has drastically affected gastrointestinal practice worldwide. During the initial surge of cases in early 2020, many endoscopy centers cancelled elective endoscopic procedures, leading to delayed cancer diagnoses and patient follow-up. The advent of the COVID-19 vaccine in late 2020 has been shown to reduce both disease transmission and severity. However, the rise of novel virus variants such as the Delta variant in early 2021 has led to renewed concern regarding infection risk. On August 2021, the Food and Drug Administration (FDA) authorized the use of a third booster vaccination dose. Unfortunately, vaccine hesitancy has grown in certain subgroups of healthcare providers and patients alike, fueled by misinformation from anti-vaccination groups. We examined how these recent trends affected patterns of COVID-19 positivity, endoscopy center pre-procedure screening protocols, protective equipment usage, and healthcare provider perceptions of safety in endoscopy.
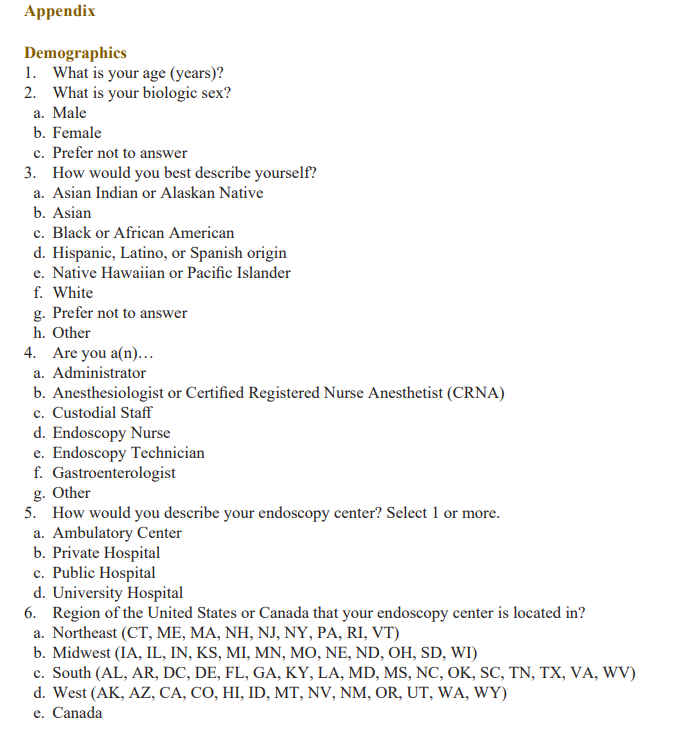
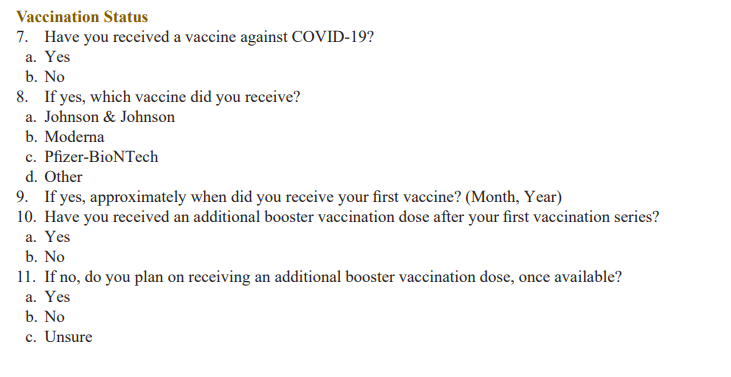
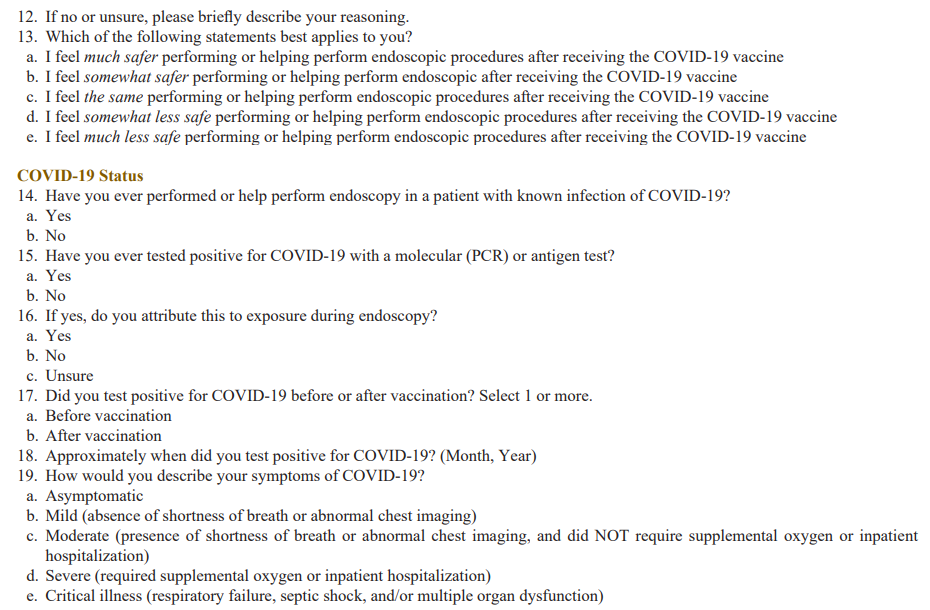
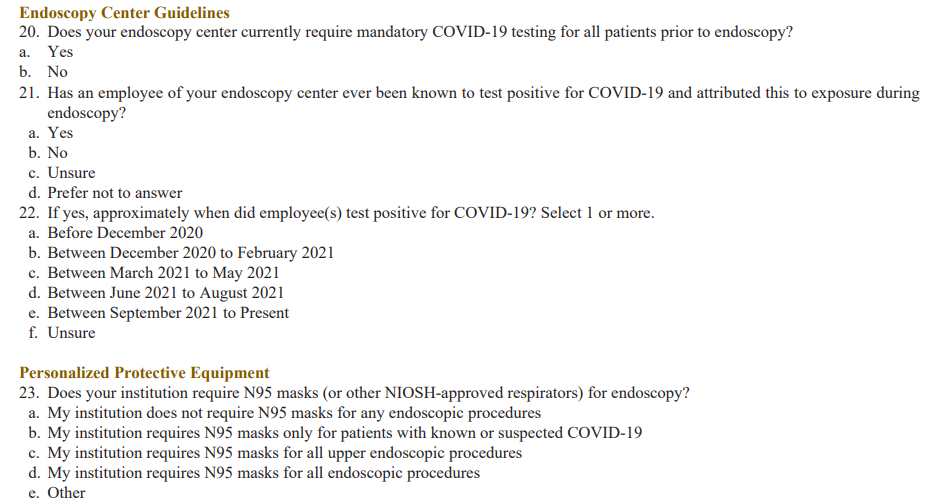
We surveyed gastroenterologists and endoscopy unit personnel throughout the United States and assessed patterns of COVID-19 positivity among providers, vaccination status, COVID-19 pre- procedural testing protocols, PPE usage, and healthcare provider perception of safety in endoscopy. An email database of 700 endoscopy workers was used. The survey was anonymous and was sent out twice: first on November 1, 2021, and again on November 15, 2021. It consisted of up to 25 questions using branched logic and required less than 5 minutes for completion (Appendix).
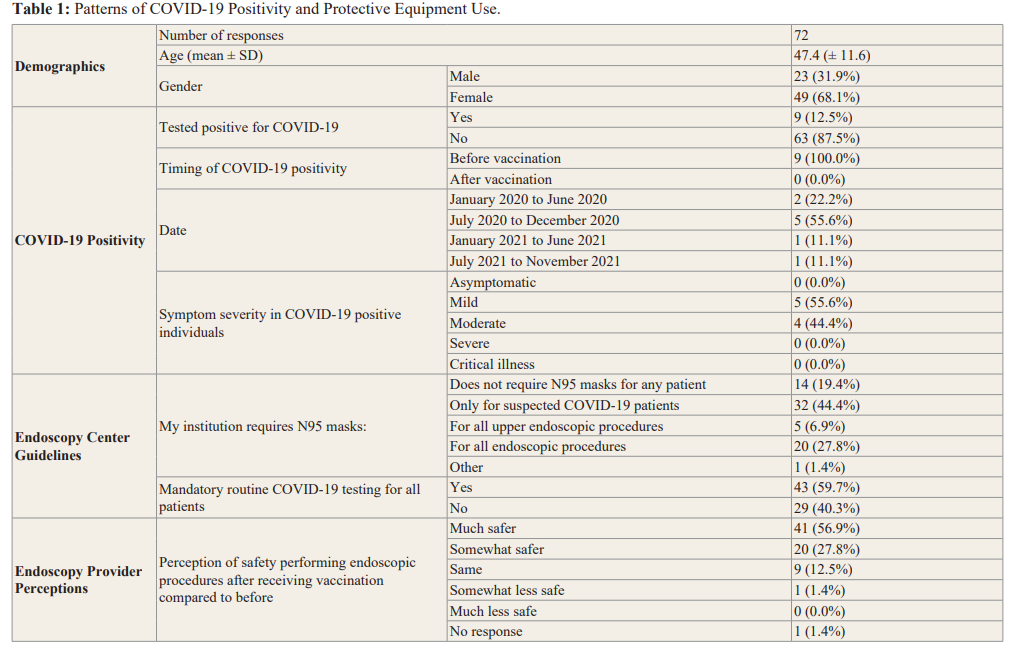
Seventy-two individuals responded to the survey, with a self- reported vaccination rate of 100%. Fifty-two respondents (72.2%) received the Pfizer vaccine, 15 (20.8%) received the Moderna vaccine, and 5 (6.9%) received Johnson and Johnson vaccine. The average age of respondents was 47.4 years, and 49 (68.1%) identified as female. Nine individuals (13%) reported testing positive for COVID-19, all of whom tested positive before vaccination. Of those who tested positive, 7 (77.8%) cases occurred before 2021. Fifty-one (71%) endoscopy workers received the booster dose, and 13 (18%) endoscopy workers planned to in the future. Seven (10%) had not received a booster dose and did not plan to, even if available. Fourteen respondents (19.4%) reported that their institution did not require advanced masks (i.e. N95) for any patients, while the remainder reported some degree of advanced masking requirement. Forty-three (59.7%) individuals reported that their endoscopy center mandated routine COVID-19 testing for all patients undergoing endoscopy. Sixty-one respondents (85%) reported feeling safer performing endoscopic procedures after vaccination (Table 1).
In our cohort, no individuals tested positive for COVID-19 after receiving their first vaccination series, compared to 9 individuals (13%) who tested positive before vaccination. The majority (77.8%) of positive tests occurred before January 2021, which is approximately when vaccines began their roll-out in the United States. Most endoscopy workers (90.1%) received the booster dose or planned to once available. Most respondents (85%) report feeling safer during endoscopy post-vaccination. Although the American Gastroenterological Association (AGA) recommended against routine COVID-19 screening prior to elective endoscopy [6], 60% of respondents reported that their endoscopy center mandated routine pre-procedural screening. Although seemingly well intentioned, mandatory pre-procedural screening can exacerbate disparities in healthcare access, with one study demonstrating that minority patients were three times as likely to experience COVID-19-related pre-endoscopy cancellations [7]. Our findings suggest that even with the advent of the highly transmissible Delta variant in early 2021, COVID-19 transmission during endoscopy remained low given vaccination and proper PPE utilization. Further data is needed to shape practice-changing guidelines regarding booster vaccine mandates and pre-procedural screening in high-risk fields such as endoscopy, especially with the continually emerging variants of COVID-19.
References
- Lotfi M, Hamblin MR, Rezaei N. COVID-19: Transmission, prevention, and potential therapeutic Clin Chim Acta. 2020; 508: 254-266.
- Sagami R, Nishikiori H, Sato T, et Aerosols produced by upper gastrointestinal endoscopy: a quantitative evaluation. Am J Gastroenterol. 2021; 116: 202-205.
- Musa S, Abdel Alem S, Amer K, et al. Prevalence of SARS- CoV-2 infection and dynamics of antibodies response among previously undiagnosed healthcare workers in a university hospital: A prospective cohort study. J Infect Public Health. 2021; 14: 1466-1473.
- Arantes VN, Martins BC, Seqatto R, et al. Impact of coronavirus pandemic crisis in endoscopic clinical practice: Results from a national survey in Brazil. Endosc Int Open. 2020; 8: 822-829.
- Parasa S, Reddy N, Faigel DO, et al. Global impact of the covid-19 pandemic on endoscopy: an international survey of 252 centers from 55 countries. Gastroenterology. 2020; 159: 1579-1581.
- Sultan S, Siddique SM, Singh S, et Aga rapid review and guideline for sars-cov2 testing and endoscopy post- vaccination: 2021 update. Gastroenterology. 2021; 161: 1011-1029.
- Aby ES, Sultan S, Vaughn Endoscopy COVID-19 Testing Requirements Disproportionately Affect Communities That Are Medically Underserved and May Worsen Health Care Disparities. Gastroenterology. 2022; 163: 795-799.