Performance of Pleuropulmonary Ultrasound in the Diagonisis of Acute Respiratory Conditions in Intensive Care Patients: Case of the Sens Hospital Center
Author'(s): Dan Kankonde1,2, Joseph Nsiala1, Wilfrid Mbombo1*, Daniel Tonduangu2, Gilbert Meziere2, Dominique Gizolme2, Médard Bula-Bula1, Erick Amisi1, Chris Nsituavibidila1, Lionel Diyamona1, Jean Claude Mubenga1, Noelly Mukuna1, Khazy Anga1, Gracia Likinda1, Jean Jacques Kalombo1, Christelle Nkombe1, Doliane Mambu1, Franklin Nzungu1 and Berthe Barhayiga1
1Department of Anesthesia and Intensive Care of the University Clinics of Kinshasa/D.R.Congo.
2Resuscitation Department of the Sens Hospital Center /France.
*Correspondence:
Wilfrid Mbombo, Department of Anesthesia and Intensive Care of the University Clinics of Kinshasa/DR Congo, Tel.+243810054829.
Received: 02 Oct 2023; Accepted: 05 Nov 2023; Published: 12 Nov 2023
Citation: Kankonde D, Nsiala J, Mbombo W, et al. Performance of Pleuropulmonary Ultrasound in the Diagonisis of Acute Respiratory Conditions in Intensive Care Patients: Case of the Sens Hospital Center. Anesth Pain Res. 2023; 7(2): 1-5.
Abstract
Background and Objective: Despite its increasing use, in critical care, the diagnosis accuracy of Lung Ultransound Sonographye (LUS) is a topic that remains highly debated. The objective of our study was to evaluate the performance of LUS compared to chest computer tomography (CT) in the diagnosis of acute respiratory condictions in critical patients at Sens hospital from March 1st to September 31st 2023.
Methods: Single-center, cross-sectional study of 54 patients, all adult with acute respiratory symptoms who benefited concurrent LUS and chest CT scan. The LUS was performed according to the BLUE-Protocol by the doctors of the department, within 8 hours before the chest CT scan was performed. The CT scan was interpreted by the hospital's radiologists who were also blinded by the LUS results. The performance of LUS was assessed by calculating sensitivity (se), specificity (sp), positive predictive values (PPV) and negative predictive values (NPV) compared to chest CT.
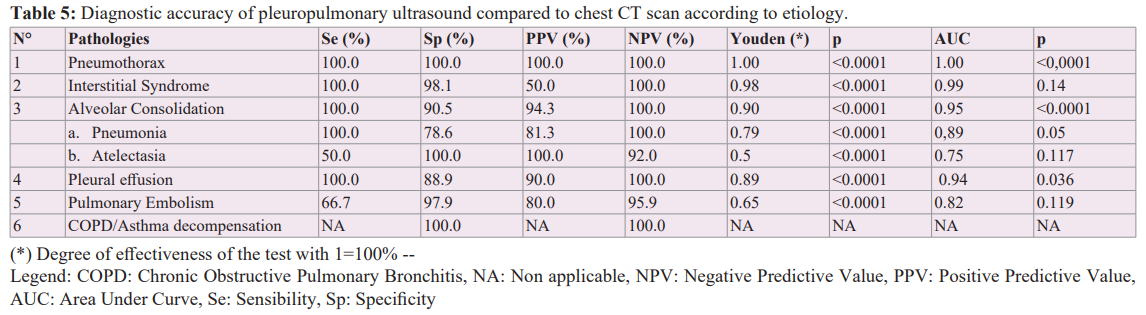
Results: Pneumothorax had a Se=100%, Sp=100, PPV=100%, NPV=100%, Youden=1.00, AUC=1.00; Interstitial syndrome had a Se=100%, Sp=98.1%, PPV=50%, NPV=100%, Youden=0.98%, AUC=0.99 with p=0.14. Alveolar consolidation had Se=100%, Sp=90.5%, PPV=94.3%, NPV=100%, Youden=0.90%, AUC=0.95%. Pleural effusion had Se=100%, Sp=88.9%, PPV=90%, NPV=100%, Youden=0.89%, AUC=0.94%. Pulmonary embolism had a Se=66.7%; Sp=97.9%, PPV=80%, NPV=95.9%, Youden=0.65%, AUC=0.82% with p=0.11. As for COPD/ Asthma decompensation, she had a Se=NA (not applicable), Sp=100%, PPV=NA, NPV=100%, Youden=NA and AUC=100%.
Conclusion: The performance of LUS in this study are satisfactory for the diagnosis of alveolar consolidation, pneumothorax, pleural fluid effusion and interstitial syndrome (only as a function of Youden's index). They are less good for the diagnosis of pulmonary embolism. Thus, we propose it as an alternative to CT in patients in critical resuscitation.
Keywords
Introduction
Many patients are admitted to intensive care units for acute respiratory illnesses [1]. These conditions include pneumonia, pneumothorax, pleural effusion, pulmonary embolism, chronic obstructive pulmonary disease (COPD)/asthma decompensation [1]. The prevalence of these acute respiratory diseases is approximately 7.1% and an overall intensive care unit (ICU) mortality rate is 72% [2]. They require a quick and accurate diagnosis for better management. In the past, the diagnosis of these conditions was based on physical examination and chest X-ray [3]. Several studies have shown that chest X-ray has low sensitivity (49%). So, the current reference imaging test to explore the chest is CT scan [4]. As for pleuropulmonary ultrasound, its use has been on the rise in recent years [1]. However, its diagnostic performance is not clearly established. Indeed, most studies, in a recent meta- analysis evaluating the diagnostic performance of pleuropulmonary ultrasound, were hampered by multiple methodological limitations [4]. The design was not the same in all these studies. They were not carried out under the usual conditions of care. Some excluded patients with multiple diagnoses. Pleuropulmonary ultrasound operators were not always blinded by the results of the CT scan. Often, the quality of the operators was not known. The comparator was still not the gold standard. Thus, in current recommendations, the place of pleuropulmonary ultrasound in critical care remains to be clarified [5].
In any case, this examination, which is inexpensive and easy to perform, could be an interesting alternative to CT scans in countries with limited resources and if the patient is difficult to transport because it is unstable. It is in this context that we felt it necessary to conduct this study whose objective was to evaluate the diagnostic performance of lung ultrasound compared to chest CT in the diagnosis of acute respiratory conditions in critical care patients at Sens hospital Cente (France) from 01 March to 31 September 2023.
Methods
Type and study framework
This is a single-center, double-blind, cross-sectional study. All ultrasounds were performed by an anaesthesia-intensive care intern after 6 months of prior training under the supervision of a hospital practitioner experienced in pleuropulmonary ultrasound. The gold standard test was chest CT scan interpreted by a radiologist. The person performing the ultrasound was not aware of the results of the CT scan and vice versa. Our study took place from March to September 2023 in the intensive care unit (12 beds) of the Centre Hospitalier de Sens located in the Bourgogne Franche-Comté region in France.
Study population
All adult patients (age ≥18 years), mechanically ventilated or not,with respiratory symptoms and who underwent pleuropulmonary ultrasound and CT concurrently were included. Patients were excluded if the time between lung ultrasound and CT was greater than 8 hours. Patient recruitment was done consecutively.
Ultrasound Protocol
The performance of the lung ultrasound was in accordance with the "BLUE Protocol". We had used the Mindray device with a convex abdominal probe of 1.3 to 5.7 MHz frequency. Patients were placed in a semi-sitting or strict supine position. Each hemithorax was divided into 3 regions separated from each other by the anterior and posterior axillary lines. Each region is subdivided into 2 quadrants: Upper and Lower. Three standardized points were evaluated: Upper BLUE-Point, Lower BLUE-Point and PLAPS- Point (Posterolateral Alveopleural Syndrome). The upper and lower BLUE-points were used for the assessment of the anterior region of the lung and the PLAPS-Point for the posterior region [1].
The ultrasound items sought were the Lines, which are repetitive horizontal artefacts from the pleural line, generated by the subpleural air that blocks ultrasound waves [2]. In the case of predominant A-lines, an A-Profile was designated [1]. Lines B, vertical artefact must have 7 characteristics (Vertical lines, arising from the pleural line, moves with it if present, hyperechoic, well- defined, obliterating line A and propagating indefinitely) [2]. It took at least 3 in a bilateral view and manner to suggest interstitial syndrome [2]. A profile B was assigned in the case of at least 3 B lines either at the top or at bottom of the BLUE point [1]. Consolidation resulted in a tissue pattern [2].
A profile C was designated in case of hypoechoic subpleural image restricted by an irregular border (sign of shredding) and B profile cancelled if present. At the PLAPS point, the presence of pleural effusion or consolidation was investigated. Pleural effusion was diagnosed when there was an anechoic area between the parietal and visceral pleura [1]. Anterior lung slippage was checked first. His presence was expected to be a pneumothorax. Earlier B-lines were sought. Profile B was suggestive of pulmonary oedema. Profiles B', A/B and C suggested alveolar consolidation. Profile A was an invitation to look for venous thrombosis. If present, pulmonary embolism was considered. In case of absence, the PLAPS was called upon. Its presence (Profile A and PLAPS) suggested alveolar consolidation, its absence (Normal Profile) suggested a decompensation of COPD/Asthma [2].
Data collection and outcomes
The following data were collected prospectively: patient demographic characteristics (age, sex, body mass index (BMI)), medical history, respiratory symptoms at the time of examination, laboratory data requested as part of routine care (Blood gas, Biological inflammatory Syndrome, CRP, PCT, D-Dimer, BNP, Troponin), diagnoses suggested by pleuropulmonary ultrasound and CT scan. We also noted the interval between the ultrasound and chest CT scan.
Evaluation criteria
The outcome measure was the performance of ultrasound in detecting interstitial syndrome, alveolar consolidation,pneumothorax, fluid pleural effusion, pulmonary embolism, and COPD/asthma decompensation. The performance indicators used for the comparison between ultrasound and chest CT were sensitivity (Se), specificity (Sp), positive predictive values (PPV) and negative predictive values (NPV) as well as area under the ROC curve (AUC) and youden index.
Statistical Analyzes
A population of about fifty patients to be included was estimated by analogy with the studies previously carried out. The data was entered into an Excel file, encoded and transferred to SPSS 26. 0 for analysis. The quantitative variables in our patients' characteristics are expressed as an average with their standard deviation and the qualitative variables as a percentage with their 95% confidence interval. Performance indicators are estimated by proportions. For all tests, the p-value was set at <0.05.
Ethical and Regulatory Aspects
This study has received authorization from the Commission Nationale de l'Informatique et des Libertés (CNIL). Informed consent was signed by all patients. The principle of confidentiality and anonymity was respected in accordance with the Helsinki Convention. We have not a conflict of interest in this study.
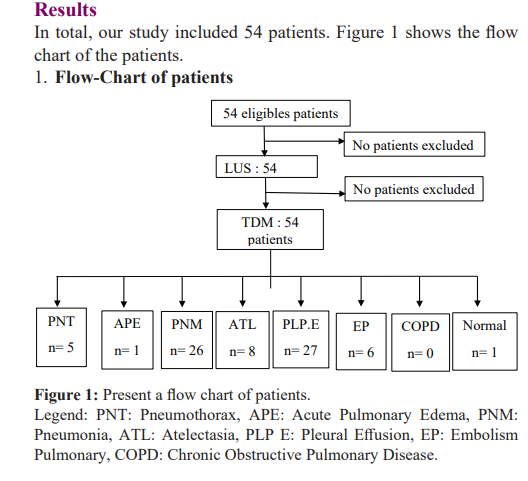
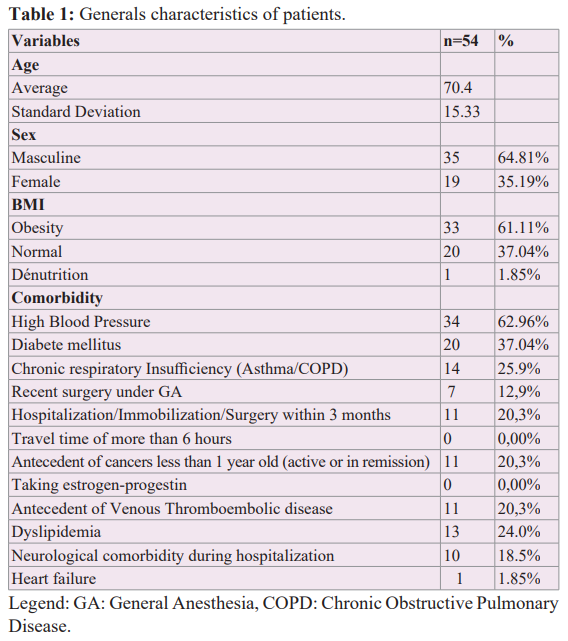
Generals Characteristics of Patients
The general characteristics of our patients are described in Table 1. The mean age was 70.4 ± 15.33 years with a sex ratio of 1.8. 61% of our patients were obese and one patient (2%) was undernourished. High blood pressure (62.96%) was the main comorbidity, followed by diabetes mellitus (37.04). Chronic respiratory failure (asthma or COPD) and dyslipidemia were present in one in four patients. Moreover, 20.37% of patients had a history of cancer and hospitalization within 3 months.
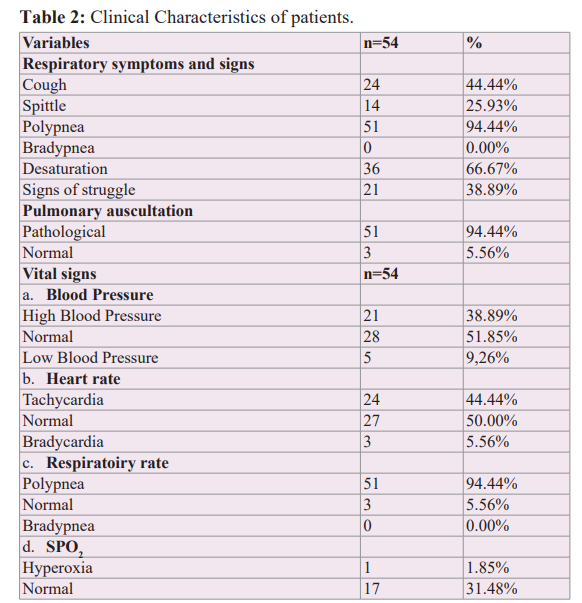
Clinical Characteristics of patients
Patients' symptoms and clinical signs are presented in Table 2. Almost all patients had polypnea. Fever was found in 28% of cases. 66.67% of patients were hypoxemic. Pulmonary auscultation was pathological in 94% of cases.

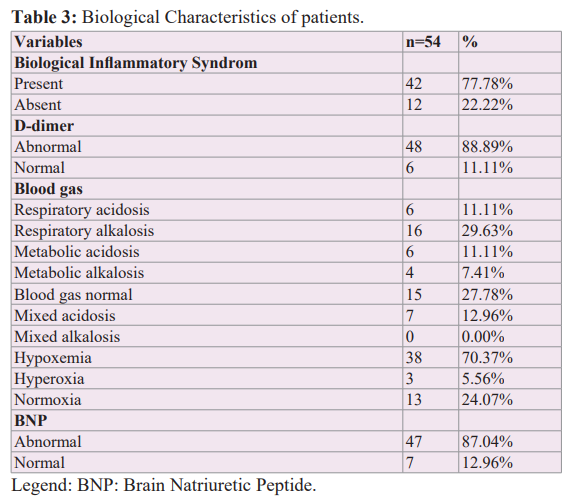
Biological Examinations for Etiological Purposes
Laboratory tests for etiological purposes are shown in Table 3. Hypoxemia were present in 38 patients (70.37%). The majority of patients had abnormal levels of D-Dimer and BNP.
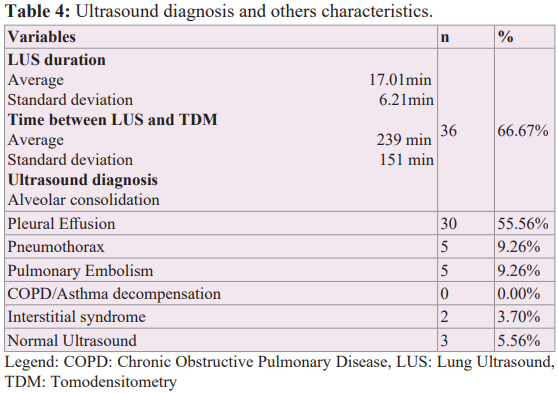
Ultrasound Diagnosis and Characteristics
Table 4 presents ultrasound diagnosis, LUS duration and time between LUS and TDM. All ultrasounds were performed in 17.01± 6.21 minutes on average. The interval between the completion of the pleuropulmonary ultrasound and the chest CT scan was 139± 151 minutes (3h59 ± 2h30) on average. Alveolar consolidation was present in 66.67% of patients, pleural effusion 55.56%, pneumothorax and pulmonary embolism in 9.26%, interstitial syndrome in 3.70% of patients Legend: COPD: Chronic Obstructive Pulmonary Disease, LUS: Lung Ultrasound,TDM: Tomodensitometry
Diagnostic Accuracy of Pleuropulmonary Ultrasound Compared to Chest CT Scan According to Etiology
Table 5 presents the diagnostic accuracy of pleuropulmonary ultrasound compared to CT scan results by etiology. According to the Youden index, ultrasound is highly effective in diagnosing pneumothorax, interstitial syndrome, alveolar consolidation, and pleural effusion. However, it is less effective (<70%) in cases of pulmonary embolism. Considering the ROC curve, the area under curve (AUC) of ultrasound performs well in cases of pneumothorax (auc: 1; p: <0.0001), alveolar consolidation (auc: 0.95; p: <0.0001) and fluid pleural effusion (auc: 0.94; p: 0.036).
Discussion
The sensitivity and specificity of pleuropulmonary ultrasound to detect alveolar consolidation and interstitial syndrome in our study is similar to that found in previous studies [4,5]. As for the results found in the study by Jasper Smit et al. [1], the sensitivity and specificity were lower than ours. This may be justified by the fact that they used the linear probe rather than the convex (abdominal or micro convex) as suggested in the literature because they allow for better visualization of B-lines [6-9]. Also, in our study, the ultrasounds were supervised by a very experienced intensive care physician. The pneumothorax in the same study [1] had a low sensitivity compared to that found in our study. This is because for Previous studies [1,4,10,11] have not evaluated the performance of ultrasound in diagnosing COPD decompensation. We think this is probably because pleuropulmonary ultrasound is normal in this condition, a situation that could confuse a truly normal ultrasound with this clinical situation. In our series, we were unable to diagnose any COPD decompensation. On the other hand, we noted three normal LUS that we did not consider to be COPD decompensation because these patients did not present the profile of COPD (both on the history and on the physical examination). Thus, the results on this performance were not applicable. The majority of our patients had multiple diagnoses at once, mirroring real life. However, it was not possible to calculate the sensitivity and overall specificity of LUS as was the case with some studies [2,4].
All in all, contrary to what the authors of the meta-analysis think (that the LUS could be taken as a first-line test to diagnose respiratory pathologies), in view of our imperfect results, we rather think that it could be an alternative to the bedside CT scan, especially when they are unable to transport (due to the fragility of their clinical condition) and for low-income settings where chest CT remains a luxury for patients.
Strengths and limitations
Our limitations included the small size of our population and the monocentric nature of the study. Inclusion of patients with multiple diagnoses, reflecting real life; the blindness of pleuropulmonary ultrasound operators and radiologists. The use of the Gold Standard as a comparator examination and the evidence of the performance of pleuropulmonary ultrasound were the strengths of our study.
Conclusion
The performance of pleuropulmonary ultrasound found in this study is satisfactory for detecting alveolar consolidation,pneumothorax and fluid pleural effusion and interstitial syndrome (only according to Youden's index). They are less good for the diagnosis of pulmonary embolism. Thus, we think that it could be an alternative to CT scanning, especially in low-income countries where it remains a luxury, even when the patient cannot be moved.
Acknowledgements
We would like to thank the whole team in the intensive care unit at Sens Hospital: the anaesthetists, nurses, physiotherapists and care assistants.
References
- Smit JM, Mark E Haaksma, Michiel H. Winkler, et al. Lung ultrasound in a tertiary intensive care unit population: a diagnostic accuracy study. Crit Care. 2021; 25: 339.
- Brun Buisson C, Cosetta Minelli, Guido Bertolini, et Epidemiology and outcome of acute lung injury in European intensive care units. Results from the ALIVE study. Intensive Care Med. 2004; 30: 51-61.
- Lichtenstein DA, Mezière GA. Relevance of lung ultrasound in the diagnosis of acute respiratory failure: the BLUE Chest. 2008; 134: 117-125.
- Winkler MH, Touw HR, van de Ven PM, et al. Diagnostic Accuracy of Chest Radiograph, and When Concomitantly Studied Lung Ultrasound, in Critically Ill Patients With Respiratory Symptoms: A Systematic Review and Meta- Crit Care Med. 2018; 46: 707-714.
- Libertario Demi, Frank Wolfram, Catherine Klersy, et New International Guidelines and Consensus of the Use of Lung Ultrasound. J Ultrasound Med. 2023; 42: 309-344.
- Lichtenstein DA. Current Misconceptions in lung ultrasound:A Short guide for experts. Chest. 2019; 156: 21-25.
- Daniel LA. Lung Ultrasound in critically ill. Ann Intensive 2014; 4: 1.
- Daniel Whole Body Ultrasound in Critical Patients, Springer-Verlag Berlin Heidelberg. Bull Acad Natl Med. 2007; 191: 495-516.
- Daniel Lung Ultrasound. Elsevier. 2003; 20-28.
- Tierney DM, Joshua S Huelster, Josh D Overgaard, et al. Comparative Performance of Pulmonary Ultrasound, Chest Radiograph, and CT Among Patients With Acute Respiratory Crit Care Med. 2020; 48: 151-157.
- Gazon M, Eboumbou N, Robert MO, et Viale Concordance analysis between chest ultrasound and chest X-ray in intensive care. Elsevier. 2010.