Prevalence and Predictors of Cannabis Use Disorder among Inflammatory Bowel Disease Hospitalizations in the United States and its Effect on Length of Stay
Author'(s): Yize Richard Wang*
Cooper Digestive Health Institute, Cooper Medical School of Rowan University, USA.
*Correspondence:
Yize Richard Wang, MD, PhD, Cooper Digestive Health Institute, Cooper Medical School of Rowan University, 501 Fellowship Road, Suite 101, Mt Laurel, NJ 08054, USA.
Received: 26 Jan 2022 Accepted: 24 Feb 2022; Published: 02 Mar 2022
Citation: Wang YR. Prevalence and Predictors of Cannabis Use Disorder among Inflammatory Bowel Disease Hospitalizations in the United States and its Effect on Length of Stay. Gastroint Hepatol Dig Dis. 2022; 5(1): 1-4.
Abstract
Background: The prevalence of cannabis use has been increasing in the United States in recent years. We examined the prevalence and predictors of cannabis use disorder among IBD hospitalizations and its effect on length of stay.
Methods: Using the 2017 National Inpatient Sample, cannabis use disorder was identified using ICD-10-CM code F12.xxx in adult IBD patients. Other variables of interest included age, sex, race, Crohn’s disease (vs. ulcerative colitis), region, metropolitan status, zip code household income, primary insurance, and length of stay. Multivariate logistic and Poisson regressions were used in statistical analysis.
Results: Of the 17,857 IBD hospitalizations, 565 (3.1%) had cannabis use disorder. Patients with cannabis use disorder were younger (mean ± standard deviation [years]: 35.1 ± 11.8 vs. 45.6 ± 18.1), less likely female (32.7% vs. 54.1%), more likely African American (24.8% vs. 13.9%), and more likely Crohn’s disease (72.0% vs. 62.2%) (all p<0.001). There were also significant differences by region, income, and insurance. Multivariate logistic regression confirmed age (odds ratio [95% confidence interval]: 0.964 [0.957, 0.971]), female (0.444 [0.369, 0.531]), African American (1.405 [1.124, 1.750]), and Crohn’s disease (1.363 [1.126, 1.657]) as predictors of cannabis use disorder. There was no association between cannabis use disorder and length of stay, confirmed in multivariate Poisson regression.
Conclusions: Young age, male sex, African American race, and Crohn’s disease were positively associated with cannabis use disorder in IBD hospitalizations. There was no effect of cannabis use disorder on length of stay.
Keywords
Introduction
The prevalence of cannabis use has been increasing in the United States in recent years [1-3]. In small studies, cannabis use improved inflammatory bowel disease (IBD) symptoms, including pain, nausea, and decreased appetite [4,5]. There is no evidence that cannabis can reduce IBD inflammation or improve disease activity [6,7].
In this study, we examined the prevalence and predictors of cannabis use disorder among IBD hospitalizations in the United States in 2017 and studied the effect of cannabis use disorder on length of hospital stay.
Data and Methods
Using the 2017 National Inpatient Sample [8], the largest publicly available database of inpatient admissions in the United States, we first identified adult IBD hospitalizations as those aged 18 years or older and with the primary diagnosis of either Crohn’s disease (ICD-10-CM diagnosis code K50.xxx) or ulcerative colitis (K51. xxx). Patients with cannabis use disorder were identified using the ICD-10-CM diagnosis code F12.xxx present in any of the 39 secondary diagnoses.
Other variables of interest included patient age, sex, race (White, African American, Hispanic, and other), hospital region (Northeast, Midwest, South, and West), metropolitan status (large or not), zip code household median income (above or below the national median), primary insurance (Private, Medicare, Medicaid, and other), and length of stay.
The Student’s t-test, chi-square test, multivariate logistic regression, and multivariate Poisson regression were used in statistical analysis.
Results
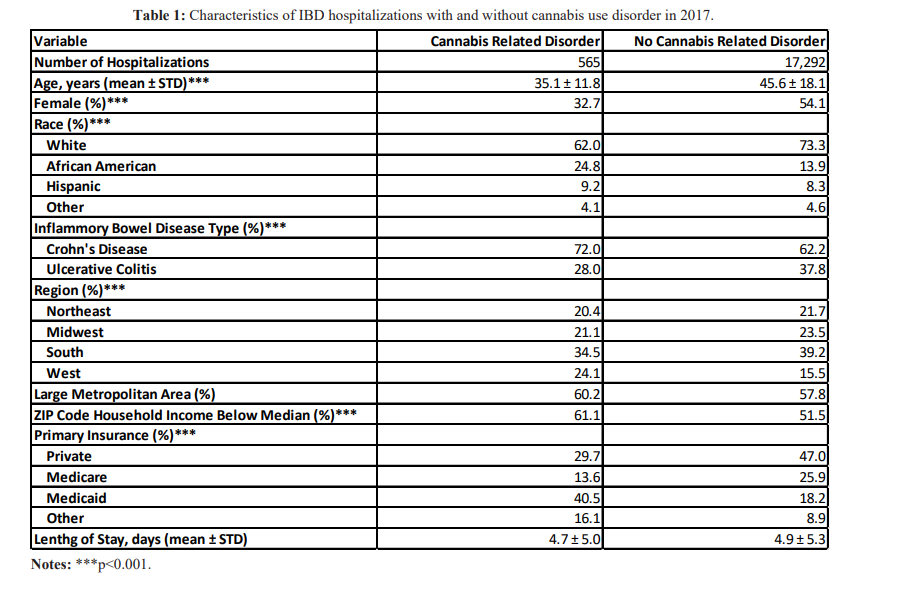
Of the 17,857 IBD hospitalizations, 565 (3.1%) had cannabis use disorder. Compared to patients without cannabis use disorder, those with cannabis use disorder were younger (mean ± standard deviation [years]: 35.1 ± 11.8 vs. 45.6 ± 18.1), less likely female (32.7% vs. 54.1%), more likely African American (24.8% vs. 13.9%), and more likely Crohn’s disease (72.0% vs. 62.2%) (all p<0.001) (Table 1). There were also significant differences between patients with cannabis use disorder and those without the disorder in region (West: 24.1 % vs 15.5%), zip code household median income (Below median: 61.1% vs. 51.5%), and primary insurance (Medicaid: 40.5% vs. 18.2%) (all p<0.001). There was no significant difference in length of stay (4.7 ± 5.0 days vs. 4.9 ± 5.3 days).
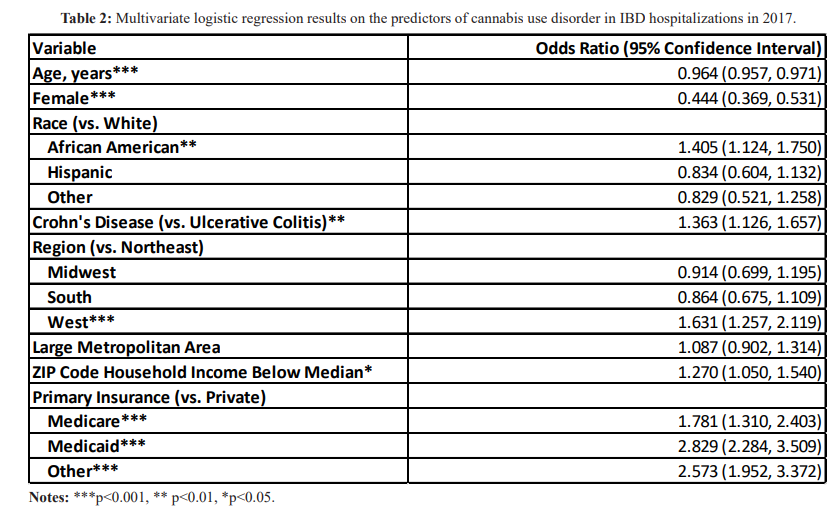
In the multivariate logistic regression, patient age (odds ratio [95% confidence interval]: 0.964 [0.957, 0.971]), female sex (0.444 [0.369, 0.531]), African American race (1.405 [1.124, 1.750]), and Crohn’s disease (vs. ulcerative colitis: 1.363 [1.126, 1.657]) were significant predictors of cannabis use disorder (Table 2). The other significant predictors included West region (vs. Northeast: 1.631 [1.257, 2.119]), zip code household median income (below vs. above the national median: 1.270 [1.050, 1.540]), and primary insurance other than private insurance (Medicare 1.781 [1.310, 2.403]; Medicaid 2.829 [2.284, 3.509]; other 2.573 [1.952, 3.372]).
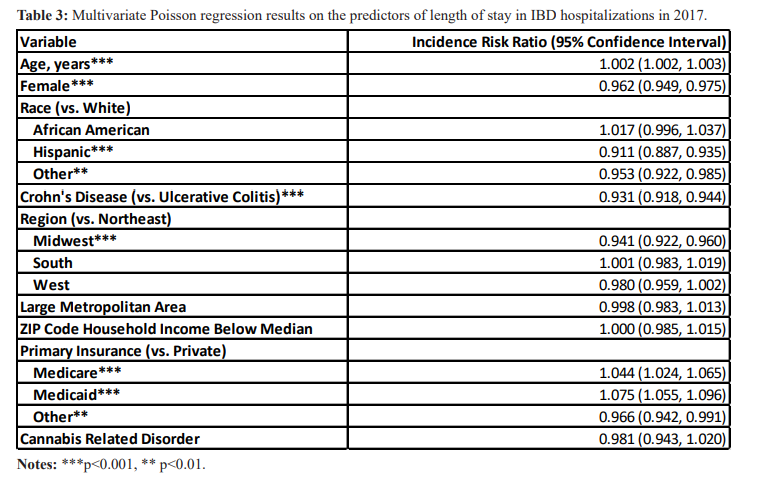
In the multivariate Poisson regression, cannabis use disorder is not a significant predictor of length of stay (incidence risk ration [95% confidence interval]: 0.981 [0.943, 1.020]) (Table 3). The significant predictors of length of stay included patient age, sex, race, Crohn’s disease, and primary insurance.
Conclusions
In this retrospective observational study, we found that young age, male sex, African American race, and Crohn’s disease were positively associated with cannabis use disorder in admitted IBD patients in 2017. Cannabis use disorder was not associated with any change in length of stay. Our findings are in line with previous studies noting an increase in cannabis use by IBD patients in the United States, similar to the general population trends [9-11]. Whether increasing cannabis use is associated with better or worse IBD outcomes is an important topic for future research.
Our study has a number of limitations. The National Inpatient
Sample is a 20% sample of all inpatient admissions in the United States, but it does not include a unique patient identifier. Some IBD patients might be admitted more than once in 2017 and overrepresented in our study sample. We do not have access to important clinical details on the location and severe of IBD, although IBS patients admitted for inpatient care tend to suffer from severe disease activity. Future studies using an outpatient IBD database or ideally an IBD registry over time may address these limitations.
References
- Cerda M, Wall M, Keyes KM, et al. Medical marijuana laws in 50 states: investigating the relationship between state legalization of medical marijuana and marijuana use, abuse and dependence. Drug Alcohol Depend. 2012; 120: 22-27.
- Hasin DS, Saha TD, Kerridge BT, et al. Prevalence of marijuana use disorders in the United States Between 2001- 2002 and 2012-2013. JAMA 2015; 72: 1235-1242.
- Charilaou P, Agnihotri K, Garcia P, et Trends of Cannabis Use Disorder in the Inpatient: 2002 to 2011. Am J Med. 2017; 130: 678-687.
- Naftali T, Bar-Lev Schleider L, Dotan I, et al. Cannabis induces a clinical response in patients with Crohn's disease: a prospective placebo-controlled study. Clin Gastroenterol Hepatol. 2013; 11: 1276-1280.
- Naftali T, Bar-Lev Schleider L, Sklerovsky Benjaminov F, et al. Medical cannabis for inflammatory bowel disease: real-life experience of mode of consumption and assessment of side- effects. Eur J Gastroenterol Hepatol. 2019; 31: 1376-1381.
- Kafil TS, Nguyen TM, MacDonald JK, et Cannabis for the treatment of Crohn's disease. Cochrane Database Syst Rev. 2018; 11: CD012853.
- Wynne J, Kozuch P. Medical marijuana for inflammatory bowel disease: the highs and lows. Scand J Gastroenterol. 2022; 57: 197-205.
- HCUP Databases. Healthcare Cost and Utilization Project (HCUP). Available at: https://www.hcup-us.ahrq.gov/jsp.
- Ravikoff Allegretti J, Courtwright A, Lucci M, et Marijuana use patterns among patients with inflammatory bowel disease. Inflamm Bowel Dis. 2013; 19: 2809-2814.
- Kerlin AM, Long M, Kappelman M, et Profiles of patients who use marijuana for inflammatory bowel disease. Dig Dis Sci. 2018; 63: 1600-1604.
- Merker AM, Riaz M, Friedman S, et al. Legalization of medicinal marijuana has minimal impact on use patterns in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2018; 24: 2309-2314.