Prevalence and Risk Factors for Peripheral Arterial Disease in Type 2 Diabetic Out Patients in A Care Center in Cotonou
Author(s): Comlan Jules Gninkoun1, Annelie Kerekou Hode1, Marie Jésus Ahoudjinou1, Géraud Sètondji Padonou2, Hubert Dedjan1, and Joseph Fanou1
1Service d’Endocrinologie & Diabétologie, Faculté des Sciences de la Santé, Cotonou, Bénin.
2Centre Hospitalier et Universitaire Suru Léré, Faculté des Sciences de la Santé, Cotonou, Bénin.
*Correspondence:
Dr Comlan Jules Gninkoun, MD, Senior Lecturer, Service d’Endocrinologie & Diabétologie, Faculté des Sciences de la Santé, Cotonou, Bénin.
Received: 02 May 2021 Accepted: 25 May 2021
Citation: Gninkoun CJ, A Kerekou Hode, Ahoudjinou MJ, et al. Prevalence and Risk Factors for Peripheral Arterial Disease in Type 2 Diabetic Out Patients in A Care Center in Cotonou. Diabetes Complications. 2021; 5(2); 1-4.
Abstract
Aim: To determine the prevalence of peripheral arterial disease and its risk factors in type 2 diabetic outpatients.
Materials and Methods: It was a descriptive and analytical cross-sectional study, which included 146 diabetic out patients seen. Peripheral arterial disease (PAD) has been accessed using Ankle-Brachial Index and Arterial Doppler Ultrasound . PAD was defined by an ABI value ≤ 0.9 in either of the legs Data management and analysis were performed using Epi-Info software. A p value <0.05 was considered significant.
Results: The overall prevalence of peripheral arterial disease was 62.3%. Factors statistically associated with peripheral arterial disease were age (p=0.009), duration of diabetes greater than 10 years (p=0.006) and presence of peripheral neuropathy (p=0.0005).
Conclusion: The prevalence of peripheral arterial disease is high in type 2 diabetic outpatients. A systematic screening and suitable management should be done in order to prevent cardiovascular events often associated.
Keywords
Introduction
Diabetes is a growing public health concern worldwide. It is known to cause degenerative complications at both macrovascular and microvascular levels. Peripheral arterial disease (PAD) is one of its macrovascular complications. PAD affected in 2010 about 202 million people worldwide [1] with a prevalence that varies from 3 to 10% in the adult population [2]. In 2017 in Benin, this prevalence was 5.5% [3]. The risk of developing arterial disease is four times higher in diabetics than in the general population [4]. In a cross-sectional study in Benin, the prevalence of diabetic foot was 21.53% and arterial disease was found in 70.40% of cases in patients hospitalized for diabetic foot [5]. There have been a number of longitudinal studies involving PAD that have reported the increased risk of amputation in the patient with intermittent claudication; from 5% at five years the risk of amputation increases to 25% at one year in case of critical ischemia. Moreover, previous studies have established that PAD is associated with major cardiovascular events such as myocardial infarction and stroke. About 50% of patients with PAD have concomitant coronary involvement, and 20% have cerebrovascular involvement [6]. In other words, knowledge of the risk factors and screening for PAD in the diabetic patient should help to improve predictions of the cardiac and cerebral prognosis of the patient. The objective of the study was therefore to determine the prevalence and identify the risk factors for PAD in diabetic patients followed in the outpatient setting.
Materials and Methods
We conducted a cross-sectional, descriptive, analytical study that took place from November 18, 2018 to December 17, 2018 in Diabetic Care Center of Cotonou. Diabetic patients over 18 years of age and who gave consent were included.
Commodity sampling was performed and the sample size was calculated using Openepi software version 3.01. Considering p=22.07% (prevalence of PAD in Ivory Coast) [7], we obtained a sample size of 109, which we increased to 150 to reduce the effect of missing data.
Variables
The variables studied were :
- Peripheral arterial disease.
It was assessed in two ways:
- the Ankle-Brachial Index (ABI) : PAD was defined by an ABI value ≤ 9 in either of the legs. PAD was categorized as mild if 0.71≤ IABI≤ 0.90, moderate if 0.41<ABI≤ 0.70 and severe if ABI≤ 0.40 [8]. ABI was measured in a patient who was supine and at rest for at least 20 minutes. ABI was measured using Sonotrax® handheld Doppler with 8Hz probe according to standardized methods [9,10].
- Arterial Doppler ultrasound: arteriopathy was defined by the presence of one of the following conditions: atherosclerotic plaque, which may or may not be stenosed, or calcification. The arterial Doppler ultrasound was performed by a doctor specializing in medical imaging on a General Electric vivid 7 device using a 12Mhz linear probe.
Overall prevalence of PAD was defined by a ABI value ≤ 0.90 or by a presence of atherosclerotic plaque, calcification, or occlusion on arterial Doppler Ultrasound
- Socio-demographic: age, sex, profession,
- Related to medical and surgical history such as duration of diabetes, type of diabetes, current treatment of diabetes, history of diabetic foot, history of hypertension, history of stroke, history of myocardial ischemia, smoking
- Clinical -- Clinical variables collected were blood pressure, weight, height, intermittent claudication, lower limb sensation abnormality: paresthesia and dysesthesia, deep tendon reflexes abnormalities, reduced or absent pulses of the dorsalis pedis and posterior tibial arteries, presence of foot ulceration.
- Biological variables were A1C, lipid Variables were defined as follows :
- Hypertension was defined by a systolic blood pressure (SBP)≥140mmhg and/or its diastolic blood pressure (DBP) ≥ 90mmhg in a patient at rest for 10 minutes or by the presence of antihypertensive medication.
- Peripheral neuropathy was defined as the presence of at least one of the following abnormalities: paresthesia, dysesthesia, reduction of deep tendon reflexes of the lower limb
- Dyslipidemia was defined by any of the following conditions: LDL cholesterol ≥1g/L or Cholesterol Lowering Drugs being using, HDL cholesterol <0.40g/L in men and at 50g/L in women, total cholesterol >2g/L or Cholesterol Lowering Drugs being using, triglyceridemia >1.5g/L or Cholesterol Lowering Drugs being using.
Data management and analysis
Data management and analysis were performed using Epi-Info software version 3.5.1. The database was checked as the data was entered. At the end of the data entry process, the database was checked to assess the consistency and accuracy of the data recorded in relation to the survey forms. Descriptive data were generated for all variables. Frequencies were determined with their confidence intervals, means with their standard deviations. Proportions were compared using the Chi2 test (or Fisher's exact test depending on the caseï´¿ and means by using the t-test. A p value <0.05 was considered significant.
Results
A total of 146 adult subjects in whom ABI was measured and arterial Doppler ultra sound performed were included.
Study population characteristics
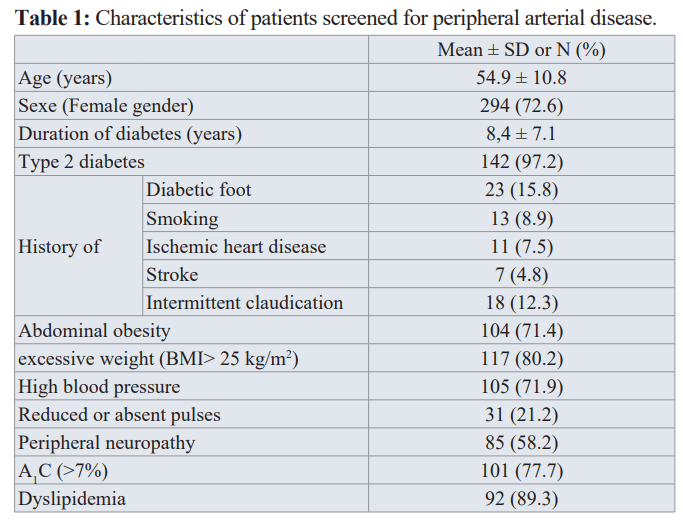
The mean age of the subjects was 54.9 years, women represented 72.6% of the study population and this population was largely dominated by type 2 diabetes (97.2%). The results, as shown in Table 1, indicate that high blood pessure, excessive weight and dyslipidemia were mainly represented
Prevalence of peripheral arterial disease
Among the 146 patients investigated, 65 had an ABI less than or equal to 0.90 in a pelvic limb, corresponding to a frequency of 44.5%, and 26 had typical arterial ultasonographic abnormalities and their ABI normal or greater than 1.30, hence the overall frequency of PAD disease 62.3% (91/146).
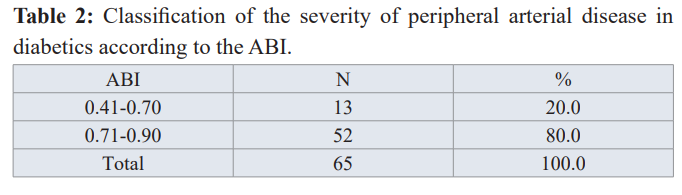
Regarding severity, 80% of the subjects had severe PAD as per the ABI (Table 2)
Risk factors for peripheral arterial disease
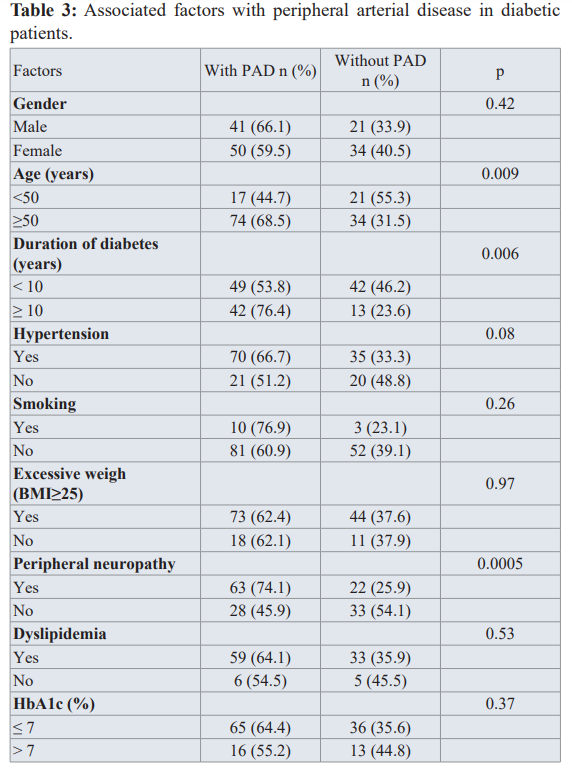
As Table 3 shows, factors statistically associated with peripheral arterial disease were age more than 50 years, duration of diabetes more than 10 years, and presence of peripheral neuropathy.
Discussion
We conducted a cross-sectional study of a total of 146 patients with diabetes. The first question in this study sought to determine the prevalence of peripheral arterial disease. The second question was to identify the associated factors with PAD.
The study found that the overall prevalence of PAD was 62.3%. These results agree with the findings of other studies, in which the prevalence of PAD is high in patients living with diabetes.
Indeed, Codjo et al. in Parakou in 2013 noted a prevalence of 41.9% [11], while Konin et al. found a prevalence of 22.07% in the diabetic population in 2014 in Ivory Coast [7] and Mwebaze et al. in Uganda in 2014 has reported a prevalence of 39% [12]. These results seem to differ from our findings. Actually these differences can be explained in part by the methods of screening used by each author. In this current study we combined ABI and arterial Doppler ultrasound of the lower limbs, whereas Codjo and Konin used only ABI
It is therefore not surprising that we found a higher frequency. Considering ABI alone in our study, we found a frequency of 44.5% which is similar to that reported by Codjo. There are, however, other possible explanations. Although all these studies have been conducted in diabetic populattions, there are some differences to point out. Our sample size seems to be small comparing with the previously cited authors (146 versus 308 in Konin’s study) and the frequencies of cardiovascular risk factors was higher in our study. Indeed, high blood pressure was present in 71.9% of cases, excessive weight in 80.2% of cases and dyslipidemia in 89.3% of cases whereas Konin and al. reported respectively 58.8%, 23.9% and 40.9% of hypertension, excessive weight and dyslipidemia.
Another important finding was that age, duration of diabetes and peripheral neuropathy were significantly associated with PAD. These results are in keeping with previous observational studies. These results are consistent with those of Amidou [3]. and Soyoye [13] who also showed an association between age and PAD. It’s known that PAD is uncommon in young people; its prevalence increases sharply with age and a possible explanation for this might be the fact that these patients are exposed to several cardiovascular risk factors over their lifetime. Moreover, the association of duration of diabetes and PAD is well established and have been shown by several reports [6,14,15]. Chronic hyperglycemia associated with other cardiovascular risk factors is at the origin of arthrosclerosis lesions that often appear within a period of 10 to 20 years.
In contrast to earlier findings, however, no evidence of association of PAD to dyslipidemia and smoking was detected. Smoking has been reported to be an important risk for PAD [16, 17]; however, smoking was not a significant factor in this study. The reason for this may be that few subjects (8.9%) ever smoked. Hence, the smaller number of smokers and the smaller size of our sample may explain the lack of association between smoking and PAD that we observed.
Conclusion
The results of this study show that the prevalence of peripheral arterial disease is high in type 2 diabetic outpatients. Age, duration of diabetes and peripheral neuropathy emerged as main factors associated this diabetes macrovascular complication. A systematic screening and suitable management should be done in order to prevent cardiovascular events often associated.
References
- Fowkes FGR, Rudan D, Rudan I, et al. Comparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: a systematic review and analysis. Lancet 2013; 382: 1329-1340.
- Aboyans V, Lacroix P, Laskar M. Prevalence of symptomatic and asymptomatic peripheral arterial disease in primary care Atherosclerosis. 2004; 175: 183-184.
- Amidou S, Houehanou YC, Houinato SD, et Epidemiology of lower extremity artery disease in a rural setting in Benin, West Africa: The TAHES study. International Journal of Cardiology. 2018; 267: 198-201.
- Lepantalo M, Apelqvist J, Setacci C, et Chapter V: Diabetic foot. Eur J Vasc Endovasc Surg. 2011; 42: S60-74.
- Kerekou Hode A, Djrolo F, Amoussou-guenou D. Aspects bacteriologiques du pied diabetique à cotonou. Journal de la Société de Biologie Clinique du Bénin. 2015; 022: 5-8.
- Aboyans V, Sevestre MA, Désormais I, et al. Épidémiologie de l’artériopathie des membres inférieurs. Presse Med. 2018; 47: 38-46.
- Konin C, Essam N’loo AS, Adoubi A, et Artériopathie des membres inférieurs du diabétique noir africain: aspects ultrasoniques et facteurs déterminants. Journal des Maladies Vasculaires. 2014; 39; 373-381.
- Nathaniel Clark. American Diabetes Association. Peripheral arterial disease in people with diabetes a consensus Diabetes Care. 2003; 26: 3333-3341.
- Meijer WT, Grobbee DE, Hunink MG, et al. Determinants of peripheral arterial disease in the elderly: the Rotterdam study. Arch Intern Med. 2000; 160: 2934-2938.
- Curb JD, Masaki K, Rodriguez BL, et al. Peripheral artery disease and cardiovascular risk factors in the elderly. The Honolulu Heart Arterioscler Thromb Vasc Biol. 1996; 16: 1495-1500.
- Codjo HL, Adoukonou TA, Wanvoegbè A, et Prévalence de l’artériopathie oblitérante des membres inférieurs et facteurs associés chez les diabétiques suivis en milieu hospitalier à Parakou en 2013. Annales de Cardiologie et d’Angéiologie. 2016; 65: 260-264.
- Mwebaze RM, Kibirige D. Peripheral arterial disease among adult diabetic patients attending a large outpatient diabetic clinic at a national referral hospital in Uganda: a descriptive cross sectional PLoS ONE. 2014; 9: e105211.
- Soyoye DO, Ikem RT, Kolawole BA, et al. Prevalence and Correlates of Peripheral Arterial Disease in Nigerians with Type 2 Adv Med. 2016; 2016: 3529419.
- Got I, Creton C, Guerci B, et al. Artériopathie oblitérante des membres inférieurs chez le diabétique. Sang Thromb Vaiss. 1996; 8: 221-228.
- Trevor J, Orchard SD, Raelene EM, et Prevalence of complications in IDDM by sex and duration. Diabetes. 1990; 39: 1116-1124.
- Selvin E, Erlinger TP. Prevalence of and risk factors for peripheral arterial disease in the United States: results from the National Health and Nutrition Examination Survey, 1999– Circulation. 2004; 110: 738-743.
- Hirsch AT, Criqui MH, Treat-Jacobson D, et al. Peripheral arterial disease detection, awareness, and treatment in primary The Journal of the American Medical Association. 2001; 286: 1317-1324.