Prospective Evaluation of Factors Associated with Arteriovenous Fistula Primary Failure and Complications in Hemodialysis Patients: A Single Center-Study
Author'(s): Ismail Al-Shameri MS1*, Gamal KhudaBux MD2, and Abudar Al-Ganadi Phd1
1Department of General & Vascular Surgery, Authority of Althawra Hospital, Taiz University Factuality of medicine, Taiz, Yemen.
2Department of General & Vascular Surgery, AL-Gamhoria Modern General Hospital, Aden University Factuality of medicine, Aden, Yemen.
*Correspondence:
Ismail Al-Shameri, Authority of Althawra Hospital, Factuality of medicine, Taiz University, Taiz-Yemen, Tel: 00967-772228396.
Received: 24 March 2021; Accepted: 06 May 2021
Citation: Al-Shameri I, KhudaBux G, Al-Ganadi A. Prospective Evaluation of Factors Associated with Arteriovenous Fistula Primary Failure and Complications in Hemodialysis Patients: A Single Center-Study. Cardiol Vasc Res. 2021; 5(3): 1-7.
Abstract
Aim: The objective of this study was to analysis factors affecting arteriovenous fistula patency, to improve access outcome.
Methods& Patients: Patients (n=290) were enrolled in our prospective observational study. Demographic, clinical, and operative variables were compared between those with and without NAVF function loss. In addition, we evaluated the distribution and complication of NAVF and its association with different factors. All statistical analyses were performed with the use of appropriate SPSS software package, version 24.0.
Results: We found 96.5% (n=280) of patients had NAVFs, among them 67.9% (190/280) of patients had upper NAVFs, followed by lower NAVFs 32.1% 90/280), while 3.4% (10/290) of patients had depended on a cuff catheter. The most frequent complication post NAVF creation was thrombosis (11.4%), followed by noninfectious fluid collections (9.3%), infection (6.4%), Limp edema (4.3%), Aneurysmal degeneration (3.2%), arterial steal syndrome (2.5%) and venous hypertension (1.8%). History of dialysis catheter used AVF location and absent intraoperative thrill were independently associated with loss of NAVF primary patency. There was a statistically significant increase in the number of steal syndrome in patients who had diabetes mellitus (P value= 0.021) and in patients who had age >65 years (P value 0.002), while female gender was not (P value= 0.122). History of catheter used (P = 0.02), previous AVF procedure (P= 0.01), and present of non-infection fluid (P = 0.00) were found significantly increase the infection rate of NAVF.
Conclusions: Identifying risk factors affecting AVF patency is crucial. Early and timely treating complications post AVF is essential for proper management and maturation.
Keywords
Introduction
Long-term vascular access patency has resulted in the long-life survival of thousands of patients with end-stage renal disease (ESRD) on maintenance hemodialysis (HD) [1-3] AVFs have higher primary patency, lower risk of infection, higher durability, lower mortality, [4-6] and fewer required interventions [7] when compared with prosthetic grafts and TDCs. However, AVFs have a high rate of no maturation (20–50%), [8-11] which likely accounts for the fact that at 6 months after initiating HD, 55% of patients continue to be dialyzed with tunneled dialysis catheter (TDC) [12-17].
Studies have found that fistula complications are associated with morbidity, mortality, and a high economic burden [18,19]. And it was reported that early detection and treatment of these complications can prevent more severe conditions and consequently save additional costs and reduce hospitalization periods [20].
Despite the burden of vascular access complications on patients and the healthcare system, there remains a poor consensus on the incidence risk and factors associated with increased rates of fistula complications. The wide variation in complication event rates across studies is attributed to variation in definitions, inconsistent reporting, and differences in patient populations [21].
Variables associated with fistula complications; patient comorbidities, vessel features, surgeon experience, or ability of nursing cannulation was generally not reported in studies. Overall, due partly to poor quality studies, significant heterogeneity of study populations, and inconsistent definitions, we found marked variability in complication rates. The need to standardize reporting is urgent [21]. For that, the main aim of this research was to studies the distribution of different variable age, gender, and location of AVF (wrist or elbow AVF) with NAVF patency loss. The study also looked for any predisposing risk factors and complications of AVF to improve outcomes.
Method and Patients
This prospectively study was conducted at Department of vascular surgery, Authority of Althawra Hospital in Taiz-Yemen, from 1st June 2018 to 31th July 2020. All patients with ESRD, who refer for creation AVF were include in this study. 280 Two-hundred eighty patients were enrolled in the study. Details Demographic, Clinical, and preoperative dialysis variables were obtained for every patient. Allen’s test and arterial pulses (i.e. axillary, brachial, radial, and ulnar) were examined. Patients with visible veins on the clinical examination were directly scheduled for AVF creation while patients with non-visible veins were underwent venous mapping by ultrasonography (US) before being scheduled for surgery [22]. The distal part of the non-dominant extremity was selected as priority anatomical site, whenever possible [23].
After determination of the appropriate limb for surgery, the procedure was done under local anesthesia by end vein to side artery parachute vascular anastomosis technique in the operation theatre. We divided our patient in tow groups by age, gender and location of AVF with aim to study the associated of this variable with fistula complications.
The access was considered mature if its successful use for six consecutive sessions of HD Outcome Parameter. This definition for the evaluation of AVF maturation has been validated in the literature in several previous studies [24-26]. Primary failure define as an AVF that has never been usable for dialysis or that fails within three months of use [27,28]. In our study, primary patency of AVF at immediate, 30 and 90 days, and at 6 months had been measured.
All patient discharges on operation day with oral antibiotics and analgesics for three days. Patients were instructed to start hand exercise on the second postoperative day with ball. Skin stitches ware removed on the 10th post-operative day. The follow up performed on an outpatient basis, at 7th and 14th day then at 4- and 6-weeks post-operative, where fistula was released to puncture for HD. Periodic follow up was performed for at least 24 months. In follow up visit, all patients were be evaluated for the presence or absence thrill or complications i.e. seroma, hematoma, infection, bleeding, thrombosis, aneurysms, steal syndrome and venous hypertension.
Study analysis
Data collection and analysis conducted using SPSS (IBM SPSS Statistics 24.0). Initially, descriptive analysis of complication and variables predominantly was analyzed as frequencies, tables and percentages for categorical variable and mean and SD for continuous variable. The association between variable and complication were analyzed by the Chi-square (x2) or fisher test for the categorical variable and unpaired Student's t-test for the continuous variable with the corresponding 95% confidence interval (CI). P-values ≤ 0.05 were considered statistically significant.
Result
From June 1/ 2018, through July 31/ 2019, the study included a total 280 patients had native AVF with end-to-side anastomotic (parachute) technique. Among those, 67.9% (190/280) of patients had upper (elbow) NAVFs, followed by lower (wrist) NAVFs 32.1% (90/280). Most common comorbidity in this study was hypertension in 202 (72.1%), followed by diabetes in 79 (28.2%).
Distribution of NAVFs with gender in our patients 167 (59.6%) in men while 113 (40.4%) in female patients with male to female ratio of 1.5:1. The main age of patients was (48.64 ± 17.15); among those, 216 (77.1%) patients was less than 65years, and 64 (22.9%) patients were more than 65 years old. We find that, age and gender were not statistically association with AVF complication.
During the study period, the most frequently complication post NAVF creation was thrombosis (11.4%), followed by noninfectious fluid collections (9.3%), infection (6.4%), limp edema (4.3%), aneurysmal degeneration (3.2%), arterial steal syndrome (2.5%) and venous hypertension (1.8%) Figure 1.
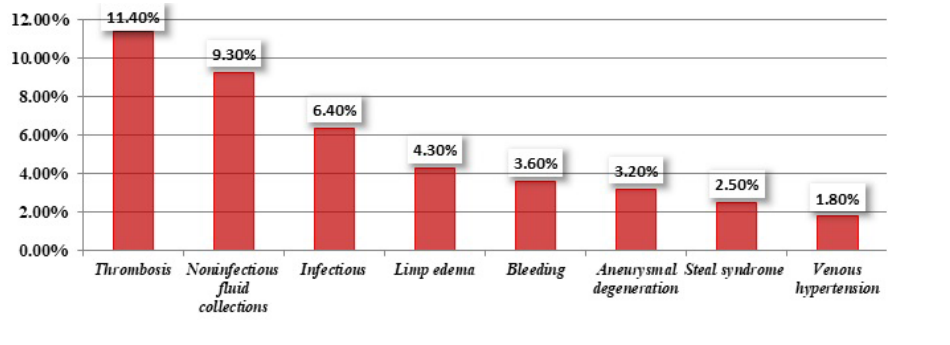
Figure 1: Complication of Native Arteriovenous Fistula in our study.
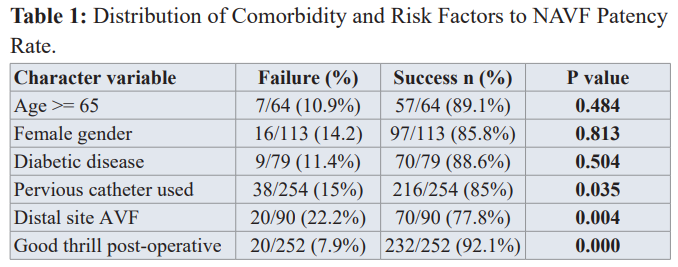
We studied the relationship between different patients’ characteristics and comorbidities with primary failure in our patients using the appropriate statistical tests as outlined above: we noted that, there were no statistically different between age, gender, diabetic disease, HTN and PAD and the patency of AVF. However there statistically influence of pervious dialysis catheter used and primary loss of AVF patency (P value = 0.035).
The site of creation AVF was found statistically influence the outcome patency in our study; as 90 fistulas created distally around the wrist, 20 (22.2%) failed and70 (77.8%) matured, compared to 18/190 (9.5%) and 172/190 (90.5%) of those placed in the arm respectively (P = 0.004). Moreover, good thrill intraoperative was significantly associated with a more favorable outcome as only 20/252 (7.9%) created AVFs had failed compared to 18/28 AVFs were failed in those patients who have not good intra-operative thrill (P = 0.000) Table 1.
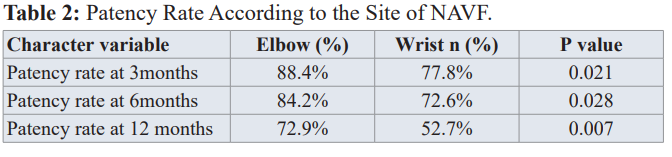
There was significant difference in patency rate between the two groups (elbow vs. wrist) (p<0.05) (Table 2). The patency rate during 3,6,12 months in the wrist group was 77.8%, 72.6%, and 52.7%, respectively; and in elbow group, it was 88.4%, 84.2% and 72.9%, respectively.
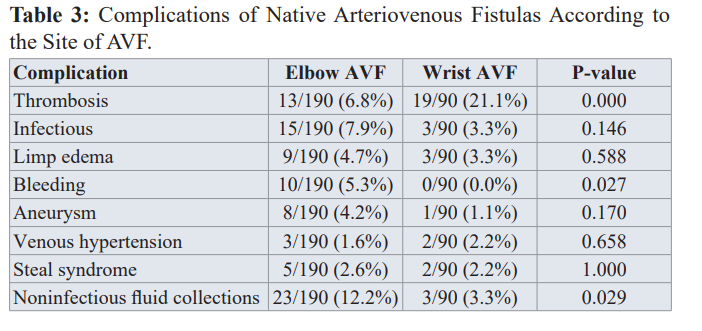
Of the patients, 11.1% (32/280) had an NAVF complicated by thrombosis, 59.37% (19/32) of those occurred at the distal (wrist) group and 40.6% (13/32) occurred at the proximal sit (elbow group). This deferent was found statistically significant (P value = 0.000). Bleeding was more common in the elbow group 10/190 (5.3%) than in the wrist group 0/90 (0.0%) (P value = 0.027). Aneurysm was more common in the elbow group 8/9 (88.9%) than in the wrist group 1/90 (1.1%) but this different was statistically not significant (P value = 0.170). There were no differences in other complications such as venous hypertension, infection, noninfectious fluid collections and arterial steal syndrome between the two groups. Table 3.
In our study, there was a statistically significant increase in the number of steal syndrome in patients who had diabetes mellitus (P value = 0.021) and in patients who had age >65 years (P value 0.002), while female gender was not (P value = 0.122).
Discussion
The mean age of patients with ESRD undergoing AVF in our patients was (48.64 ± 17.15y), which was similar or close to other studies reported in Iran, India and Nigeria [29-31].
However, the mean age in developed countries was one or two decades older [26,32-34]. These outcomes reflect inequalities of healthcare system in our country (especially with current war) than others.
The influence of age on the patency of AVF is still controversial. A review of literature by Smith et al. [35] (2012) on the factors influencing patency of AVF showed an increase of access failure in the elderly population [35] In a meta-analysis of 2007, Lazarides et al. [36] showed a significant difference in secondary patency rates between the elderly and younger patients at 12 and 24 months with odds ratios (ORs) of 1.525 (P = 0.001) and 1.357 (P = 0.019) [36]. On other hand, a literature review by Al-Jaishi et al. [37] found that age had no effect on primary patency. Our results are similar to those of Olsha et al. [38], Bashar et al. [26], and Chan et al. [33] who’s reported that, age did not seem to influence the primary patency. Overall, age as an isolated variable should not greatly affect access decision with consider good preoperative preparation.
We did not find a significant effect of gender on AVF patency. In a literature review of 2012, Smith et al. [35] also found the same result. Similar finding was also found by Olsha et al. [38] from Turkey and Chan C. et al. [33] from USA. On the other hand, there’re studies found significant differences in outcomes of AVF creation when comparing male and female [26,31]. In one study, Peterson et al. [39] report that, female was at greater risk for failure of the AVF to mature compared with male in spite of preoperative vascular mapping (hazard ratio 2.42, 95% CI 1.32-4.45) [39]. The reasons for these differences are not clear. It has been suggested that female has smaller vessels [31,40] These discrepancies suggest that functional properties of the vessels may contribute to fistula failure to mature even when the diameters are adequate [39].
Factors adversely affecting AVF patency in ESRD patients reported include diabetes [41]. We reported that, diabetic was found in 79 (28.2%) of our patients while Elsharawy et al. [42] and Susan et al. [43] had been report higher percent than us (40%), (43%) respectively. In contrast to previous studies [33,41,44,45] in which there is significant difference noticed between patients with diabetes and risk of loss of primary patency, our results indicated that patients with diabetes had no effect on AVF patency rates. Our results are similar to those of Maharaj et al. [47] and Olsha et al. [38] and suggest that patients with diabetes should not be a limiting factor when determining candidacy for AVF creation. In our study, HTN 164 (74.5%) was most common comorbidity. Similar finding, was report by Susan J. et al. [43] (73.7%) from India, while lower percentage had reported in other studies [31,48]. HTN had no effect on AVF patency in our study (p value = 0.182).
Unfortunately, in our practice, many patients notice to have venous lesion of upper limbs due to repeated venous access and phlebotomy. This, adversely affect the available peripheral and central venous routes so that, more proximal vein was used for AVF creation. This issue had recognized clearly in our study, as about fifty presents (135 patients) of our series had their first native AVF creation in proximal site.
In contrast to previous studies [26,30-32,49,43], in which radiocephalic fistula was most common type, our results notice that brachiocephalic (50%) was the most common type AVF in our patients, followed by radiocephalic type (32%). Similar observation was also reported by Yabanoglu et al. [50] from Turkey, and Shan et al. [51] from Nepal and Chan et al. [33] from USA. This result may be explained by multiples factors include destruction of veins by repeated venipuncture before fistula creation, poor technique, inadequate information available to patients and health worker on pre dialysis care.
Complications of AVF adversely affect quality of life and survival of ESRD patients [52] Despite the burden of vascular access complications on patients and the healthcare system, there remains a poor consensus on the incidence risk and factors associated with increased rates of fistula complications [21]. The most common complications after AVF creation is thrombosis. It was reported in previous studies with rate of (3-14.5%) [29,53,54]. Thrombosis of NAVF was the most common complication 30 (13%) in our patients. Similar finding was reported by Yu, Q. et al. [55] with thrombosis rate 13.86 %. Other studies reported higher thrombosis rate; 33% by Dekhaiya et al. [29] in India 2016, and 27% by Susan et al. [43] in India 2018. However, lower thrombosis rate war reported; 10% by Gjorgjievski et al. [32] in Macedonia 2019, and 7.5% by Salako et al. [30] in Nigeria 2018.
In a systematic review and meta-analysis of 2014, Al-Jaishi et al. [37] showed a statistically significant difference in primary patency loss between AVF locations (lower 28% vs. upper arm 20%) at 1 year (P = 0.001), but not at 2 years (P = 0.3). Monroy-Cuadros et al. [45] in Canada found that, the location of forearm AVF (OR 4.0, P < 0.001) was independently associated with loss of primary patency. We had similar observation; there was significant difference in primary patency loss and the location of AVF (elbow vs. wrist) at 3,6,12 months (P = 0.021), (P = 0.028), and (P = 0.007). These observed differences may be related to smaller size of the vessels at distal location; Poiseuille’s law physiologically supports the presence of lower arterial blood flow in the forearm location. In upper arm fistulas, the diameter of the vessels is expected to be bigger than in the forearm, and more significant roles for systemic aspects such as cardiac output and blood pressure can be expected [45,56,57].
Infection is the second most frequent cause of vascular access site loss, and it is frequent complication of AVF surgery requiring hospitalization. Moreover, it’s ranks second to cardiovascular disease as a cause of death in HD patients [58-60]. In our study infection was (7.4%) the third common complication after thrombosis (13%) and noninfectious fluid (10%). Similarly, infection rate was observed 7.4% by Schinstock et al. [61] in USA 2011. However, Aljuaid et al. [48] in Saudi Arabia 2020 reported higher infection rate 20%. In other hand, lower infection rate was reported; 3.5% by Dekhaiya et al. [29] in India 2016, 5.1% by Susan et al. [43] in India 2018, and 3.75% by Salako et al. [30] in Nigeria 2018. In our study we observed a statistically significant increase in the infection rate as the proportion of patients with history of catheter used (P = 0.02), previous AVF procedure (P = 0.01), and present of non-infection fluid (P = 0.00) increased. Therefore, these results support that these patients should be routinely monitored for present of infection post AVF creation.
In the series, steal syndrome were observed; 16.1% by Aljuaid et al. [48] in Saudi Arabia 2020, 5.1% by Schinstock et al. [61] in
USA 2011 and 3.3% Dekhaiya et al. [29] in India 2016. However, in our study this rate was (2.5%). In other studies were reported lower rate of steal syndrome; 1.1% by Alhassan et al. [62] in Nigeria 2013.In contrast to previous studies [63-69] in which, there are multiple factors for developed steal syndrome that include female gender, advanced age, DM, PAD [63-69]. Age >65 years (P value 0.002) and patient with diabetic disease (P value= 0.021) were found statistically related to developed steal syndrome complication. While female gender (P = 0.122) was not. Our results are similar to those of Rocha et al. [68] in Portugal 2012. So that, these higher risk patients should be counseled preoperatively, their operative plans should be designed to reduce the risk of hand ischemia, and they should be observed closely. The management of steal syndrome in our study was done by DRIL procedure in 3 patients (Figure 2) while the 4 patients was managed by ligation of AVF and permanent tunneled catheters.
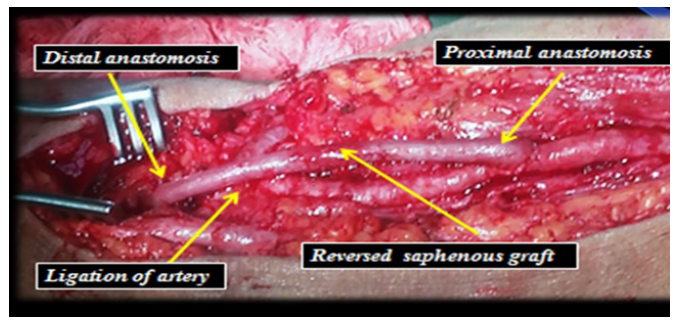
Figure 2: Intraoperative Photo Show DRILE Procedure for ESRD Patient with AVF Complicated by Grade IV Steal Syndrome
A previous review documented an aneurysm rate between 5% and 6% [70]. It was found in nine patients (3.9 %) of our patients. Nearly similar results 4.2% found by Susan et al. [43] in India 2018 and 3.5% by Alhassan et al. [62] in Nigeria 2013. However, lower result was report 1.3% by Dekhaiya et al. [29] in India 2016, 2.4% by Schinstock et al. [61] in USA 2011 and 3.2 by Shahnawaz et al. [49] in Pakistan 2012. In other hand, Aljuaid et al. [48] in Saudi Arabia 2020, by Yu, Q. et al. [55] 2011 reported higher rate of AVF aneurysm (25%), (12.2%) respectively.
Aneurysms/pseudoaneurysms that require urgent evaluation to prevent rupture include the presence of a non-healing eschar, spontaneous bleeding from access sites, and rapid expansion in size of the aneurysm [71]. In our study, management of those nine patients were; one patient managed by aneurysmoplasty, one patient by resection aneurysm part with interposition vein graft repair and the remain seven were managed by resection of aneurysm and creation new AVF.
In the present study, venous hypertension was developed in five patients (1.8%). The most common cause of venous hypertension is central stenosis secondary to placement of central venous catheters and devices [72] Similar noted was observed in our study, where there was statistically related between pervious central dialysis catheter used and venous hypertension (p=0.001).
Conclusion
The distribution of complications of AVF according to location showed that thrombosis more common in distal (Wrist) AVF, while bleeding was more in elbow group. History of dialysis catheter used AVF location and absent intraoperative thrill were independently associated with decrease patency rate in our patient. Infection occurred most commonly in patients with history of previous AVF, dialysis catheter, or present of non-infection fluid. Additionally, steal syndrome was predominantly seen on patients age > 65 and patient with diabetic disease.
Acknowledgements
The authors would like to acknowledge and thank all of the surgeons, nurses, and medical personnel who worked selflessly to care for these patients.
References
- Santoro D, Benedetto F, Mondello P, et Vascular access for hemodialysis: Current perspectives. Int J Nephrol Renovasc Dis. 2014; 7: 281-294.
- Rowse JW, Kirksey L. Surgical Approach to Hemodialysis Access. Semin Intervent Radiol. 2016; 33: 21-24.
- Jennings WC, Taubman KE. Alternative autogenous arteriovenous hemodialysis access Semin Vasc Surg. 2011; 24: 72-81.
- Ocak G, Halbesma N, Le Cessie S, et al. Haemodialysis catheters increase mortality as compared to arteriovenous accesses especially in elderly patients. Nephrol Dial Transplant. 2011; 26: 2611-2617.
- Malas MB, Canner JK, Hicks CW, et al. Trends in incident hemodialysis access and mortality. JAMA Surg. 2015; 150: 441-448.
- Ocak G, Rotmans JI, Vossen CY, et Type of arteriovenous vascular access and association with patency and mortality. BMC Nephrol. 2013; 14: 79.
- Lok CE, Sontrop JM, Tomlinson G, et Cumulative patency of contemporary fistulas versus grafts (2000-2010). Clin J Am Soc Nephrol. 2013; 8: 810-818.
- Vassalotti JA, Jennings WC, Beathard GA, et Fistula First Breakthrough Initiative: Targeting Catheter Last in Fistula First. Semin Dial. 2012; 25: 303-310.
- Allon M, Lockhart ME, Lilly RZ, et Effect of preoperative sonographic mapping on vascular access outcomes in hemodialysis patients. Kidney Int. 2001; 60: 2013-2020.
- Miller PE, Tolwani A, Luscy CP, et Predictors of adequacy of arteriovenous fistulas in hemodialysis patients. Sznitman J, ed. Kidney Int. 1999; 56: 275-280.
- Lynch JR, Mohan S, McClellan WM. Achieving the goal: Results from the Fistula First Breakthrough Initiative. Curr Opin Nephrol Hypertens. 2011; 20: 583-592.
- Saran R, Li Y, Robinson B, et US Renal Data System 2014 Annual Data Report: Epidemiology of Kidney Disease in the United States. Am J Kidney Dis. 2015; 66: A7.
- https://www.kidney.org/professionals/guidelines
- https://www.kidney.org/patients/pfc/DialysisEducation
- Schmidt RJ, Goldman RS, Germain M. Pursuing permanent hemodialysis vascular access in patients with a poor prognosis: Juxtaposing potential benefit and harm. Am J Kidney Dis. 2012; 60: 1023-1031.
- Tan TW, Farber Brachial-basilic autogenous access. Semin Vasc Surg. 2011; 24: 63-71.
- Kinney 2005 Annual Report: ESRD Clinical Performance Measures Project. Am J Kidney Dis. 2006; 48.
- Manns B, Tonelli M, Yilmaz S, et al. Establishment and Maintenance of Vascular Access in Incident Hemodialysis Patients: A Prospective Cost Analysis. J Am Soc Nephrol. 2005; 16: 201-209.
- Ravani P, Palmer SC, Oliver MJ, et al. Associations between Hemodialysis Access Type and Clinical Outcomes: A Systematic Review. J Am Soc Nephrol. 2013; 24: 465-473.
- Rosas SE, Feldman HI. Synthetic Vascular Hemodialysis Access Versus Native Arteriovenous Ann Surg. 2012; 255: 181-186.
- Al-Jaishi AA, Liu AR, Lok CE, et al. Complications of the Arteriovenous Fistula: A Systematic Review. J Am Soc Nephrol. 2017; 28: 1839-1850.
- Lee K, Chong T, Goh N, et al. Outcomes of Arteriovenous Fistula (AVF) Creation, Effect of Preoperative vein mapping and Predictors of Fistula Success in Incident Hemodialysis Patients–A Single-center Experience. Nephrology. (Carlton). 2017; 22: 382-387.
- Adequacy H, Adequacy PD, Access 2006 Updates Clinical Practice Guidelines. Blood Pressure. 2006.
- Bhalodia R, Allon M, Hawxby AM, et al. Comparison of Radiocephalic Fistulas Placed in the Proximal Forearm and in the Wrist. Semin Dial. 2011; 24: 355-357.
- Renaud CJ, Pei JH, Lee EJC, et Comparative outcomes of primary autogenous fistulas in elderly, multiethnic Asian hemodialysis patients. J Vasc Surg. 2012; 56: 433-439.
- Bashar K, Zafar A, Elsheikh S, et Predictive Parameters of Arteriovenous Fistula Functional Maturation in a Population of Patients with End-Stage Renal Disease. James LR, ed. PLoS One. 2015; 10: 1-15.
- Asif A, Roy-Chaudhury P, Beathard Early arteriovenous fistula failure: a logical proposal for when and how to intervene. Clin J Am Soc Nephrol. 2006; 1: 332-339.
- Beathard GA, Arnold P, Jackson J, et Physician Operators Forum of RMS Lifeline. Aggressive treatment of early fistula failure. Kidney Int. 2003; 64: 1487-1494.
- Dekhaiya FA, Hathila TN, Doshi SA, et al. A prospective study of arteriovenous fistula creation in chronic renal failure patients in Bhavnagar, Gujarat, western India. 2016; 5: 5-9.
- Salako AA, Badmus TA, Igbokwe MC, et Experience with arteriovenous fistula creation for maintenance hemodialysis in a tertiary hospital in South-Western Nigeria. In: Saudi Journal of Kidney Diseases and Transplantation : An Official Publication of the Saudi Center for Organ Transplantation, Saudi Arabia. 2018; 29: 924-929.
- Gh K, Mhs M, H R, et al. Primary patency rate of native AV fistula: Long-term follow up. Int J Clin Exp Med. 2012; 5: 173-178.
- Gjorgjievski N, Dzekova-Vidimliski P, Gerasimovska V, et al. Primary Failure of the Arteriovenous Fistula in Patients with Chronic Kidney Disease Stage 4/5. Open Access Maced J Med Sci. 2019; 7: 1782-1787.
- Chan C, Ochoa CJ, Katz SG, et Prognostic Factors for Arteriovenous Fistula Maturation. Ann Vasc Surg. 2018: 1-4.
- Badawy DA, Mowafi HS, Al-Mousa HH. Surveillance of dialysis events: 12-Month experience at five outpatient adult hemodialysis centers in J Infect Public Health. 2014; 7: 386-391.
- Smith GE, Gohil R, Chetter IC. Factors affecting the patency of arteriovenous fistulas for dialysis access. J Vasc Surg. 2012; 55: 849-855.
- Lazarides MK, Georgiadis GS, Antoniou GA, et al. A meta- analysis of dialysis access outcome in elderly J Vasc Surg. 2007; 45: 420-426.
- Al-Jaishi AA, Oliver MJ, Thomas SM, et Patency rates of the arteriovenous fistula for hemodialysis: A systematic review and meta-analysis. Am J Kidney Dis. 2014; 63: 464-478.
- Olsha O, Hijazi J, Goldin I, et al. Vascular access in hemodialysis patients older than 80 J Vasc Surg. 2015; 61: 177-183.
- Peterson WJ, Barker J, Allon M. Disparities in fistula maturation persist despite preoperative vascular mapping. Clin J Am Soc Nephrol. 2008; 3: 437-441.
- Gibson KD, Gillen DL, Caps MT, et Vascular access survival and incidence of revisions: A comparison of prosthetic grafts, simple autogenous fistulas, and venous transposition fistulas from the United States Renal Data System Dialysis Morbidity and Mortality Study. J Vasc Surg. 2001; 34: 694-700.
- Iyem H. Early follow-up results of arteriovenous fistulae created for hemodialysis. Vasc Health Risk Manag. 2011; 7: 321-325.
- Elsharawy Prospective Evaluation of Factors Associated with Early Failure of Arteriovenous Fistulae in Hemodialysis Patients. Vascular. 2006; 14: 70-74.
- Johny S, Pawar Complications of arteriovenous fistula for haemodialysis access. Int Surg J. 2018; 5: 439.
- da Cruz RN, Retzlaff G, Gomes RZ, et al. Influência do diabetes mellitus sobre a perviedade da fistula arteriovenosa para hemodiálise. J Vasc Bras. 2015; 14: 217-223.
- Monroy-Cuadros M, Yilmaz S, Salazar-Bañuelos A, et al. Risk factors associated with patency loss of hemodialysis vascular access within 6 months. Clin J Am Soc Nephrol. 2010; 5: 1787-1792.
- Wolowczyk L, Williams AJ, Donovan KL, et The snuffbox arteriovenous fistula for vascular access. Eur J Vasc Endovasc Surg. 2000; 19: 70-76.
- Maharaj D, Ramdass MJ, Baksh R, et Distal-to-Snuffbox Arteriovenous Fistula. Tobago Int J Angiol. 2018; 27: 227-231.
- Chowdhury S, Chakraborty P pratim. Complications of arteriovenous fistula in dialysis patients: Incidence and risk factors in Taif city, KSA. J Fam Med Prim Care. 2017; 6: 169-170.
- Shahnawaz, Ali S, Shahzad I, Baloch MU. Arterio venous fistula experience at a tertiary care hospital in Pakistan. Pakistan J Med Sci. 2012; 29: 161-165.
- Yabanoglu H, Kus M, Arer IM, et Comparison of the Early-Term Complications and Patency Rates of the Standard (Parachute) and Diamond-Shaped End-To-Side Anastomosis Techniques in Arteriovenous Fistulas Created for Hemodialysis. J Coll Physicians Surg Pakistan. 2018; 28: 597-602.
- Shah S, Maharjan N, Chapagain D, et Arterio-Venous (AV) Fistula: Surgical outcome in College of Medical Sciences Teaching Hospital, Bharatpur, Chitwan. J Coll Med Sci. 2013; 8: 1-6.
- Acipayam M, Zor H, Yildiz GD, et al. Hemodiyaliz amaçli açilan arteriyovenöz fistüllerin açikligi üzerine etkili faktörler: Üç yillik sonuçlarin degerlendirilmesi. Turkish J Thorac Cardiovasc Surg. 2013; 21: 59-62.
- Brescia MJ, Cimino JE, Appel K, et Chronic hemodialysis using venipuncture and a surgically created arteriovenous fistula. N Engl J Med. 1966; 275: 1089-1092.
- Meyer F, Müller JS, Bürger T, et al. Experiences with Ambulatory Arteriovenous Shunt Surgery. A Cost-Benefit Analysis. Chirurg. 2002; 73: 274-278.
- Yu Q, Yu H, Huang J, et al. Distribution and complications of native arteriovenous fistulas in maintenance hemodialysis patients: A single-center J Nephrol. 2011; 24: 597-603.
- Lok CE. Fistula First Initiative: Advantages and Pitfalls History and Necessity for Fistula Clin J Am Soc Nephrol. 2007; 2: 1043-1053.
- Beathard GA, Dillavou ED, Berns JS, et Patient evaluation prior to placement of hemodialysis arteriovenous access. 2020.
- Stevenson KB, Hannah EL, Lowder CA, et al. Epidemiology of hemodialysis vascular access infections from longitudinal infection surveillance data: Predicting the impact of NKF- DOQI clinical practice guidelines for vascular access. Am J Kidney Dis. 2002; 39: 549-555.
- Mailloux LU, Bellucci AG, Wilkes BM, et al. Mortality in dialysis patients: analysis of the causes of Am J Kidney Dis. 1991; 18: 326-335.
- Butterly DW, Schwab Dialysis access infections. Curr Opin Nephrol Hypertens. 2000; 9: 631-635.
- Schinstock CA, Albright RC, Williams AW, et al. Outcomes of Arteriovenous Fistula Creation after the Fistula First Initiative. Clin J Am Soc Nephrol. 2011; 6: 1996-2002.
- Alhassan S, Adamu B, Abdu A, et al. Outcome and complications of permanent hemodialysis vascular access in Nigerians: A single centre experience. Ann Afr Med. 2013; 12: 127.
- Malik J, Tuka V, Kasalova Z, et Understanding the dialysis access steal syndrome. A review of the etiologies, diagnosis, prevention and treatment strategies. J Vasc Access. 2008; 9: 155-166.
- Davidson D, Louridas G, Guzman R, et al. Steal syndrome complicating upper extremity hemoaccess procedures: Incidence and risk factors. Can J Surg. 2003; 46: 408-412.
- Yu SH, Cook PR, Canty TG, et Hemodialysis-Related Steal Syndrome: Predictive Factors and Response to Treatment with the Distal Revascularization-Interval Ligation Procedure. Ann Vasc Surg. 2008; 22: 210-214.
- Morsy AH, Kulbaski M, Chen C, et al. Incidence and characteristics of patients with hand ischemia after a hemodialysis access procedure. In: Journal of Surgical Research. 1998; 74: 8-10.
- Huber TS, Larive B, Imrey PB, et al. Access-related hand ischemia and the Hemodialysis Fistula Maturation Study. In: Journal of Vascular Surgery. 2016; 64: 1050-1058.
- Rocha A, Silva F, Queirós J, et Predictors of steal syndrome in hemodialysis patients. Hemodial Int. 2012; 16: 539-544.
- Kudlaty EA, Kendrick DE, Allemang MT, et al. Upper Extremity Steal Syndrome Is Associated with Atherosclerotic Burden and Access Configuration. Ann Vasc Surg. 2016; 35: 82-87.
- Radojica Stolic. Most important chronic complications of arteriovenous fistulas for hemodialysis. Med Princ Pr. 2013; 22: 220-228.
- Navuluri R, Regalado S. The KDOQI 2006 Vascular Access Update and Fistula First Program Synopsis. Semin Intervent Radiol. 2009; 26: 122-124.
- Agarwal AK, Patel BM Central vein stenosis: A nephrologist’s perspective. Semin Dial. 2007; 20: 53-56.