Recognizing the Differences to Reduce Disparities in Cardiovascular Disease Impact Among African Descendants
Author(s): Felix Nunura FACC*
1Division of Cardiovascular Medicine, Heart Institute of the Caribbean (HIC) and the Heart Hospital, Kingston, Jamaica.
*Correspondence:
Dr. Felix Nunura, FACC, Heart Institute of the Caribbean, 23 Balmoral Avenue, Kingston 10, Jamaica.
Received: 20 April 2020; Accepted: 15 May 2020
Citation: Nunura Felix. Recognizing the Differences to Reduce Disparities in Cardiovascular Disease Impact Among African Descendants. Cardiol Vasc Res. 2020; 4(2): 1-5.
Abstract
There are important differences in morbidity and mortality from cardiovascular diseases across ethnic groups, namely: Hypertension, Coronary artery disease, Heart Failure and cardiovascular risk factors, disease presentation and treatment response. To recognize this is particularly important in order to understand the nature of cardiovascular disease health disparities among African descendant (African American/Afro-Caribbean origin) populations as is also critically important for cardiovascular professionals to be aware of their role in perpetuating disparities, and consider the race and ethnicity in personalizing their treatment for their patients.
Keywords
Introduction
Health Disparities
Cardiovascular diseases (CVD) have been established as the leading cause of morbidity and mortality in both developed and developing countries [1-3]. Low- and middle-income countries (LMICs) are disproportionally affected, with over 80% of CVD deaths taking place in LMICs [2]. The WHO in its 2008-2013 Action Plan for the Global Strategy for the Prevention and Control of Non-communicable Diseases draws attention to the rapidity with which the increasing burden of these diseases affects poor and disadvantaged populations, contributing to widening health gaps between and within countries [4].
These gaps or “health disparities” refer to preventable differences in the indicators of health of different population groups, often defined by race, ethnicity, sex, educational level, socioeconomic status, and geographic location of residence (Figures 1A and 1B). Recognizing sex, gender, racial and ethnic differences in cardiovascular risk factors, disease presentation and treatment response is crucial to improving outcomes in these populations and reducing disparities. This review has the objective to increase the awareness of racial, ethnic-based disparities among cardiovascular health care professionals because all of us also have to play a role in this complex topic.
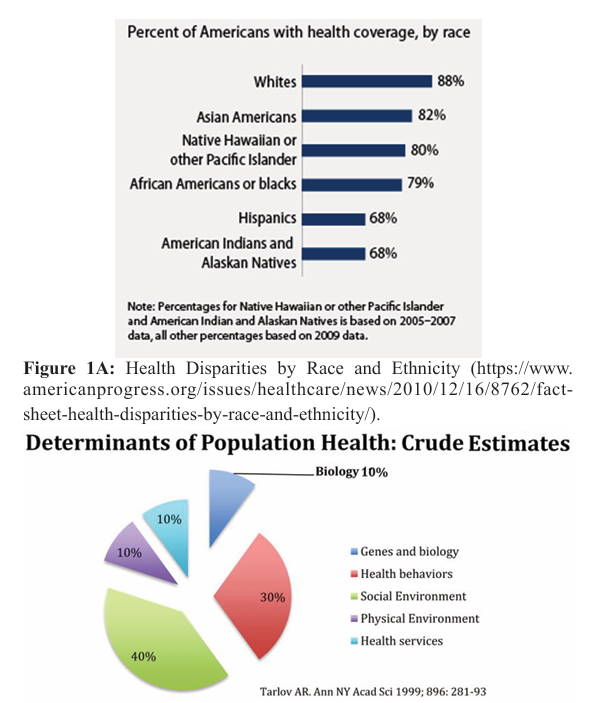
Figure 1B: Determinants of Population Health emphasizing the relatively minor contribution of genes and biology (crude estimates).
Disparities in Coronary Heart Disease
In a bivariate analysis [5] in order to compare coronary arteries obstructions between clinically similar African Americans (AA) and white persons that undergoing coronary angiography within 90 days of a nuclear imaging study, the AA patients showed less severe CAD than whites (p = 0.01) (Figure 2). In particular, AA were less likely to have severe obstructive coronary artery disease (39.4% vs. 26.9%) and more likely to have no significant obstructions (36.5% vs. 23.6%). These results suggest that AA have less coronary obstruction than apparently clinically similar whites. Further studies are required to confirm these findings and better understand the paradox of why AA are less likely to have obstructive coronary disease but more likely to suffer mortality from coronary disease. On the other hand, overall, the prevalence of coronary heart disease (CHD) and peripheral artery disease is lower in Afro-Caribbean populations [6,7,9-10,11] when compared to other ethnic groups except for Immigrant Chinese and African Blacks to the UK [6,11]. Prevalence of CHD ranged from 0–7 % [7] in Afro-Caribbean compared to 2–22 % [7,13] in Caucasians. One study [13] reported no difference in the prevalence of CVD among Afro-Caribbean compared to other ethnic groups. Two studies reported a higher prevalence of cerebrovascular disease among Afro-Caribbeans, Caucasians and Indo-Asians [13,8].

left anterior descending; Mild = one or two systems with obstructions, not including the proximal left anterior descending; None = no obstruction ≥70%. Whittle J., Kressin NR, Petterson E., Orner M., Glickman M., Mazzella M., Petersen L. Racial Differences in Prevalence of Coronary Obstructions Among Men with Positive Nuclear Imaging Studies. JAAC 2005; 47 (10) 2034-41.
Coronary artery disease mortality in Afro Caribbeans
A Systematic literature review have found that coronary heart disease mortality is significantly lower among Afro-Caribbean compared to South Asian, Caucasian, US Blacks and East African ethnic groups [14]. The study also found that place of birth also emerged as a disparity theme in the analyses. Southern born US Blacks had a standardized rate of death from coronary heart disease more than twice that of Caribbean-born Blacks (406.5 vs. 165.2 per 100,000) in the less than 65 years age group. Coronary heart disease deaths were also lower in Caribbean-born Blacks compared to US Northeastern. Whites. On the other hand in all age groups and both sexes, deaths due to stroke were higher among Caribbean-born blacks than among US Northeastern-born whites. Finally, this analysis also found that the prevalence of peripheral arterial disease was lower in Afro-Caribbeans when compared to Caucasians but higher than that of South Asians [14] (Figure 3).
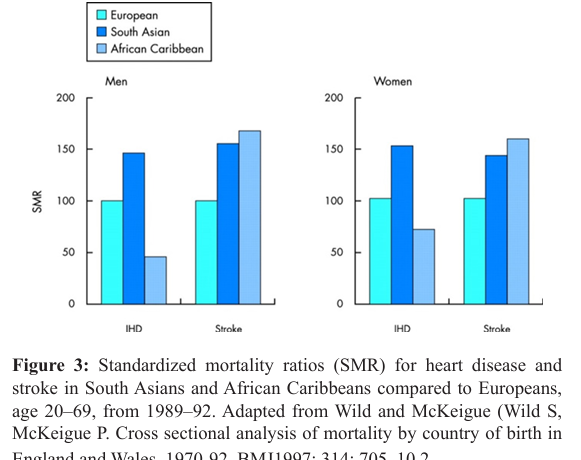
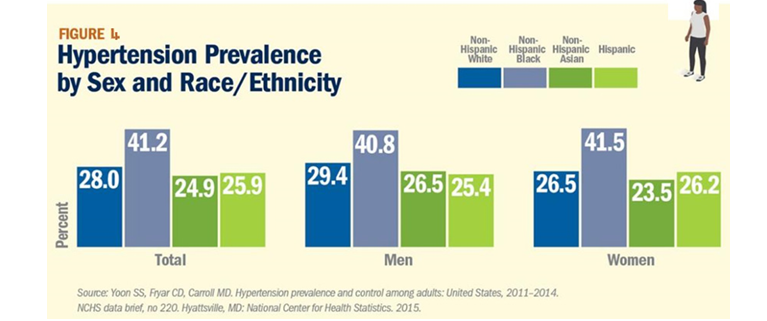
Figure 4: Hypertension Prevalence by Sex and Race/Ethnicity.
Blacks in the U.S. have the highest rate of hypertension in the world, with a prevalence of 41.2 percent in 2011-2014 compared with 28 percent among whites, 24.9 percent among Asians and 25.9 percent among Hispanics. In addition, blood pressure control rates for blacks with hypertension are lower than other groups, despite higher awareness and treatment rates. [Heart Disease and Stroke Statistics-2018 Update: A Report from the American Heart Association. Benjamin EJ, Virani SS, Callaway CW, et al. Circulation. 2018; 137:e67-e492].
Hypertension in Blacks
Blacks are more disproportionately affected by Hypertension (HTN) and its comorbid conditions. In the US, the prevalence of HTN is 40-50% in African-Americans when compared to 25– 30% in Whites. Furthermore, the prevalence of HTN associated complications is higher in Blacks than Whites. Compared to Whites, Blacks have higher prevalence of heart failure, by twofold, stroke, by twofold to fourfold and kidney failure, by twofold to fourfold in the US. These could partly explain the higher disparities in CVD outcomes in Blacks than Whites [15] (Figure 4). Black patients of African origin have more severe and resistant hypertension, often because of genetically determined predisposition to salt and water retention, with suppressed plasma renin activity (Figure 5).
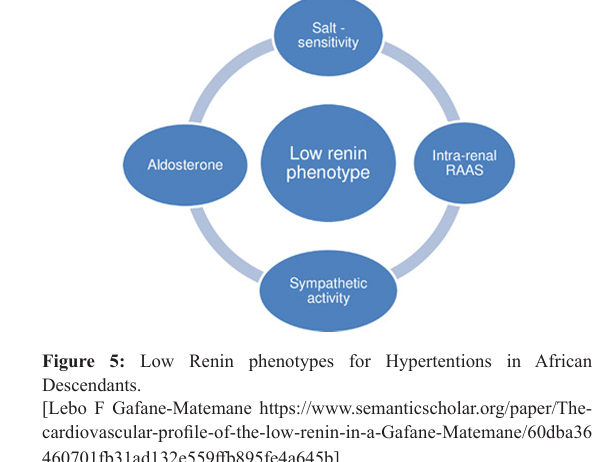
Furthermore, there are two main groups of low-renin hypertensives: those with a primary aldosteronism phenotype (low renin/high aldosterone), for whom the best therapy is aldosterone antagonists and those with a Liddle phenotype (low renin/low aldosterone), for whom the specific therapy is amiloride. Patients with a renal phenotype (high renin with secondary hyperaldosteronism) that respond best to angiotensin receptor blockers or renin inhibitors are less common and patients with the Liddle phenotype (low renin/low aldosterone) because of overactivity of Renal tubular epithelial sodium channel -ENaC) might be more common than most physicians appreciate [16]. Therefore, even though BP lowering may not be as robust with the “anti-renin” drugs (ie ACEIs/ARBs/Beta-blockers), the tissue-protective benefits should certainly be considered in the treatment of blacks in an effort to not only improve BP control but to achieve the ultimate goal of reducing the risk of organ damage. On the other hand Adrenergic receptor blockers or beta-blockers, specially the first generation ones, might be less effective in a subgroup of African American subjects for the management of congestive heart failure [17]. This reduced efficacy might be related to variants in two genes related to the G protein–coupled pathway of the b1-adrenergic receptor (ADRB1) and G protein receptor kinase 5 (GRK5) genes. Traditionally, Thiazide diuretics, angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, and calcium channel blockers (CCB) have been the preferred medications in nonblack patients and thiazide diuretics and calcium channel blockers are preferred in black patients. While CCBs and diuretics have been shown to be the most effective therapies for lowering BP in the African-American patient, the patient at high risk for CVD should also be considered for therapy with cardioprotective agents such as ACE inhibitors, ARBs, and beta-blockers that have been shown to provide greater protection against end-organ damage. This protection is the ultimate rationale for their inclusion in antihypertensive therapy [18].
Reduced NTproBNP Levels in African Americans
African Americans have substantially lower plasma NTproBNP levels; compared to Caucasians. African Americans have a higher prevalence of HTN, left ventricular hypertrophy, and microalbuminuria, conditions that should raise NP levels. Consequently, the finding in ARIC that African-American individuals have lower NP levels, compared to white individuals, is counterintuitive and suggests that nonhemodynamic factors may contribute. One biologically plausible way in which NP levels may be decreased is through impaired synthesis or reduced release from cardiomyocytes. Indeed, previous studies indicate that variations in processes related to the synthesis of NTproBNP, such as genetic polymorphisms in the NPPB gene that influence transcription, translation, and/or post-translational processing, may contribute to lower NTproBNP levels, although there are limited data on racial differences in the genetics of the NP system [19]. In conclusion: African Americans have lower levels of plasma NTproBNP than Caucasians, which may be partially owing to genetic variation. Low natriuretic peptide levels in African Americans may contribute to the greater risk for HTN and its sequalae in this population.
Heart Failure (HF) in African Americans (AA)
As suggested by the clinical trials experience, HF in African Americans is much more commonly associated with a nonischemic etiology of left ventricular dysfunction. Hypertension is considered to be the putative disease process, but dilated cardiomyopathies and diabetes-related diseases are also common in African Americans. Coronary artery disease remains a cause of left ventricular dysfunction in African Americans, but, as an attributable cause of HF, it is strikingly less common in African Americans than in whites [20] Several reasons have been proposed associated with the increased HF in AA, to note: a) Modifiable risk Factors b) Neurohormonal imbalances and endothelial dysfunction c) Genetic Polymorphisms d) Socioeconomic factors and quality of care [21].
“Race-Based” Differences in pathophysiology and response to Heart Failure medications
Several polymorphisms associated with the risk of heart failure may provide insight into some of the “race-based” differences in pathophysiology and response to medications and, it is hoped, may eventually serve as the basis for a future in tailored therapy. Genes of interest include those for: • Beta 1 adrenergic receptor • Alpha 2c receptor • Aldosterone Synthase • G protein • Transforming growth factor beta • Nitric oxide synthase • Transthyretin [21], for instance Blacks are also more likely to achieve a substantial clinical benefit from the use of nitric-oxide-enhancing therapy (isosorbide dinitrate/hydralazine) than whites than other ethnicities, furthermore although previous research suggested racial differences in beta-blocker effectiveness for treating heart failure with reduced ejection fraction by self-reported race, namely, some studies reports that Beta blockers appears to be 40 –50% less effective in preventing death or hospitalization among African American patients with Heart Failure as compared with white individuals [22], however a recent investigation of Self-Reported Race and Proportion of African Genetic Ancestry concluded that among black and white patients with heart failure and reduced ejection fraction, reduction in all-cause mortality associated with Beta-Blocker exposure was similar, regardless of self-reported race or proportion African genetic ancestry [23]. Finally in the topic of Polymorphisms associated with the risk of heart failure is important to mention that most African Americans have some European ancestry. In one study, the estimated proportion of European ancestry ranged from 7% in Jamaicans of African descent to approximately 23% in African Americans in New Orleans [26].
Lessons from the regional clinical Studies on Afro Caribbean Patients with Heart Failure Living in Jamaica
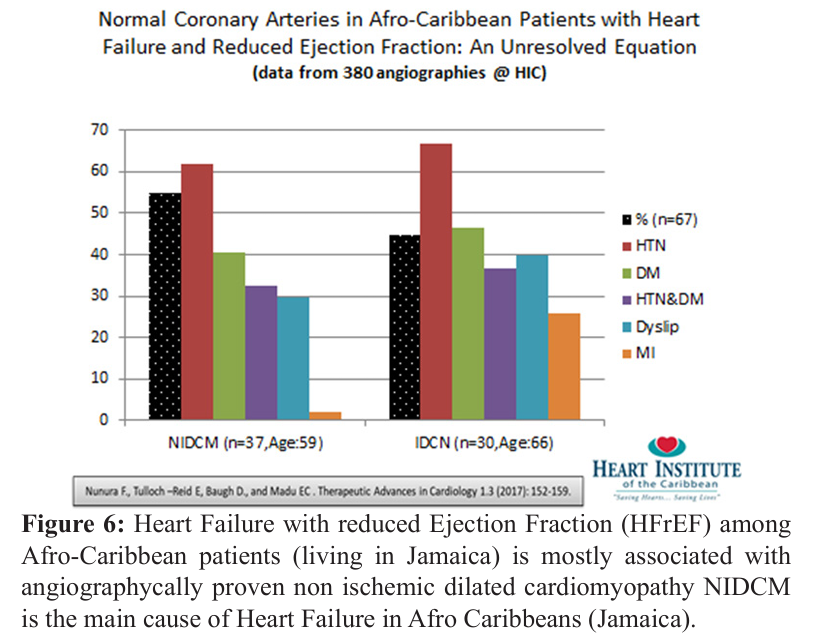
Our clinical observations demonstrated that Heart Failure with reduced Ejection Fraction (HFrEF) among Afro-Caribbean patients (living in Jamaica) is mostly associated with angiographically proven non ischemic dilated cardiomyopathy –NIDCM vs IDCM- (55vs.45%) (Figure 6). Interesting, this final outcome (NIDCM) occurs despite the fact that both (NIDCM and IDCM) group of patients were exposed to similar strong CAD risk factors (Hypertension and Diabetes) during their life-time, suggesting that other factors (i.e. coronary microvascular dysfunction) might play a role in the etiology of the Heart Failure [24]. More regional clinical studies might be useful to improve our current Heart Failure Guideline-Directed Medical Therapy (GDMT) experience as there is a need to understand more the epidemiology and mechanisms of Afro Caribbean Heart Failure in order to improve the current management practices, for instance we recently founded that the use of Valsartan/Sacubitril (ARNI-Angiotensin Receptor blocker / Neprysilin Inhibitor) therapy was safe, well tolerated and effective in a cohort of Afro Caribbean Heart Failure (HFrEF) population [25].
Conclusion
There are important differences in morbidity and mortality from cardiovascular diseases across ethnic groups [14]. To recognize this is particularly important in order to understand the nature of cardiovascular disease health disparities among African descendant /Afro-Caribbean origin populations. Nowadays there are more interest in recognize the substantial race/ethnicity differences in pathophysiology, preventive approaches, clinical presentations, management issues and prognosis [26]. Many knowledge gaps remain in understanding the pathophysiologic and social determinants (socioeconomic status, physical environment, employment status, access to care and social support) of these disparities in cardiovascular diseases, accordingly, more research exploring these gaps by varying disparity indicators needs to be undertaken.
References
- Yusuf S, Reddy S, Ounpuu S, et al. Global burden of cardiovascular diseases: Part II: variations in cardiovascular disease by specific ethnic groups and geographic regions and prevention strategies. Circulation. 2001; 104: 2855-2864.
- World Health Organization. Global status report on noncommunicable disease 2010. In World Health Organization. Geneva. 2011; 176.
- Caribbean Commission on Health and Development. Report of the Caribbean Commission on Health and Development. In Caribbean Community (CARICOM) Secreteriat. Kingston. 2006; 154.
- World Health Organization. 2008-2013 Action plan for the global strategy for the prevention and control of noncommunicable diseases. In: Working in partnership to prevent and control the four noncommunicable diseases - cardiovascular diseases, diabetes, cancers and chronic respiratory diseases and the four shared risk factors - tobacco use, physical inactivity, unhealthy diets and the harmful use of alcohol. World Health Organization. Geneva. 2009: 42.
- Jeff Whittle, Nancy R Kressin, Eric D Peterson, et al. Racial Differences in Prevalence of Coronary Obstructions Among Men with Positive Nuclear Imaging Studies. J Am Coll Cardiol. 2005; 47: 2034-2041.
- Brindle P, May M, Gill P, et al. Primary prevention of cardiovascular disease: a web-based risk score for seven British black and minority ethnic groups. Heart. 2006; 92: 1595-1602.
- Chaturvedi N, McKeigue PM, Marmot MG. Relationship of glucose intolerance to coronary risk in Afro-Caribbeans compared with Europeans. Diabetologia. 1994; 37: 765-772.
- Cruickshank JK, Beevers DG, Osbourne VL, et al. Heart attack, stroke, diabetes, and hypertension in West Indians, Asians, and whites in Birmingham, England. Brit Med J. 1980; 281: 1108.
- Gill PS, Calvert M, Davis R, et al. Prevalence of heart failure and atrial fibrillation in minority ethnic subjects: The Ethnic-Echocardiographic Heart of England Screening Study (E-ECHOES). PLoS ONE. 2011; 6: e26710.
- Goyal D, Tayebjee M, Lip GYH, et al. South Asian or Afro-Caribbean ethnicity is not associated with altered 1 min heart rate recovery estimates in suspected coronary artery disease patients. Int J Cardiol. 2007; 114: 261-264.
- Wang Y, Rudd AG, Wolfe CDA. Trends and survival between ethnic groups after stroke: The South London Stroke Register. Stroke. 2013; 44: 380-387.
- Wild S, McKeigue P. Cross sectional analysis of mortality by country of birth in England and Wales, 1970-92. BMJ. 1997; 314: 705-710.
- Zaninotto P, Mindell J, Hirani V. Prevalence of cardiovascular risk factors among ethnic groups: results from the Health Surveys for England. Atherosclerosis. 2007; 195: 48-57.
- Damian K Francis, Nadia R Bennett, Trevor S Ferguson, et al. Disparities in cardiovascular disease among Caribbean populations: A systematic literature review. BMC Public Health. 2015; 15: 828.
- Kwame Osei, Trudy Gaillard. Disparities in Cardiovascular Disease and Type 2 Diabetes Risk Factors in Blacks and Whites: Dissecting Racial Paradox of Metabolic Syndrome. Front Endocrinol. 2017; 8: 204.
- David Spence J, Brian L Rayner. Hypertension in Blacks Individualized Therapy Based on Renin/Aldosterone Phenotyping. Hypertension. 2018; 72: 263-269.
- Dries DL, Exner DV, Gersh BJ, et al. Racial differences in the outcome of left ventricular dysfunction. N Engl J Med. 1999; 340: 609-616.
- Yancy CW. Executive Summary of the African-American Initiative. MedGenMed. 2007; 9: 28.
- Deepak K Gupta, Brian Claggett, Quinn Wells, et al. Racial Differences in Circulating Natriuretic Peptide Levels: The Atherosclerosis Risk in Communities Study. J Am Heart Assoc. 2015; 4: e001831.
- Joseph A Franciosa, Keith C Ferdinand, Clyde W Yancy, et al. Treatment of Heart Failure in African Americans: A Consensus Statement. Congestive Heart Failure. 2010; 16: 27-38.
- Alok Sharma, Monica Colvin-Adams, Clyde W Yancy. Heart Failure in African Americans: disparities can be overcome. Cleveland Clinic Journal of Medicine. 2014; 81: 301-311.
- David E Lanfear, Tara N Hrobowski, Edward L Peterson, et al. Association of beta-blocker exposure with outcomes in heart failure differs between African American and white patients. Circ Heart Fail. 2012; 5: 202-208.
- Jasmine A Luzum, Edward Peterson, Jia Li, et al. Race and Beta-Blocker Survival Benefit in Patients with Heart Failure: An Investigation of Self-Reported Race and Proportion of African Genetic Ancestry. JAHA. 2018; 7: e007956.
- Nunura F, Tulloch-Reid E, Baugh D, et al. Normal Coronary Arteries in Afro-Caribbean Patients with Heart Failure and Reduced Ejection Fraction: An Unresolved Equation. Therapeutic Advances in Cardiology. 2017; 1: 152-159.
- Felix Nunura, Edwin Tulloch-Reid, Daniel Nepaul, et al. Real-World Evidence for the Tolerance and Effectiveness of the First Drug (Sacubitril/Valsartan) in a New Class-ARNI in Afro-Caribbean Patients with Heart Failure and reduced Ejection fraction. Journal of Clinical and Experimental Cardiology. 2019; 10: 1-5.
- Parra EJ, Marcini A, Akey J, et al. Estimating African American admixture proportions by use of population-specific alleles. Am J Hum Genet. 1998; 63: 1839-1851.
- https://www.acc.org/latest-in-cardiology/articles/2018/10/14/12/42/cover-story-one-size-does-not-fit-all-sex-gender-race-and-ethnicity-in-cardiovascular-medicineCoverstory:Onesizedoesnotfitall-sex,gender,race,andethnicityincardiovascularmedicine.