Removal of an Impacted Foreign Body from The Upper Airway with a Gastroscope in a Tertiary Hospital in South-West Nigeria – A Case Report
Author'(s): Oguntoye Oluwatosin Oluwagbenga1, Yusuf Musah1, Olowoyo Paul1, Aremu Shuaib Kayode2, Soje Michael Osisiogu1, Oguntoye Oluwafunmilayo Adenike3, Raji Mustapha4, Oguntade Hameed Banjo3, Ariyo Olumuyiwa Elijah3, Atolani Segun Alex3, Talabi Olukayode Abiola3, Ogunmola Toba Osiron3
1Department of Internal Medicine, Federal Teaching Hospital Ido-Ekiti and Afe Babalola University Ado-Ekiti, Nigeria.
2Department of Otorhinolaryngology, Federal Teaching Hospital Ido-Ekiti and Afe Babalola University Ado-Ekiti, Nigeria.
3Department of Internal Medicine, Federal Teaching Hospital Ido-Ekiti, Nigeria.
4Department of Otorhinolaryngology, Federal Teaching Hospital Ido-Ekiti, Nigeria.
*Correspondence:
Dr. Oguntoye Oluwatosin Oluwagbenga MBBS (Ibadan), FWACP(Gastroenterol), Lecturer 1 and Consultant Physician / Gastroenterologist and Hepatologist, Department of Internal Medicine, Federal Teaching Hospital Ido-Ekiti and Afe Babalola University Ado-Ekiti, Ekiti State, Nigeria.
Received: 21 April 2020 Accepted: 02 May 2020
Citation: Oguntoye O Oluwagbenga, Yusuf Musah, Olowoyo Paul, et al. Removal of an Impacted Foreign Body from The Upper Airway with a Gastroscope in a Tertiary Hospital in South-West Nigeria – A Case Report. Gastroint Hepatol Dig Dis. 2020; 3(1): 1-5.
Abstract
Foreign body ingestion and food bolus impaction are encountered commonly in clinical practice and are a common endoscopic emergency. A wide variety of objects could be ingested which could get impacted, and the site of impaction is commonly the oesophagus but can also be the airway depending on the nature of the substance ingested, the age of the patient and the presence of a neurologic disorder. The predominant clinical features of a patient will depend on the site of impaction of the foreign body; the airway or the oesophagus. Endoscopy remains the gold standard for the diagnosis and management of foreign body ingestion of which there are different modalities and equipment types. For foreign body in the airway laryngoscopy, tracheoscopy and bronchoscopy are the modalities indicated and there are also different types of retrieval devices some of which include standard biopsy forceps, retrieval graspers, retrieval forceps and polypectomy snares. The management of foreign body ingestion cuts across different specialties including Pulmonology, Otorhinolaryngology, General surgery, Cardiothoracic surgery and Gastroenterology all of which are involved in various different endoscopic procedures and their endoscopy equipment have a lot of similarities and in certain instances they can be adapted to perform varying roles. Foreign bodies in the airway require urgent endoscopic removal because it can become rapidly life threatening with associated high morbidity and mortality, therefore the available equipment should be immediately deployed to save lives. We present a case of foreign body impaction in the upper airway (larynx) that was removed with a flexible video Gastroscope using a polypectomy snare
Keywords
Introduction
Foreign body ingestion and food bolus impaction are encountered commonly in clinical practice and are a common endoscopic emergency [1]. The majority of foreign body ingestions occur in the pediatric (75%) population but frequently occur among adults (25%) also [2,3]. The site of impaction is commonly the oesophagus but can also be the airway depending on the nature of the substance ingested, the age of the patient and the presence of a neurologic disorder [4]. The airway can be divided into the upper airway, which includes the nasal cavity, the oral cavity, the pharynx, and the larynx while the lower airway consists of the tracheobronchial tree. Foreign bodies can lodge either in the upper airway or the lower airway.
While a wide variety of objects could be ingested, the most common foreign bodies in children are coins, marbles, button, batteries, safety pins and bottle tops. In adults, common foreign bodies are meat bone, fish bone, dentures and metallic wires [4,5]. Patients usually present with history of accidental swallowing of such objects, often while eating or during sleep or in association with seizures, trauma, or in the presence of some degree of neurologic or psychological dysfunction.
The clinical features depend on the site of impaction of the foreign body. In the airway, patients may present with choking, gagging, coughing, hoarseness of voice, breathlessness, stridor, chest tightness, wheezing or cyanosis [6]. The predominant clinical features can indicate the section of the airway that is affected. For laryngotracheal foreign bodies they include dyspnea, cough, and stridor, whereas those of bronchial foreign bodies include cough, decreased air entry, wheezing, and dyspnea [7]. In the oesophagus, patients may present with dysphagia, odynophagia, hypersalivation, retrosternal fullness, regurgitation, hiccups or retching [8,9].
If the diagnosis of foreign body in the upper airway is not established immediately and the object removed, the foreign body can get dislodged distally and retained in the bronchial tree leading to recurrent pneumonias, bronchiectasis, recurrent hemoptysis, pneumothorax, lung abscesses, pneumomediastinum, or other complications [10].
Endoscopy remains the gold standard for the diagnosis and management of foreign body ingestion of which there are different modalities and equipment types ranging from flexible to rigid scopes which have their merits and demerits but flexible endoscopes are generally preferred partly because they can be used under local anesthesia [11,12]. For foreign body in the airway laryngoscopy, tracheoscopy and bronchoscopy are the modalities indicated while for foreign body in the oesophagus, oesophagoscopy is indicated with success rates greater than 95% and complication rates of 0%–5% [13].
The choice of retrieval device is determined by the size, location and shape of the foreign body, by the endoscope length and instrument channel, and by the endoscopist’s preference and practice. Examples of retrieval devices include: standard biopsy forceps, retrieval graspers, retrieval forceps, polypectomy snares, multi-prong snares, endoscopic baskets, magnetic probes, retrieval nets or bags, balloon catheters and cryoprobe [12,13].
Foreign bodies in the airway require urgent endoscopic removal because it can become rapidly life threatening with high morbidity and mortality. Foreign body aspiration accounts for 0.16–0.33% of adult bronchoscopic procedures [14]. Most oesophageal foreign bodies (80%–90%) pass spontaneously but 10%-20% of cases will require endoscopic removal, while less than 1% will need surgery for foreign body extraction or to treat complications [15,16].
Despite improvements in medical care and public awareness, approximately 3000 deaths occur each year in the United States from foreign body aspiration, with most deaths occurring before hospital evaluation and treatment [12]. Use of the Heimlich maneuver as a first line intervention for foreign body in the upper airway has improved the mortality rate of patients with complete airway obstruction, but its use in patients with partial obstruction may result in complete airway obstruction, therefore it is not always beneficial [12].
The management of foreign body ingestion cuts across different specialties including Pulmonology, Otorhinolaryngology, General surgery, Cardiothoracic surgery and Gastroenterology all of which are involved in various different endoscopic procedures. The principle of endoscopy is the same and the equipment used by different specialties have a lot of similarities and in certain instances they can be adapted to perform varying roles.
We present a case of foreign body impaction in the upper airway (larynx) that was removed with a flexible video Gastroscope using a polypectomy snare at the Federal Teaching Hospital Ido-Ekiti, Ekiti state in south-western Nigeria.
Case Presentation
Mr A.S., a 50-year old trader who was rushed to the emergency room on account of sudden onset noisy breathing of two days duration with associated difficulty with breathing which became worse a day prior to presentation. He was apparently well until two days prior to presentation when while he was eating, he was said to have complained that the bolus of meat he swallowed was stuck in his throat and he immediately started having noisy breathing with associated breathlessness. There was also associated hoarseness of his voice.
There was no cough but he had a feeling of choking and a feeling of a lump in his throat. No precordial pain, no palpitations, no fainting spells but patient had diaphoresis. No recent prolonged immobilization or recent long-distance travel, no calf pain or swollen limbs and no pleuritic pain. He is a known patient with systemic arterial hypertension with poor drug compliance who has a history of previous Left hemispheric ischaemic stroke one year ago but still had significant residual neurologic deficit (right-sided hemiparesis) despite physiotherapy.
Prior to this incident of choking while eating, there was no complain of worsening of the weakness in his right upper and lower limbs and no weakness in the contralateral limbs, there was no headaches, no sudden unilateral visual loss, no slurred speech, no deviation of the mouth to one side, no observable facioparesis by the caregivers, no convulsion, no altered sensorium or loss of consciousness, no neck pain or neck stiffness, no nausea or vomiting, no dizziness, no vertigo and no tinnitus. No past history of similar choking while eating, no past history of dysphagia or odynophagia and no history of drooping of the eyelids (or ptosis), no difficulty with opening the mouth. No history of mouth lesions or ulcers and no loose tooth. He has no dental prosthesis. No history of orthopnea or paroxysmal nocturnal dyspnea and no pedal oedema.
He is not a known patient with diabetes mellitus, bronchial asthma or chronic obstructive pulmonary disease. Not a known patient with seizure disorder. No past history of surgery. He is married in a monogamous family setting and has four children. He does not smoke cigarette nor drink alcohol. He has not been regular with his anti-hypertensive medications and not on any other routine medications. He has no known allergy.
Every attempt the patient made as well as that of his caregivers to get the meat bolus out proved abortive. He was initially taken to a primary health facility where he was placed on supplemental oxygen but they also could not get the meat bolus out because of lack of the necessary equipment and expertise. He was subsequently referred to our health facility the following day for further intervention and management.
At presentation in our emergency room he was conscious, extremely breathless and in severe respiratory distress, having grunting breathing, febrile (temperature was 38.1oC), diaphoretic, centrally cyanosed and progressively getting exhausted. No neck swelling or neck mass noted. The respiratory rate was 40cycles/ minute, Sp02 was 67%, and on auscultation of the chest, he had widespread crackles bilaterally, no rhonchi. The pulse rate was 120 beats/minute, blood pressure was 170/100mmHg and the heart sounds were S1 and S2 only; there was no murmur. There was absent gag reflex and a right cranial nerve 7 palsy; upper motor neuron type. The muscle power was 2 in the right upper limb and 3 in the right lower limb. There was hypotonia and hyporeflexia in the right limbs but the findings in the left upper and lower limbs were essentially normal. There was no other remarkable abnormality noted and abdominal examination was normal.
A provisional diagnosis of Upper airway obstruction by a foreign body (meat bolus) was made in a known hypertensive patient with residual neurologic deficit from a previous left-sided ischaemic stroke, to keep in view aspiration pneumonitis.
He was immediately placed on high flow (10L/min) 100% intranasal Oxygen and the Sp02 gradually improved from 67% to 88%. He could not be intubated and ventilated mechanically by the anesthesiologists due to the suspected airway obstruction by a foreign body. There was also no facility in our health institution at the time for flexible laryngoscopy or bronchoscopy and the patient was not clinically fit for a rigid laryngoscopy by the otorhinolaryngologists under general anesthesia. The Gastroenterology unit was therefore invited for a possible endoscopic intervention. The patient was optimized and he subsequently had an emergency endoscopy done. In view of the clinical profile of the patient, no sedation or local anesthetic agent was administered but an antimotility agent, intravenous Hyosine Butyl Bromide 20mg stat, was administered to the patient before the commencement of the endoscopy procedure. There was close monitoring of the patient’s Sp02 and vital signs throughout the procedure by an endoscopy nurse.
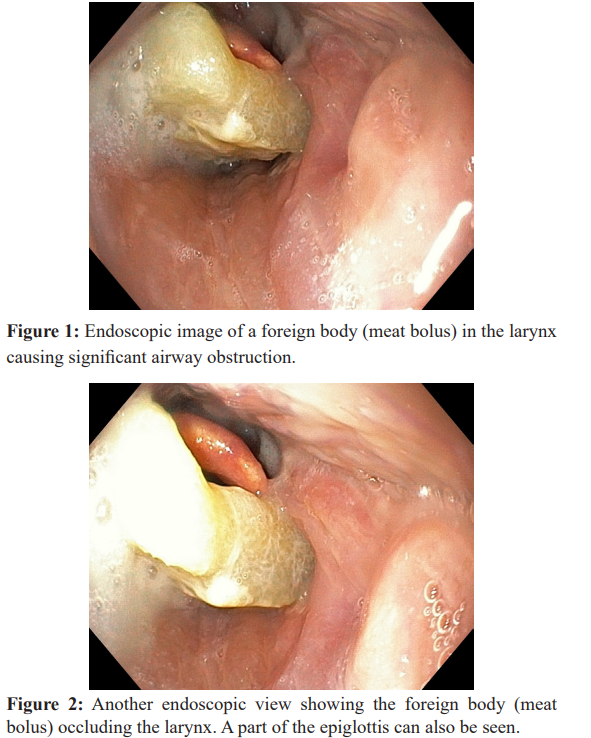
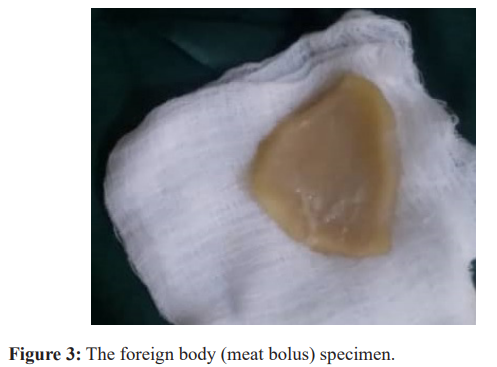
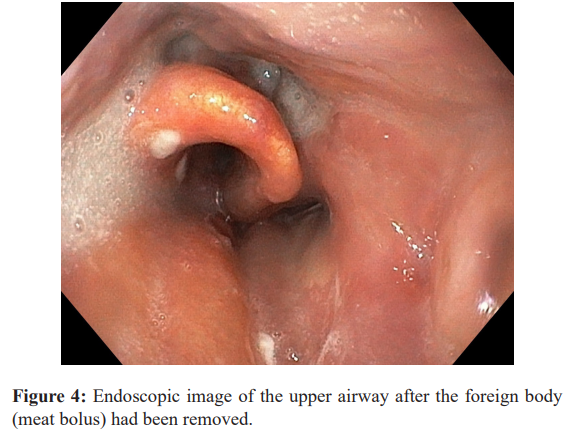
An Olympus CV-170 series (Olympus America Incorporated) with a forward viewing flexible video Gastroscope was used for the procedure. The meat bolus was found abutting on the epiglottis and almost completely occluding the larynx (Figures 1 and 2). The meat bolus was removed with a Polypectomy snare. It measured about 6cm x 5cm x 2cm in dimension (Figure 3). There was an immediate dramatic improvement in his symptomatology thereafter. The noisy breathing stopped and the breathlessness improved remarkably. The endoscope was re-inserted into the pharynx for a proper assessment of the mucosa. The epiglottis was inflamed, there was also surrounding mucosal oedema and hyperaemia; and some exudates seen at the site of impaction (Figure 4). No endoscopic features to suggest a mucosa/wall tear, perforation or any bleeding at the site of impaction.
The procedure was fairly well tolerated and there were no complications. He was continuously monitored while in the recovery room and was subsequently transferred to the ward when his vital signs were satisfactory. He was placed on nil per os (NPO), intravenous fluids (for hydration and calorie maintenance), intravenous dexamethasone, ceftriaxone and metronidazole. He was eventually, transferred to the Neurology/Stroke unit for further management and neuro-rehabilitaion.
Conclusion
The management of foreign body ingestion requires an interprofessional team with an interprofessional approach; this will reduce the morbidity and mortality associated this condition. Most patients will present to the emergency department and the triage nurse or physician has to be aware of the symptoms and signs of a foreign body in the airway or the oesophagus and immediately invite the appropriate specialist.
Foreign bodies in the airway require urgent endoscopic removal because it can become rapidly life threatening, therefore the available equipment should be immediately deployed to save lives. Gastroscopes are used for endoscopic visualization of the upper gastrointestinal tract for diagnostic, screening and therapeutic purposes. Our patient was managed by us at a time when there was no flexible laryngoscopy or bronchoscopy facility in our health institution and the patient was not clinically fit for a rigid laryngoscopy by the otorhinolaryngologists under general anesthesia. A minimally invasive procedure was required at that time which was successfully achieved with the use of the Gastroscope and a polypectomy snare.
Prior to discharge, patients should be evaluated for a possible underlying psychological disorder such as mental retardation, bulimia nervosa or pica; or a neurologic disorder such as stroke or myasthenia gravis; and such patients should be referred to the appropriate specialist for expert care in order to prevent a recurrence. Patients should also be educated about measures to prevent foreign body ingestion and food impaction such as good eating habits; careful removal of bony components from fish and meat; and care of dentures and metallic implants among others.
Acknowledgement
Special thanks to the Endoscopy Nurses, House Officers and Resident Doctors in the Gastroenterology unit of the Department of Internal Medicine for their support in making this publication a reality.
Funding
The authors bore the entire cost of the research and did not receive any financial support from any individual, institution, organization or body towards this research work.
References
- Salih A, Alfaki M, Alam-Elhuda D. Airway foreign bodies. A critical review for a common pediatric World J Emerg Med. 2016; 7: 5-12.
- Baharloo F, Veyckemans F, Francis C. Tracheobronchial foreign bodies: presentation and management in children and adults. Chest. 1999; 115: 1357-1362.
- Hsu Wc, Sheen Ts, Lin Cd. Clinical experiences of removing foreign bodies in the airway and esophagus with a rigid endoscope: a series of 3217 cases from 1970 to 1996. Otolaryngol Head Neck Surg. 2000; 122: 450-454.
- Pulcherio JOB, Magalhães EJC, Oliveira Velasco CMM, et al. Methods for Esophageal Foreign Body Removal Among Pediatric Patients: 10 Years? Experience at a Referral Current Pediatric Research. 2016; 20: 132-136.
- Mondal PJ, Saha S, Ghosh A, et Removal of Foreign Bodies from Esophagus with Flexible Endoscope - A Case Report. Indian J Otolaryngol Head Neck Surg. 2014; 66: 78-80.
- Poirier M. Foreign bodies of the respiratory tract. Intern J Emerg Med. 2003; 2: 1-12.
- Blazer S, Naveh Y, Friedman Foreign Body in the Airway - A Review of 200 Cases. Am J Dis Child. 1980; 134: 68-71.
- Schaefer TJ, Trocinski D. Esophageal Foreign Body. https://ncbi.nlm.nih.gov/books/NBK482131/. Updated: Nov. 26, 2019. Assessed: April 11, 2020.
- Ashraf Foreign body in the esophagus. A review. Sao Paulo Med. J. 2006; 124: 346-349.
- al-Majed SA, Ashour M, al-Mobeireek AF. Overlooked inhaled foreign bodies: late sequelae and` the likelihood of recovery. Respir Med. 1997; 91: 293-296.
- Hewlett JC, Rickman OB, Lentz RJ, et al. Foreign body aspiration in adult airways: therapeutic approach. Journal of Thoracic Disease. 2017; 9: 3398-3409.
- Murray Foreign Bodies of the Airway. https://emedicine.medscape.com/article/872498-overview.Updated: May 07,
- Assessed: April 13, 2020.
- Birk M, Bauerfeind P, Deprez PH, et al. Removal of foreign bodies in the upper gastrointestinal tract in adults: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2016; 48: 1-8.
- Sehgal IS, Dhooria S, Ram B. Foreign Body Inhalation in the Adult Population: Experience of 25,998. Bronchoscopies and Systematic Review of the Literature. Respir Care. 2015; 60: 1438-1448.
- Athanassiadi K, Gerazounis M, Metaxas E, et Management of esophageal foreign bodies: a retrospective review of 400 cases. European Journal of Cardio-Thoracic Surgery. 2002; 21: 653-656.
- Pfau PR. Removal and management of esophageal foreign bodies. Techniques in Gastrointestinal Endoscopy. 2014; 16: 32-39.