Seroprevalence of Hepatitis B Virus in Pregnant Women in Pointe-Noire
Author'(s): AHOUI APENDI C P1,2*, ITOUA-NGAPORO N A1,2, MONGO-ONKOUO A1,2, AGOUNDA B M2,3, MIMIESSE MONAMOU J F1,2, NZIENGUE M'VOUALA J B3, NGAMI R S1,2, NGALESSAMI MOUAKOSSO M1, DEBY GASSAYE1,2, ATIPO IBARA B I1,2, IBARA J R1,2
1Department of Gastroenterology and Internal Medicine, Brazzaville University Hospital, Brazzaville, Congo.
2Faculty of Health Sciences, University Marien Ngouabi of Brazzaville, Brazzaville, Congo.
3National Blood Transfusion Center, Brazzaville, Congo.
*Correspondence:
Ahoui Apendi C P, Department of Gastroenterology and Internal Medicine, Brazzaville University Hospital, Brazzaville, Congo.
Received: 29 November 2019 Accepted: 16 December 2019
Citation: Ahoui Apendi Clausina, Itoua-Ngaparo N A, Mongo-Onkouo Arnaud, et al. Seroprevalence of Hepatitis B Virus in Pregnant Women in Pointe-Noire. Gastroint Hepatol Dig Dis. 2019; 2(2): 1-4.
Abstract
Objective: To characterize the epidemiological profile of HBV infection in women pregnant in Pointe-Noire.
Patients and Methods: This was a descriptive cross-sectional study conducted in Pointe-Noire over a 6-month period. The study concerned pregnant women received in antenatal care in some hospitals in the city. Screening for HBsAg was performed using two tests,namelytheHbsAgimmunochromatographic test and the fourth generation ELISA. The socio-demographic factors of the study population as well as the risk factors for transmission of the virus were studied.
Results: During the study, 150 pregnant women were enrolled. The average age was 27.22 +/- 6.10 years old. The most represented age group was 25 to 35 years old. The majority of women were common-law, had a college-level education, were unemployed and consulted from the second trimester of pregnancy. Scarification was the most important risk factor in 52% of cases. Immunization coverage was low, around 3.33%. The frequency of HBsAg
was 2.67%. Infection predominated in scarified women, women in middle school, and women in common-law unions. However, no significant difference was found between this biological marker and the study variables.
Keywords
Introduction
Viral hepatitis B is a highly endemic infection and a public health problem [1,2]. It is estimated that there are 350 million chronic HBV carriers worldwide [3]. Africa and Asia are the most affected areas, with prevalence generally above 8% [4]. Modes of transmission are known, viremic women constitute a veritable reservoir of vertical transmission, which increases the frequency and incidence of this infection, especially in developing countries [5]. Indeed, the prevalence of the virus in pregnant women ranges from 0.6% in areas with low endemicity to 20% in areas of high endemicity [6]. The risk of mother-to-child transmission of HBV reaches 90% in the perinatal period with a similar transition rate to chronicity [5]. Although often asymptomatic, the infection can induce complications of variable severity in both mother and child [5,7]. In the Congo, HBV work in pregnant women was restricted to Brazzaville [8,9]. The objective of the study was to characterize the epidemiological profile of pregnant women carrying HBV living in Pointe-Noire in order to contribute to the fight against this virus.
Study method
This was a cross-sectional descriptive study that took place from June to November 2018, for a six-month period, in Pointe-Noire Integrated Health Centers and Loandjili Hospital. The consenting pregnant women in the study, who had been living in the city for more than 6 months and had an unknown HBV serological status and who received antenatal care regardless of the term, were included systematically. Sociodemographic factors in the study population (age of female, age of pregnancy, level of education, occupation, marital status) and risk factors for transmission of the virus were studied. The HBsAg Gold Rapid Screen immuno- chromatographic test was used for the detection of HBsAg in the sera collected. The fourth-generation ELISA technique, using the Monolisareagent TM HbsAg ULTRA, confirmed the results. The Microsoft Excel version 2013 and Epi-Info version 7.2.2.6 software were used for data entry and analysis. The odds ratio (OR) and the 95% confidence intervals (95% CI) were calculated, the significance level was set at 5%.
Results
Sociodemographic Factors of the Study Population
Data collection allowed to include 150 women in the study. The extreme ages were 15 and 43 years, the average age of 27.22 +/- 6.10 years. The most represented age group was 25 to 35 years old. Figure 1 illustrates the distribution of the population by age group.
The majority of pregnant women were common-law (84.67%), had a college-level education, were unemployed and consulted from the second trimester of pregnancy. Table 1 shows the distribution of the population by marital status, educational attainment, occupation of women, and age of pregnancy.
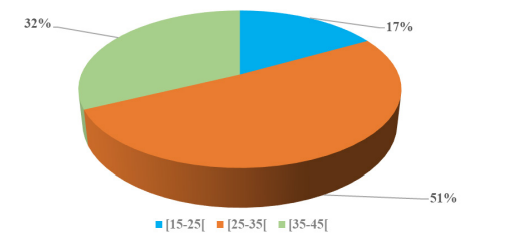
Figure 1: Distribution of the population by age group.
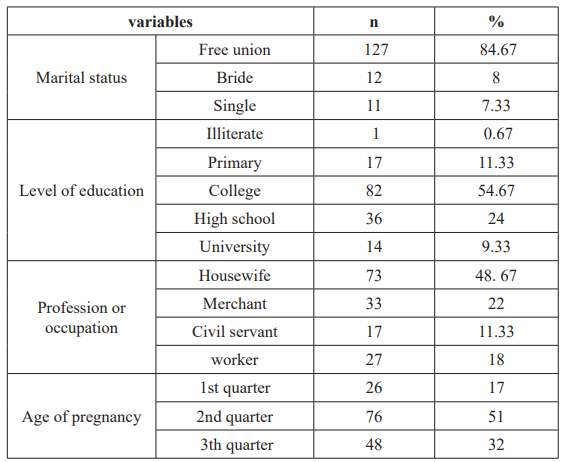
Table 1: Distribution of the population by socio-demographic factors.
Transmission Risk Factors
Scarification was the most represented risk factor at 52%, followed by piercing, tattooing and sexual risk. Immunization coverage was low at 3.33%. The distribution of the population according to the risk factors for HBV transmission is shown in Figure 2.
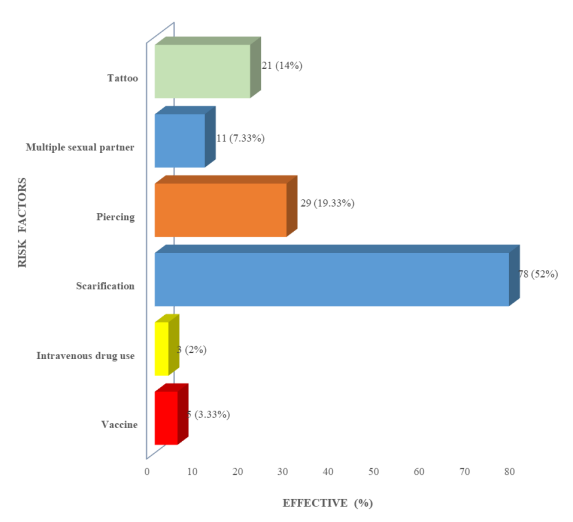
Figure 2: Distribution of the population as of transmission of HBV risk factors.
HBV carriage frequency
Of the 150 women examined, only four had HBsAg at a frequency of 2.67%.
Distribution of HBV positive pregnant women according to epidemiological data
The young population, especially those aged between 15 and 25 years, was the most exposed to HBV in the study. It is the same for women at the college level and those living in a common-law relationship. Table 2 shows the distribution of pregnant women with HBsAg according to socio-demographic factors.
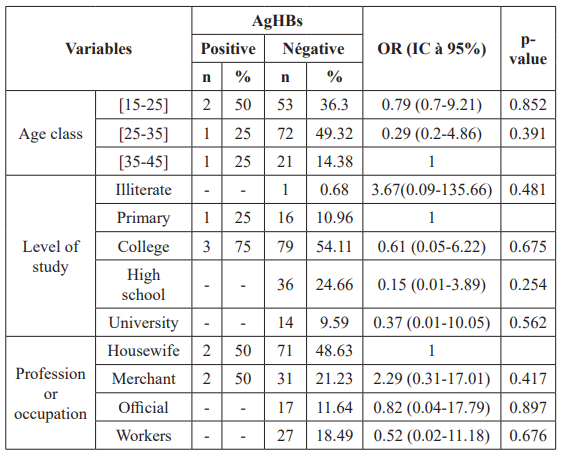
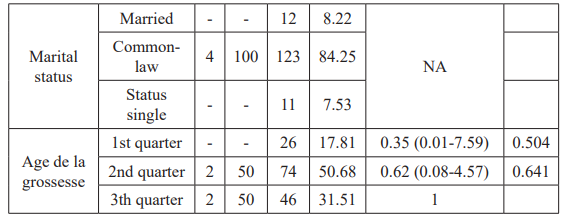
Table 2: Distribution of HBV positive pregnant women by socio- demographic factors.
OR: Odd ratio; IC: confidence interval; NA: not applied.
Infection predominated in scarified women, tattooed women and those wearing a piercing. The distribution of pregnant women with HBsAg according to risk factors for transmission is shown in Table 3.

Table 3: Distribution of HBV positive pregnant women according to risk factors for transmission.
Discussion
In order to optimize the reliability of the results, we opted for the use of two identification tests. These means of diagnosis are traditional in some works, in particular they were used in a study on the seroprevalence of HBV in the department of Likouala in Congo [10].
Similar observations concerning the youth of our study population have been made in other countries of sub-Saharan Africa [11-13]. The predominant marital status in the study may be related to the lack of financial means, marriages in civil status previously requiring a customary marriage which is usually very expensive in our country. The small percentage of women employed in sub- Saharan Africa in general and in Congo in particular could explain the high number of unemployed women in the study. The same observation was made by Noubiap et al. in Cameroon in 2015 and Mulu et al. in Ethiopia in 2014 [14,15]. College-level women were the most represented, this confirms the average level of education of Congolese as reported by the Demographic and Health Survey of Congo [16].
The predominance of scarification could be explained by the fact that this ancient practice is very widespread in our country. It was also one of the most important risk factors in a 2013 study on the prevalence of hepatitis B, C and HIV in pregnant women in Brazzaville [8]. The low immunization coverage could be explained by the lack of knowledge about vaccination in the general population, since the Expanded Program on Immunization was systematic only in 2012.
Our analyzes show that the carrying frequency of HBV is low. area of high prevalence of HBV infection such as Congo would be expected to have a higher frequency. In fact, higher prevalences of HBsAg have been reported in earlier work in pregnant women in Brazzaville and in women who gave birth in Pointe-Noire [8,9,17].
The high percentage of HBV in pregnant women aged 15 to 25 may be explained by the fact that this age group is more exposed to risk factors, especially sexual risk. The same observation was made by Ugbebor et al. in 2011 in Benin, Onwuiri et al. in 2017 and Esan et al. in Nigeria in 2014 [12,18,19]. The lack of sufficient knowledge about this infection would explain the high percentage among women with average education. The explanation is the same for housewives who are more exposed to HBV.
The high percentage of scarified patients is justified by the fact that this ancestral practice, usually used in sub-Saharan Africa and Congo in particular, is a frequent mode of contamination in these highly endemic areas. However, we found no statistically significant difference between the carriage of the virus and the variables studied.
Conclusion
Our study reported a low frequency of HBsAg in pregnant women in Pointe-Noire. These results require large-scale studies to determine the true HBV carriage rate in this population. Nevertheless, preventive and educational measures of the population on the modes of transmission of the virus as well as the systematic and early screening of pregnant women are necessary.
References
- World Health Organization. Prevention, Care and Treatment of Viral Hepatitis in the African Region: Addis Ababa, 2016- 2020 Framework for Action.
- Ghoma Linguissi LS, Celine Nguefeu Epidemiology of Viral Hepatitis in the Republic of Congo Review. BMC Research Notes. 2017; 10: 1-7.
- Mohammed S, Khalki H, Benbella I, et al. Seroprevalence of HBsAg in pregnant women in central Morocco. Pan African Medical Journal. 2016; 24: 1-5.
- Yohannes Z, Mulu W, Yimer M, et al. Sero-prevalence and risk factors of hepatitis B infection among pregnant women in Bahir Dar city, NW Ethiopia Cross sectional study. Pan African Medical Journal. 2015; 21: 1-7.
- Sogni P. Viral hepatitis and pregnancy. Hepato 2013; 20: 595-600.
- Petrova M, Kamburov Breastfeeding and Chronic HBV infection clinical and social implications. World J Gastroenterol. 2010; 16: 5042-5046.
- Towell V, Cowie Hepatitis B serology. Reprinted from Australian family physician. 2012; 41: 212-214.
- Angounda BM, Bokilo-Dzia A, Boumba A, et al. Prevalence of Serologic Markers and Risk Factors for Hepatitis B Viruses among Pregnant Women in Brazzaville, International Journal of Science and Research (IJSR). 2013; 14611: 2319- 7064.
- Itoua-Ngaporo A, Sapoulou MV, Ibara JR, et Prevalence of viral hepatitis B markers in a population of pregnant women in Brazzaville Congo. J Gynecol Obstet Biol Reprod Paris. 1995; 24: 534-536.
- Andzi Viral Hepatitis B Seroprevalence and Molecular Biodiversity in the Likouala Department of Congo. [Thesis # 1031: Med] Brazzaville: UMNG FSSA. 2016.
- Nelson J, Fomulu Frederick LI, Morfaw Torimiro NJ, et al. Prevalence, correlates and pattern of Hepatitis B among antenatal clinic attenders in Yaounde-Cameroon Is perinatal transmission of HBV neglected in BMC Pregnancy and Childbirth. 2013; 13: 1-10.
- Ose Ugbebor, Moses Aigbirior, Favor Osazuwa, et al. The prevalence of viral hepatitis B and C infections among pregnant North American Journal of Medical Sciences. 2011; 3: 238-241.
- Acept, Yesuf A, Alagaw A. Seroprevalence of Hepatitis B virus surface area and associated factors in Dawuro zone, SNNPR, Southwest Ethiopia: a cross sectional study. BMC Res Notes. 2017; 10: 418.
- Noubiap JJ, Nanseu JR, Chokfe N, et Prevalence, Infectivity and Correlates of Hepatitis B Infection Among Rural Women in Rural District of Far North Region of Cameroon. BMC Public Health. 2015; 15: 454.
- Zenebe Y, Mulu W, Yimer M, et al. Seroprevalence and risk factors of hepatitis B virus and human immunodeficiency virus infection among pregnant women in Bahir Dar city, NW Ethiopia a cross sectional study. BMC Infectious Diseases. 2014; 14: 118.
- National Center for Statistics and Economic Studies (CNSEE) and OCR Macro 2006. Demographic and Health Survey of Congo (EDSC-I) 2005. Calverton, Maryland, USA: CNSEE and OCR Macro.
- Bossali F, Taty-Taty R, Houssissa P, et al. Seroprevalence of co-infection with hepatitis B, hepatitis C and HIV in women delivered at the maternity ward of the Adolphe Sicé hospital in Pointe-Noire in 2010. African Journal of Hepato- Gastroenterology. 2012; 6: 315-319.
- Onwuiri FC, Ndako JA, Onwuliri Prevalence of Hepatitis B Virus Hbv and Hepatitis C Virus Hcv and their effects on serum albumin and liver aminotransferases in pregnant women in Jos. Virology Research and Reviews. 2017; 1: 1-4.
- Esan AJ, Omisakin CT, Ojo-Bola T, et al. Sero- Prevalence of Hepatitis B and Hepatitis C Viral Co-Infection among Pregnant Women in American Journal of Biomedical Research. 2014; 1: 11-15.