The Added Value of Gated- SPECT Myocardial Perfusion Imaging Amongst the Elderly and Very Elderly Patients
Author(s): Adriana C Puente-Barragán*, Rizo-Bermudez F, and Lilian G Delgado-Espejel
Nuclear Medicine Department, Centro Médico Nacional “20 de Noviembre”, ISSSTE, Félix Cuevas 540 Col. Del Valle Del. Benito Juárez, C.P. 03100, México.
*Correspondence:
Adriana C Puente-Barragán, Nuclear Medicine Department, Centro Médico Nacional “20 de Noviembre” ISSSTE, Félix Cuevas 540 Col. Del Valle Del. Benito Juárez, C.P. 03100, México, D.F.
Received: 17 January 2020; Accepted: 15 February 2020
Citation: Adriana C Puente-Barragán, Rizo-Bermudez F, Lilian G Delgado-Espejel, et al. The Added Value of Gated-SPECT Myocardial Perfusion Imaging Amongst the Elderly and Very Elderly Patients. Cardiol Vasc Res. 2020; 4(1); 1-5.
Abstract
Background: Myocardial perfusion g-SPECT method in the diagnosis and decision making in the very elderly (>75) remains scarce in its evidence. We conducted research to evaluate the added value g-SPECT perfusion in the diagnosis, risk stratification and decision making in patients with suspected or diagnosed coronary artery disease (CAD).
Methods and Results: We retrospectively evaluated the results of 183 patients aged ≥65 years with clinical suspected CAD. Exclusion criteria: structural heart disease, dilated-hypertrophic myocardiopathy, hemodynamic instability. G-SPECT: Technetium-99m sestamibi (8 mCi rest-16 mCi stress); stress test according clinical conditions (pharmacological, only stress or mixed). Imaging acquisition: SIEMENS®-Symbia-S equipment with IQ-SPECT technology, and evaluated subjectively in 17 segment analysis. Mean age was 72 ± 5.50 years old (88% 65-79 and 12% >80); 126 (70%) had ischemia: 63 (65%) mild, 51 (28%) moderate, and 12 (7%) severe; 28% with FEVI>45%. Twenty one (33%) with moderate or severe ischemia were derived to catheterization; 12 underwent stent placement, 2 surgical revascularization; and, 7 continued medical treatment.
Conclusion: G-SPECT, even conducting with stress, is a safety non-invasive test with high diagnosis accuracy in the very elderly. It adds value in the decision making and reduces the risk of referring unnecessary catheterization, represents a gatekeeper option and a turn for better prognosis.
Keywords
Introduction
Globally, deaths from cardiovascular disease are increasing; in particular, due to the aging population [1]. Between 1990 and 2013, the number of global deaths caused by cardiovascular disease has increased by 41% [2]. As a result of aging of the population, more elderly patients are referred for diagnostic and prognostic cardiac evaluation. Stress myocardial perfusion imaging (MPI) is useful for the evaluation of coronary artery disease (CAD) in elderly patients [3,4].
Despite of this betterment of our health status, non-communicable diseases predominate and are the leading cause of morbi-mortality; particularly, atherosclerotic cardiovascular diseases (CVD) and ischemic disease [5]. In this setting, 80% of patients with heart failure and 60% of those who had suffered a myocardial infarction are people of 60 years old and older [6].
Thus, as the population grows older worldwide, and CAD remains the leading cause of morbidity and mortality, there is an imminent need to identify effective methods of cardiovascular risk stratification which may direct management decisions in such patients. In this setting, the diagnostic value of Single Photon Emission Computed Tomography Myocardial Perfusion Imaging (SPECT MPI) in the general population is well understood [7-9]; nevertheless, the role of this non-invasive technique in the elderly population remains scarce, particularly in octogenarians [10,11].
In this regard, since a considerable proportion of elderly patients cannot perform adequate exercise stress test, solid evidence has shown the usefulness of pharmacological stress with dipyridamole g-SPECT stress myocardial perfusion imaging for clinical diagnosis and also, prognosis in patients aged 70 years and older [12]. Still, little research has been conducted in adequate exercise stress test performance. Therefore, clinical decisions on whether pursue non-invasive versus invasive management, particularly in the presence of abnormal myocardial perfusion imaging, is crucial to address quality of life and prognosis rather than only prolongation of life amongst increasing elderly population [7].
The aim of the present study was to evaluate the added value of gated myocardial perfusion single-photon computed tomography (g-SPECT) in the diagnose, risk stratification and decision making in patients aged 60 years and older with suspected or diagnosed (CAD) performing all stress tests types, exercise and/or pharmacological, depending on patients’ physical capability.
Patients and Methods
We searched patients’ records aged 60 years and older that were clinically referred to undergo stress 99mTc-Sestamibi g-SPECT for the evaluation of suspected or known CAD; patients with history of coronary artery disease were assessed for risk stratification and control after a revascularization. A total of 183 patients met these criteria within a six month period. Excluded patients were those with any of the following at the time of MPI: structural heart disease, dilated or hypertrophic myocardiopathy, cardiac failure; and, haemodynamic instability.
We evaluated clinical characteristics, history of cardiovascular events and risk factors as hypertension (defined as systolic blood pressure ≥130 mmHG and diastolic pressure ≥80mmHg); dyslipidaemia (cholesterol levels ≥200 mg/dl and c-LDL ≥ 130 mg/dl triglycerides ≥ 150 MG/dl; diabetes (A1C ≥ 6.5% or fasting plasma glucose ≥ 100 mg/dl); and, smoking.
This study was approved by the institutional ethics committee at the National Medical Center “20 de Noviembre”, ISSSTE.
Nuclear screening and Image Acquisition
All 183 patients were non-invasively assessed through one-day protocol g-SPECT rest-stress. Rest/stress MPI was performed with Tc99m Sestamibi in a 1-day protocol following the American Society of Nuclear Cardiology protocols (ASNC) [13]; and, American Heart Association (AHA) consensus [14]. The stress testing was determined by the nuclear cardiologist based on each patient’s clinical history, physical exploration, patients’ functional capacity; and, general condition. Stress protocol was conducted through physical exercise, pharmacological vasodilation with dipyridamole, or physical and pharmacological (mixed stress).
The perfusion images were acquired in synchronization with the patient's electrocardiogram (g-SPECT); this allowed us to study not only the left myocardial perfusion, but also the function (left ventricle ejection fraction), wall motion, and systolic wall thickness.
We utilized a gamma camera SIEMENS®-Symbia-S, with IQ- SPECT technology (dual head) and collimators SMATRZOOM with acquisition of 32 images (in 180º elliptical orbit from 45º right anterior oblique to 45º left anterior oblique, in step and shoot mode); allowing the use of radiotracer lower doses and the acquisition of high quality imaging in less time than older technology (4 minutes).
Image Processing and Data Analysis
All 183 g-SPECT myocardial perfusion imaging (MPI) studies were analysed by two experienced nuclear cardiologist physicians who were blinded to perfusion results (Kappa intra e inter-observer 0.92). Reconstruction and image processing were generated as ordinary: short axis, vertical long axis and horizontal long axis. For qualitative analysis, perfusion g-SPECT studies were assessed visually, using the 17-segment model rated based on the severity of perfusion defects, in a visual 5-point scale, where 0 denotes normal perfusion, 1 mild perfusion defect, 2 moderate defects, 3 severe perfusion defect and 4 denotes absence of perfusion. Necrosis was indicated at the presence of a perfusion defect in the rest images, and was defined as transmural (severe defect or absence of perfusion), and nontransmural (moderate perfusion defect).
Ischemia was indicated where the presence of a reversible defects, which refers to a perfusion defect present in stress that resolved at rest in the same segment; and, was rated as mild, moderate and severe level of ischemia.
Statistical analysis
Continuous data were expressed as mean ± SD, and percentages were rounded. Discrete or dichotomized variables were compared using Chi-square or Fisher’s exact tests and continuous variables using Student’s t-tests for unpaired samples. A p value <0.05 was considered statistically significant. All statistical analyses were 2 tailed and performed using SPSS version 21 [15].
Results
One hundred eighty-three patients’ records met the inclusion criteria and were examined from the Nuclear Medicine Department. Patients’ average age was 72 ± 5.50 years within a range of 69-85 years old. Table 1. Baselines characteristics and cardiovascular risk factors by groups and Figure 1. Gated-SPECT myocardial perfusion study indications by groups shows variables divided into two groups defined as elderly those from 65 to 79 years old and very elderly who were those at the age of 80 or more years old.
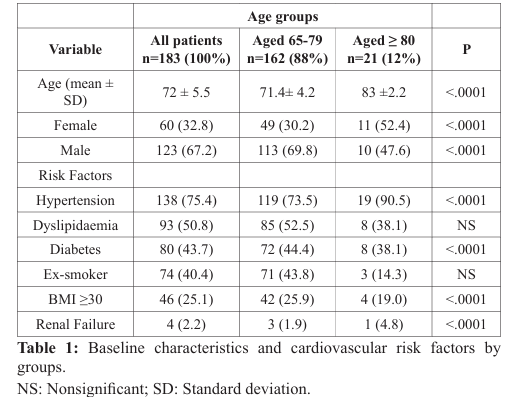
The indications for the performance of the myocardial perfusion study with g-SPECT in both groups of patients were multiple.
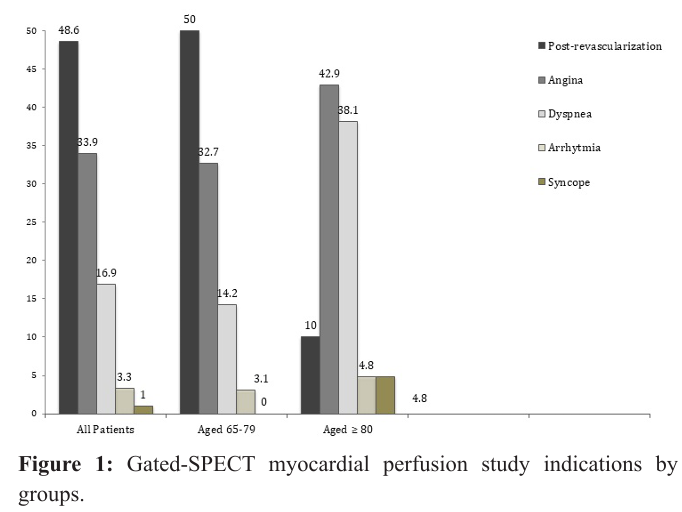
In general, the most frequent indication was control study as part of the clinical follow-up in patients with a history of revascularization (post-revascularization) which predominated in the group of elderly patients (50%); in the very elderly group the most frequent indication was the presence of typical angina (42.9%).
The vast majority of patients (96.2%) performed the one-day protocol including stress phase. According to their clinical conditions, 60.2% performed mixed stress (dipyridamole + physical stress); 38.6% dipyridamole; and, only 1.2% performed only exercise in treadmill. In the elderly group, 60.3% patients performed a mixed stress protocol, while most of the patients in the very elderly group underwent a pharmacological stress with dipyridamole (62%). There were no complications or related adverse events during the performance of the stress phase. The MPI was abnormal in all patients. When subjectively evaluating the degree of ischemia, the majority presented mild ischemia(67.6%), 25% had a moderate degree and only 7.4% had severe grade ischemia; 29.5% of the group in general showed a decrease in post-exercise LVEF (Table 2).
According to the findings of myocardial perfusion, 33.5% and 23.8% of the patients belonging to the elderly and very elderly group respectively had a high-intermediate post-test risk
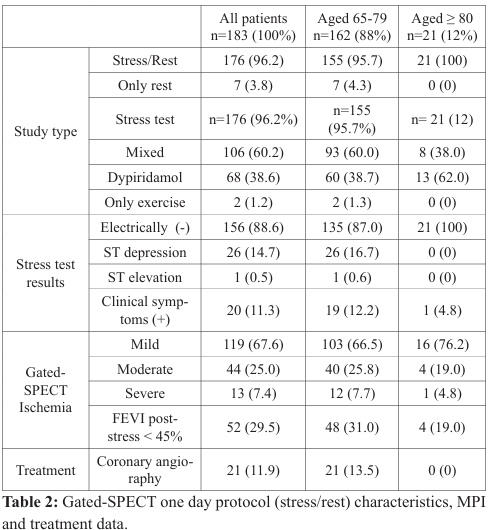
According to the myocardial perfusion results, 21 (13.5%) elderly patients with moderate to severe ischemia were referred for coronary angiography; from who 12 (57.1%) underwent percutaneous coronary intervention with stent and only two (9.5%) had revascularization surgery; the other 7 (33.4%) continued with medical treatment due to coronary anatomy (Figure 2).
On the other hand, the vast majority of very elderly patients (76.2%, n=16) presented mild ischemia and five patients (23.8%) had moderate to severe ischemia. All very elderly patients were conservatively treated.
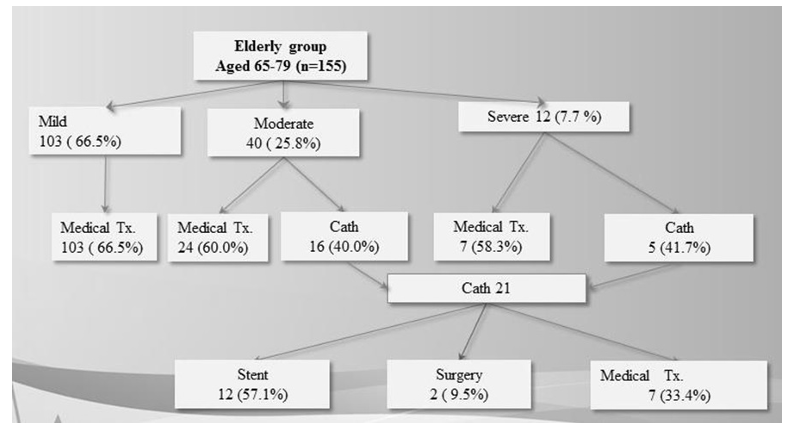
Figure 2: Decision making and treatment according myocardial perfusion imaging data.
Discussion
Worldwide, rates of cardiovascular diseases continue to increase and their impact on medical practice is huge. Important differences should be taken into account in elderly patients with CAD as compared with their younger counterparts: symptom presentation may be different, and complex coronary lesions, coexisting illness, and functional limitations are more prevalent; and, the risk of revascularization procedures is generally increased [16]. In this context, a diagnosis of only coronary anatomy is not sufficient, and the prognostic estimation in a given patient is of utmost importance in the management of older elderly patients with CAD [17]. Other prospective studies focus their primary goal of treatment in elderly and very elderly patients to be not only the prolongation of life, as in younger patients, but rather the improvement in the quality of life. Our results demonstrate that stress myocardial SPECT successfully stratified the risk for subsequent cardiac events [18] and also are consistent with literature in terms of the added value of risk stratification after g-SPECT protocol is performed.
In addition, prior studies have found that stress diagnostic and stratification tests are not conducted in the elderly and; much less, in the very elderly population due to aggregated comorbidities; and thus, complications and adverse events increment during the process [19]. The current study proves well that stress test could be thoroughly conducted in elderly and very elderly people with suspected and/or history of coronary artery disease. Another important finding is that 12% of our sample was ≥80 which indicates that even in this particular group stress stratification test is also possible to be safely conducted.
We conducted protocols as follows: 60.2% of stress tests were mixed, 38.6% induced with dipyridamole, and two (1.2%) patients were able to do the complete exercise treadmill test. The vast majority of patients were favoured by the vasodilator alone or in combination with slight exercise (walk) in order to conduct a thorough and valid g-SPECT results interpretation; the most important clinical finding was to prove that this option is an added value and a benefit for clinicians to properly evaluate myocardial perfusion in the very elderly and the elderly who commonly present comorbidities that limit the ability to do an effective physical stress.
As shown in the results, the vast majority of the total sample (n=156, 88.6%) had a clinical and electrical negative result, only 26 (14.7%) presented significant ST segment depression, and 20 (11.3%) develop angina equivalent symptoms during the stress test. It is important to mention that no patient presented or develop related adverse events or complications.
Myocardial perfusion was positive in all patients according to SPECT results. In the elderly group, 66.5% had mild, 25.8% had moderate, and 7.7% had severe ischemia; from the very elderly group, 76.2% had mild, 19% had moderate, and only one patient(4.8%) had severe ischemia. A third of the elderly group of patients (n=48, 31%) and 4 (19%) of the very elderly presented a decrease of left ventricular ejection fraction (LVEF), which added evidence to correctly and safely stratify them in intermediate to high post-test risk. Therefore, treatment was indicated according to the diagnosis for each patient.
From all 183 patients, 21 (11.4%) from the elderly group with moderate to severe ischemia were referred to catheterization; 12 of them underwent stent placement and 2 patients to surgical revascularization, seven continued with medical treatment. None of the very elderly was referred to catheterization, since all were low to intermediate risk and received medical treatment.
In the aging population, CAD is a major health problem, and cardiovascular disease is still the leading cause of mortality in elderly patients. As a result, elderly patients with known or suspected CAD are frequently encountered in a nuclear cardiology practice. Stress MPI is an important non-invasive technique for the evaluation of patients with known or suspected CAD, also in the control after revascularization and after myocardial infarction. Elderly patients are frequently unable to perform an exercise test due to several comorbidities (e.g. obstructive lung disease, peripheral vascular disease, poor functional capacity or clinical conditions); however, our study shows evidence that in patients with hemodynamic stability is possible to perform stress with physical exercise, or undergoing mixed test, which relevant use is that stress phase is induced trough the dypiridamol and little physical exercise. Taken together these results show that if stress test protocol is effectively chosen according to each patient history, symptoms and comorbidities, diagnostic and prognostic efficacy is achieved regardless the age. More important, treatment decision making is clearer and all available options as catheterization and further revascularization. Therefore, g-SPECT is the door for therapeutic routes and decision making regardless the age.
Conclusion
The main finding of this study is that g-SPECT proves to be an effective, accurate and safe prognostic tool for the elderly; and moreover, for the very elderly population. Given the fact that myocardial ischemia is very frequent in 60 years old and more population and based on present results, gated-SPECT seems to add value in the diagnosis and decision making process in the elders and even in the very elders.
This non-invasive cardiovascular imaging assessment is very accurate; and more important, is safe even in very elderly patients undergoing whether the mixed protocol or vasodilator alone protocol reducing the risk of referring a patient to an unnecessary catheterization. Therefore, myocardial perfusion with gated- SPECT represents to be a gatekeeper option and a turn for better prognosis risk stratification. The added value of the mixed protocol, the combination of induced dypiridamol along with low- level exercise represents a powerful alternative in the elderly and very elderly population.
References
- https://apps.who.int/iris/handle/10665/44203.
- Gregory A. Roth, Mohammad H. Forouzanfar, Andrew E. Moran, et al. Demographic and Epidemiologic Drivers of Global Cardiovascular Mortality. The New England Journal of Medicine. 2015; 372: 1333-1341.
- Pasquale Perrone-Filardi, Pierluigi Costanzo, Santo Dellegrottaglie, et al. Prognostic role of myocardial single photon emission computed tomography in the elderly. Journal of Nuclear Cardiology. 2010; 17: 310-315.
- Olivier De Winter, Nico Van de Veire, Filip Gemmel, et al. Myocardial perfusion imaging in the elderly: a review. Nuclear Medicine Communications. 2006; 27: 529-534.
- Karen Yeates, Lynne Lohfeld, Jessica Sleeth, et al. A global perspective on cardiovascular disease in vulnerable populations. Canadian Journal of Cardiology. 2015; 31: 1081-1093.
- Aakriti Gupta, Yongfei Wang, John A Spertus, et al. Trends in Acute Myocardial Infarction in Young Patients and Differences by Sex and Race, 2001 to 2010. 2014; 64: 337-345.
- Tadashi Nagao, Taishiro Chikamori, Satoshi Hida, et al. Quantitative Gated Single-Photon Emission Computed Tomography With 99mTc Sestamibi Predicts Major Cardiac Events in Elderly Patients With Known or Suspected Coronary Artery Disease. Circ J. 2007; 71: 1029-1034.
- Zhiming Yao, Hui Zhu, Wenchan Li, et al. Adenosine triphosphate stress myocardial perfusion imaging for risk stratification of patients aged 70 years and older with suspected coronary artery disease. J Nucl Cardiol. 2017; 24: 429-433.
- Su Jin Lee, Kyung-Han Lee, So-Mi Park, et al. Myocardial perfusion defects and coronary risk factors in symptomatic and asymptomatic elderly women. Int J Cardiovasc Imaging. 2008; 24: 277-281.
- Francesco Nudi, Giuseppe Biondi-Zoccai, Orazio Schillaci, et al. Prognostic accuracy of myocardial perfusion imaging in octogenarians. J Nucl Cardiol. 2018; 25: 1342-1349.
- Sanjeev U Nair, Alan W Ahlberg, Shishir Mathur, et al. The clinical value of single photon emission computed tomography myocardial perfusion imaging in cardiac risk stratification of very elderly patients (≥80 years) with suspected coronary artery disease. Journal of Nuclear Cardiology. 2012; 19: 244-255.
- Xichun Sun, Aibo Liu, Zhonghua Jiang, et al. The sensitivity and specificity of single photon emission computed tomography (SPECT) in the diagnosis of coronary artery disease (CAD): a meta-analysis. Int J Clin Exp Med. 2017; 10: 6221-6236.
- Robert C Hendel, James R Corbett, S James Cullom, et al. The value and practice of attenuation correction for myocardial perfusion SPECT imaging: a joint position statement from the American Society of Nuclear Cardiology and the Society of Nuclear Medicine. Journal of Nuclear Cardiology. 2002; 9: 135-143.
- Ryan TJ, Anderson JL, Antman EM, et al. ACC/AHA guidelines for the management of patients with acute myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute Myocardial Infarction). Journal of the American College of Cardiology. 1996; 34: 1328-1428.
- IBM. Statistical Package for the Social Sciences. Vol. 20.
- Michelle C Odden, Pamela G Coxson, Andrew Moran, et al. The Impact of the Aging Population on Coronary Heart Disease in the United States. American Journal of Medicine. 2011; 124: 827-833.
- Mahesh V Madhavan, Bernard J Gersh, Karen P Alexander, et al. Coronary Artery Disease in Patients >80 Years of Age. Journal of the American College of Cardiology. 2018; 71: 2015-2040.
- Lisa L Schlitzkus, Alyson A Melin, Jason M Johanning, et al. Perioperative Management of Elderly Patients. Surgical Clinics of North America. 2015; 95: 391-415.
- Gerald F. Fletcher, Gary J. Balady, Ezra A. Amsterdam, Exercise Standards for Testing and Training. Circulation.