The Comparative Analysis of Obesity Risk Factors among Indian and Ukrainian Adolescents
Author'(s): Starets O, Khimenko T, Kaur N* and Bharadwaj O
Department of Pediatrics, Odessa National Medical University, Ukraine
*Correspondence:
Navneet Kaur, Odessa National Medical University, Tel: +380636359605; E-mail: navi.boparai7@gmail.com.
Received: 01 August 2018 Accepted: 29 August 2018
Citation: Starets O, Khimenko T, Kaur N, Bharadwaj O, et al. The Comparative Analysis of Obesity Risk Factors among Indian and Ukrainian Adolescents. Diabetes Complications. 2018; 2(3): 1-3.
Abstract
Childhood obesity is one of the most serious public health challenges affecting many low-income and middle-income countries. The aim was to analyze risk factors like bad feeding culture and sedentary lifestyle and how they correlate with general health disorders in children and their parents. The study was held in two schools of India and two schools of Ukraine, contains total 202 observations. Analysis of parent's questionnaires revealed that 71%, 95% CI (58.62; 81.16) of Indian and 64%, 95% CI (54.86; 72.96) of Ukrainian families think that their budget is not enough. Obesity in parents was documented in 22%, 95% CI (12.75; 35.24) in India and 54%, 95% CI (40.07; 68.29) in Ukraine. As per analysis of children questionnaires, we found that fast food intake was significantly frequent in India 80%, 95% CI (71.65; 86.93) versus 13%, 95% CI (8;21.59) in Ukraine. While in results of the correlation of orthostatic complaints with sedentary lifestyle OR 5.9 95% CI (2;17) headache OR 2.8 95% CI (1.1;6.5), dizziness after playing OR 3.4 95% CI (1.4;8) in Indian children on contrary stomachache OR 5.2 95% CI (2;13) in Ukrainian. The study disclosed the enhancing factors of childhood obesity in both populations. Etiology of disease is multifactorial and complex, therefore an organized and advance approach of prevention is recommended.
Keywords
Introduction
In modern era, childhood obesity is the most complex hindrance in a path towards healthy society, as it is highly influenced by race, ethnic, socioeconomic and hereditary factors [1]. In U.S. the prevalence of obesity has increased dramatically in school- aged children (age, 6-11 years) and adolescents (age, 12-19 years) between 1976 and 1980 and between 2009 and 2010 (from 6.5% to 18.0% in children and from 5.0% to 18.4% in adolescents), generally children carry their adiposity to adulthood [2,3]. The literature review and current findings showed the obesogenic environment and Nutrient density being the main factors include higher caloric consumption and decrease caloric expenditure due to low physical activity, inadequate intake of essential macronutrients, and excessive utilization of unsaturated fatty acids. Children need nutrient-rich foods rather than high-energy foods [4]. Urbanization provides fewer open and safe spaces and playgrounds along with that increasing pressure on children to perform in academics and reduced emphasis on sports. Especially in South-Asian countries such as India, sociocultural beliefs against sports and outdoor physical activity by girls is a reason behind high percentage of sedentary lifestyle among girls, whereas according to WHO European region study, prevalence of 15% and more among 15-year-old girls was found only in Ukraine [5,6]. High socioeconomic status of family lead to daily allowance (pocket money) to purchase lunch, impressed by the marketing advertisements of fast food children usually prefer such foods. The study exhibited the similar findings, revealed in previous study of India that children having sedentary activity more than 90 minutes are on 19.6% higher risk of getting obesity as compared to children who watch T.V less than 45 minute. Evidenced-based prevention of childhood obesity showed that most beneficial prevention programs are those that focus on a collaboration of community/ school, primary health care, and family based interventions that involve both a physical activity and dietary component [7]. Recently the World Health Organization recommended that free sugars should account for no more than 10% of daily energy intake [8]. This has not been universally accepted, particularly from within the food industry [9]. Reducing easy access to energy dense foods may help to limit the opportunities for overeating [10].
Materials and Methods
The study was held on the base of university child health clinic no.1, Mariinsky gymnasium and school no.121 of Odessa region of Ukraine, while in India it was done on the base of senior secondary school Bahadurgarh, Punjab, Zila parishad and St. judes high school of Hyderabad, and it lasts for 3 years from September 2015 until April 2018. The research included 100 number of observations from Ukraine and 102 from India (102 boys and 100 girls). The criteria of including into the research were children should be of 10-18 years of age, permitted by their parents and without any acute diseases, trauma and fever. The research was divided into three stages. Stage 1 consist of questionnaires for children and parents, with questions about anamnesis, level of nutrition of child, level of physical activity of child and children and their parents view about role of physical activity in their life. In stage 2 the observant went under general examinations: anthropometry, blood pressure and pulse measurement, orthostatic test. Stage 3 included correlation of various factors from questionnaires and physical examination. The anthropometric data was thoroughly correlated with Standard Deviation (z-score) tables and Percentile tables (software “WHO Anthro Plus”), blood pressure was done by the Percentile tables for age 1-17 for boys and girls (provided by the Task Force on Fourth Report OF Diagnosis, Evaluation and Treatment of High Blood Pressure in Children and Adolescents) and pulse was analogized with Percentile tables for age 0-80 years for both males and females (provided in the National Health Statistic Report of U.S survey of 2008). Statistical analysis comprised the mean value (M), standard deviation (SD), 95% confidence interval (CI), odds ratio (OR).
Results
The analysis of parent’s questionnaires revealed that 71%, 95% CI (58.62; 81.16) of Indian and 64%, 95% CI (54.86; 72.96) of Ukrainian families think that their budget is not enough. Such complaints like headache and stomachache were significantly more often observed in Ukrainian children in 82%, 95% CI (74.02; 88.13) and 58%, 95% CI (48.78; 66.76) relatively versus 55%, 95% CI (43.34; 66.83) and 14%, 95% CI (7.46; 24.27) of Indian (Figure 1).
Obesity in parents was documented in 22%, 95% CI (12.75; 35.24) in India and 54%, 95% CI (40.07; 68.29) in Ukraine. Children who doesn’t complete their meals were more often seen in Ukraine 72%, 95% CI (63.44; 79.99) versus 37%, 95% CI (26.23; 49.08) in India. Children not interested in sports are 48%, 95% CI (37.02; 59.62) in India versus 17%, 95% CI (11.45; 25.63) in Ukraine. As per analysis of children questionnaires, we found out that fast food intake was significantly frequent in India 80%, 95% CI (71.65; 86.93) versus 13%, 95% CI (8.0; 21.59) in Ukraine. Sedentary
lifestyle was seen in 34%, 95% CI (25.82; 43.95) of Indian and 19%, 95% CI (12.78; 28.31) of Ukrainian children. Complaints after playing were seen in 41%, 95% CI (32.12; 50.88) of Indian and 14%, 95% CI (8.70; 22.56) of Ukrainian children.
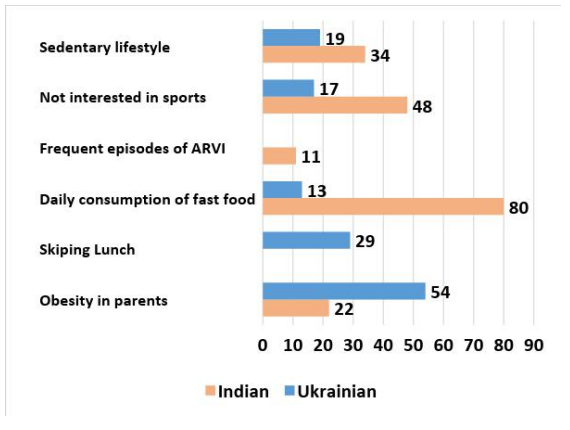
Figure 1: Results of analysis of Parents and children questionnaires
Abbreviation: ARVI: Acute Respiratory Viral Infection.
Studying the data of general examination we unveiled the prevalence of overweight children in Ukraine 24%, 95% CI (17.04; 33.86) (Figure 2), whereas in India the prevalence of underweight children 49%, 95% CI (39.53; 58.58) was documented (Figure 3).
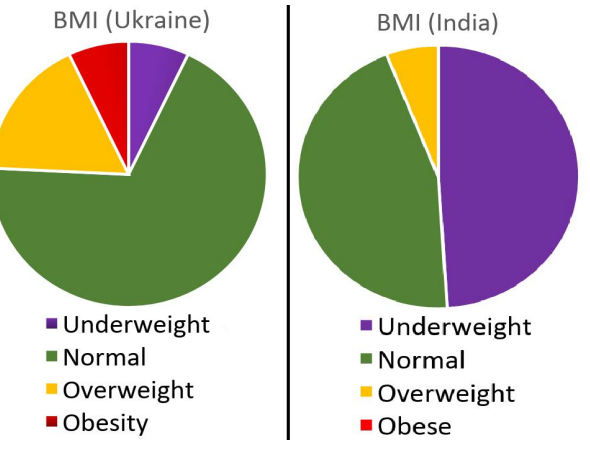
Figure 2: Body Mass Index (BMI) of Ukrainian population.
Figure 3: BMI of Indian population.
The risk of pre-hypertension was more often seen in Indian subjects 17%, 95% CI (11.46; 26.18) than Ukrainian – 10%, 95% CI (5.70; 17.95). The results of resting pulse analysis showed the prevalence of children with resting tachycardia in India 17%, 95% CI (10.67; 25.08) versus 11%, 95% CI (6.73; 19.95) in Ukraine. No significant deviations in results of orthostatic test were recorded. In Ukrainian children in orthostatic test, the difference in number of beats between Ps1 and Ps3 was less than 10 bpm (beats per minute) in 68%, 95% CI (58.34; 76.33) between 10-20 bpm in 25%, 95% CI (17.55; 34.30) and more than 20 bpm in 7%, 95% CI (3.43; 13.75) while in Indian less than 10 bpm in 75%, 95% CI (66.32; 82.81), between 10-20 bpm in 17%, 95% CI (10.67; 25.08) and more than 20 bpm in 8%, 95% CI (4.03; 14.72). While formulating the results of stage 3 (Table 1) we observed that the orthostatic complaints correlate with sedentary lifestyle OR 5.9 95% CI (2.0-17.1), headache OR 2.8 95% CI (1.1-6.5), dizziness after playing OR 3.4 95% CI (1.4-8.0) in Indian children on contrary stomachache OR 5.2 95% CI (2.0-13.3) in Ukrainian. Particularly in Indian population complaints after playing correlates with less visit to sport section OR 2.8 95% CI (1.2-6.4) and orthostatic complaints OR 2.35 95% CI (1.0-5.3). Obesity in parents highly correlates with good social status of family in both populations, in Indian OR 4.2 95% CI (1-14.7), in Ukrainian OR 4.1 95% CI (1.5-11.3).
High magnitude of correlation was found between less episodes of respiratory illness and good intake of fresh food among both populations, in Indian OR 6.3 95% CI (1.6-25.7), in Ukrainian OR 18.2 95% CI (4.8-69.3).
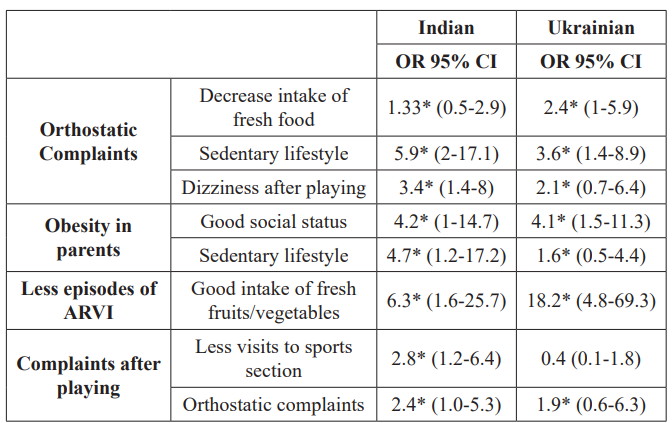
Table 1: Results of analysis of correlation of factors.
Abbreviations: CI: Confidence Interval; ARVI: Acute Respiratory Viral Infection; OR: Odds Ratio; *Statistical significance of OR.
Discussion
In the course of our research, we discovered that in both populations the orthosatstic problem has high magnitude of correlation with sedentary lifestyle, headache, and dizziness after playing. We revealed strong correlation between good intake of fresh fruits and vegetables and less episodes of respiratory illness and obesity in parents highly correlates with good social status of family and sedentary lifestyle in children. Evident from WHO European report the proportion of adolescents meeting MVPA guidelines significantly increased in Ukraine [6]. Despite the presence of numerous prevention programs of childhood obesity, the desirable decline in its prevalence is not achieved. Evidence suggested that physical activity interventions in a school-based setting with a family component or diet are more effective. More research is needed to test interventions in other settings, such as those testing policy, environmental, and consumer health informatics strategies [11].
Conclusion
The study disclosed the enhancing factors of childhood obesity in both populations. Etiology of disease is multifactorial and complex, as it originate from the reciprocal action of genetic, biological, environmental and ecological factors. An organized and advance approach of prevention is recommended with initial management being implemented in primary care and with focus on healthy eating habits and active lifestyle.
References
- Kumar S, Aaron S. Kelly Review of Childhood Obesity February. 2017; 92: 251-265.
- Ogden CL, Carroll MD, Kit BK, et al. Prevalence of obesity and trends in body mass index among US children and adolescents. 1999-2010. JAMA. 2012; 307: 483-490.
- Ogden CL, Flegal KM, Carroll, et Prevalence and trends in overweight among US children and adolescents. 1999-2000. JAMA. 2002; 288: 1728-1732.
- Lobstein T, Kevin D Hall, Steven L Gortmaker, et al. Child and adolescent obesity part of a bigger picture Lancet. 2015; 385: 2510-2520.
- Developing Countries Epidemiology Determinants and Prevention Endocrine Reviews. 2012; 33: 48-70.
- WHO regional office of Europe report Adolescent obesity and related behaviours trends and inequalities in the WHO European Region. 2002-2014.
- Thury C, de Matos CV. Prevention of childhood obesity a review of the current guidelines and supporting evidence. S D Med. 2015; 18-23.
- World Health Organization technical report series. Diet nutrition and the prevention of chronic diseases. Geneva WHO. 2003; 916.
- Kapp Brundtland meets food and drink leaders but declines Coke cocktail. Lancet. 2003; 361: 1707.
- Hill JO, Peters Environmental contributions to the obesity epidemic. Science. 1998; 280: 1371-1374.
- Wang Y, Wu Y, Wilson RF, et al. Childhood Obesity Prevention Programs: Comparative Effectiveness Review and Meta-Analysis Agency for Healthcare Research and Quality. US. 2013.