The Diet and Diabetes: A Focus on the Challenges and Opportunities within the Stroke Belt Dietary Pattern
Author'(s): Melissa Johnson*
1Tuskegee University, Department of Food and Nutritional Sciences, 207 Morrison-Mayberry Hall, Tuskegee, AL, 36088, USA.
*Correspondence:
Melissa Johnson, Tuskegee University, Department of Food and Nutritional Sciences, 207 Morrison-Mayberry Hall, Tuskegee, AL, 36088, USA, E-mail: mjohnson@mytu.tuskegee.edu.
Received: 12 August 2017 Accepted: 01 September 2017
Citation: Melissa Johnson. The Diet and Diabetes: A Focus on the Challenges and Opportunities within the Stroke Belt Dietary Pattern. Diabetes Complications. 2017; 1(3); 1-6.
Abstract
Diabetes mellitus, the most common type of endocrine disorder, globally affects over 400 million individuals and is steadily rising. Cultural and environmental norms that embrace or facilitate the lack of consistency in diet, lifestyle and behavioral patterns that promote health have inadvertently promoted and sustained a diabetogenic environment. Dietary patterns plentiful in processed foods, refined grains, sugar, sodium, fat and calories, coupled with modern conveniences that commission sedentary lifestyles have noticeably contributed to the diabetes epidemic as well. Like other chronic diet-related diseases, modifications of dietary intake and consumption patterns are necessary for diabetes prevention. Unfortunately, many modifiable and non-modifiable factors may hinder an individual’s ability to obtain an optimal diet for disease prevention and health promotion. This includes, but is not limited to, lack of access to affordable, nutrient-dense foods, geographical location, built environment and demographic characteristics. A prime example of this can be seen in the southeastern region of the United States known as the Stroke Belt, which exhibits exceptionally higher than national average prevalence rates of cardiovascular disease, stroke, diabetes and accompanying disparities in health. Major challenges to the dietary pattern of the Stroke Belt are food consumption behaviors and preparation methods. Promising opportunities with this dietary pattern are the presence of foods, rich in antioxidants and other bioactive compounds, which may reduce the inflammation and oxidative damage associated with disease pathogenesis.
Keywords
Introduction
It is estimated that more than 29 million U.S. adults have diabetes mellitus. Not surprisingly, complications of diabetes may affect every cell, tissue, organ and system in the body, and may lead to adverse cardiovascular, renal, microvascular and macrovascular outcomes [1-3]. Racial and geographical differences in diabetes prevalence have been observed, with a greater concentration of diabetes prevalence identified among African Americans and those living in the southeastern region of the United States, also referred to as the Stroke Belt [4]. The Stroke Belt, an 11-state wide region located in the southeastern portion of the United States (Alabama,
Arkansas, Georgia, Indiana, Kentucky, Louisiana, Mississippi, North Carolina, South Carolina, Tennessee and Virginia), is acknowledged as having the highest persistent prevalence rates of cerebrovascular disease (i.e. stroke) and mortality [5-7]. Further, the mortality associated with stroke is higher for African Americans living in the Stoke Belt as well as those living outside of the Stroke Belt [8]. Although much research has been conducted regarding health disparities within the Stroke Belt, there exists an immense opportunity to provide feasible and practical solutions to lessen the divide. Interventions to transform the modifiable risk factors for diabetes such as dietary intake would not only benefit individuals living in the Stroke Belt but others with similar demographic, socioeconomic and geographical risk profiles. This brief review examines the challenges and opportunities within the dietary pattern of Stroke Belt and its influence on type 2 diabetes.
The Stroke Belt
The Stoke Belt, appropriately named due to the disproportionately greater incidence and prevalence rates of cardiovascular disease, stroke, obesity and diabetes, demonstrates a dietary pattern unique to individuals living in the southeastern region of the United States. Race, socioeconomic status and chronic disease have been suggested to elucidate the excessive prevalence of disease in the Stoke Belt [9]. It has been suggested that living in the Stroke Belt during childhood may confer an additional risk for stroke, even after relocating out of the Stroke Belt [10]. Within the Stroke Belt is the “diabetes belt”, characterized by a greater prevalence of diagnosed diabetes particularly among African Americans demonstrating modifiable risk factors such as obesity (as a result of a primarily sedentary lifestyle), as well as community -level characteristics, persistent poverty, low socioeconomic status (SES), unemployment and inadequate fitness and recreational facilities [11]. Characteristics of the Stroke Belt that may contribute to increased risk for diabetes are illustrated in Figure 1.
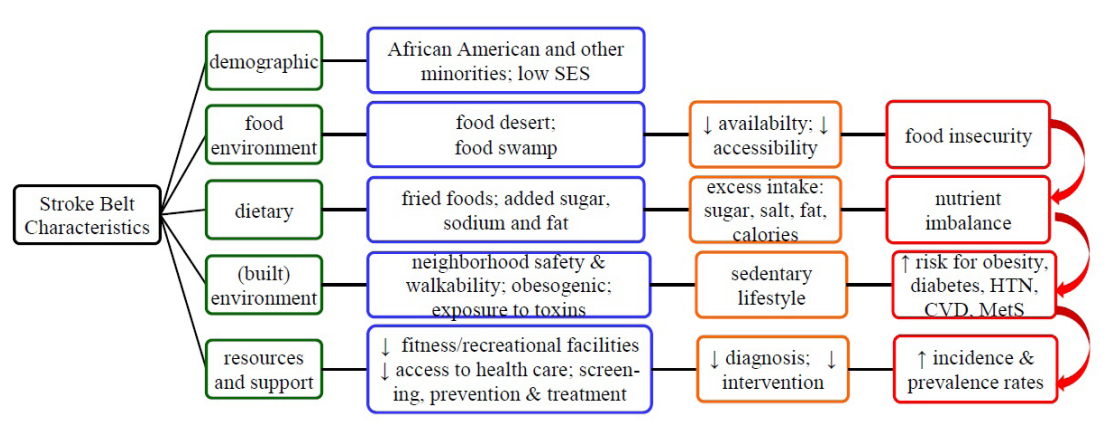
Figure 1: Select characteristics of the Stroke Belt that may contribute to diabetes risk, pathogenesis and adverse health outcomes.
The Dietary Pattern of the Stroke Belt
The relationship between diet and disease has long been studied, with more favorable, high quality dietary patterns containing whole grains, fruits, vegetables, and other plant-based foods being associated with decreased risk for diet-related disease [12-17]. In addition to the dietary composition, meal timing and frequency and environment, may set the stage for disease risk and pathogenesis [18-21]. Unfortunately, these risk factors may span across multiple generations, with offspring of at-risk mothers being at an increased risk for disease [22]. Further, living with a lower SES may considerably contribute to risk for disease by ultimately influencing dietary intake [23,24]. These risk factors may act in synergy within the Stroke Belt to further exacerbate disease risk.
The dietary pattern of the Stroke Belt may be viewed as the “soul food” or “Southern” pattern- rich, flavorful and abundant in added sugar, fat, fried foods, processed meats, animal products, sugar- sweetened beverages and calories [25]. Standard foods include processed meats, pork, poultry, ham hocks, chitterlings, catfish, fried pork cracklings (i.e. skin), and salty snacks, greens (collards, turnip, mustard), sweet potato pie and sugar sweetened tea [26]. Common food preparation techniques include deep frying, grilling, and the addition of pork (e.g. bacon, lard), salt and sugar. Conversely, this dietary pattern is associated with lower intakes of fruits, vegetables and whole grains [27]. Further combating this disparity is the limited access to quality foods, resulting in poorer diet quality [6,28,29]. Taken together, these characteristics labor additively and in synergy to further increase risk for diabetes mellitus, hypertension, stroke, cardiovascular disease and dyslipidemia [30]. Individuals consuming the Southern diet are at an increased risk for cardio-metabolic risks such as higher blood pressures, higher triglyceride levels, lower high-density lipoprotein (HDL) levels, abdominal visceral adiposity and metabolic syndrome [31]. In addition, the consumption of the Southern dietary pattern was associated with being African American, lower educational attainment, lower SES, higher likelihood of smoking, higher body mass index and physical inactivity [32].
Within the Stroke Belt, African Americans are likely to consume less dietary fiber, calcium, magnesium, potassium and iron and greater amounts of cholesterol and energy from carbohydrates [33,34]. In addition to African American race being an independent risk factor for diabetes, serum potassium was identified as an explanatory effect for diabetes risk [35]. Novel diabetes risk factors among African Americans include lifestyle, physiologic and environmental factors that impact African Americans more than others [35].
Challenges within the Dietary Pattern of the Stroke Belt
Traditional dietary components of the Stroke Belt include, but are not limited, to green leafy vegetables (e.g., collard greens, turnip greens, mustard greens), starchy vegetables (e.g., corn, sweet potatoes, white potatoes), dried beans (e.g., lima, butter, kidney, navy, black-eyed), grains (rice, grits, macaroni, cornbread), breaded and fried meats and milk (whole, buttermilk) [37]. Regional variations in food preparation methods and consumption patterns within the Stroke Belt may in part offer insight to the increased prevalence of diet-related diseases within this region [38]. This becomes even more problematic as availability, accessibility and exposure to sufficient quantities and quality of more healthful food options (e.g. fresh fruit and vegetables, lean meats, whole grains, low fat dairy products, etc.) is limited in lower income neighborhoods, which have fewer supermarkets in comparison to fast food establishments [39].
Regarded as a “food desert”, this built environment promotes and sustains the consumption of processed foods rich in sodium, sugar, fat and calories, and sets the stage for disparities in dietary intake and diet-related disease prevalence [40]. This disadvantaged food environment not only directly effects food consumption, but indirectly influences disease risk by fostering the inability to maintain a dietary pattern that promotes health and prevents disease [41-43]. More recently, the term “food swamp” has been introduced to describe foodways or food systems dominated by and saturated with calorically-dense foods and beverages [44,45]. In contrast to food deserts, which lack access and availability to nutritious and affordable food, food swamps offer (few) nutritious and affordable foods. However, the accessibility and availability of healthier food options is often “swamped” or overshadowed by the presence of processed, energy-dense, less expressive foods [46].
The relationship between food, culture and diabetes has been exposed- with a two-edged sword revelation. Individuals within certain cultures, by default, may be at a generational disadvantage because their culture may not easily endorse the consumption of healthier, high-quality foods. This may be due in part to the learned food preference, preparation and consumption patterns and the geographical challenge of food deserts and swamps. Currently defined as a high-risk population, the African American culture (particularly in the southeastern region of the United States), has experienced a disproportionately greater risk for diabetes, obesity, hypertension and other diet-related diseases [37]. Although the cultural dietary pattern of the Stroke Belt contains many nutrient- dense foods, rich in vitamins, minerals, dietary fiber, antioxidants and other bioactive compounds, the preparation and preservation methods employed may unintentionally mitigate the potential health benefits. This in and of itself adds an additional challenge to preventing disease and promoting health in the Stroke Belt.
Opportunities within the Dietary Pattern of the Stroke Belt
The colorful nature of many plant-based items included in the dietary pattern of the Stroke Belt visually represents the phytochemical and antioxidant potential of these items and their capacity to reduce the oxidative stress, inflammation and cellular injury associated with disease. Major phenolic and flavonoid compounds found in select indigenous vegetables (i.e. collard greens, mustard greens, kale, okra, sweet potato greens, green onion, butter beans, butter peas, purple hull peas, rutabagas, eggplant, and purslane) consumed in the southeastern United States include quercetin, kaempferol, isorhamnetin and ferulic acid, which have significant antioxidant potential that may be beneficial in reducing oxidative stress and inflammation associated with disease pathogenesis [47,48]. Unfortunately, certain preparation practices may lessen the intrinsic benefits offered by these foods.
Individuals living in the Stroke Belt are more likely to consume fish that has been battered and fried, which may lessen the health benefits by destroying omega-3 fatty acids, which otherwise may exert beneficial effects on blood pressure, lipid profile and endothelial function [49]. Researchers have shown that steam cooking is able to significantly increase the in vitro bile acid binding capacity of vegetables such as collard greens, mustard greens, cabbage and kale, which are all components of the dietary pattern in the Stroke Belt [50,51]. Kidney beans [52], okra, green beans, turnip greens, and eggplant, also included in the Stroke Belt dietary pattern, exhibit bile acid binding capacities as well [53]. The ability of these dietary components to bind bile acids demonstrate their hypolipidemic and hypocholesterolemic effects, which are critical in the prevention of diabetes and other chronic, diet-related diseases.
In addition to the root (i.e. tuber), sweet potatoes leaves, stalks and stems are exceptional sources of minerals, antioxidants, and bioactive compounds with anti-inflammatory, antidiabetic, antimicrobial, and hepatoprotective characteristics [54]. Although not readily consumed in the southeastern United States, sweet potato leaves offer cardioprotective, chemopreventive, and other health promoting benefits [55,56]. Researchers found that steam cooking of sweet potato leaves results in an increase in total polyphenol content and antioxidant activity [57]. In this same study boiling, microwaving and frying sweet potato leaves resulted in decreased total polyphenol content; boiling and microwaving resulted in decreased antioxidant activity. Considering the before mentioned research findings, steam cooking appears to be a viable option to optimize phenolic content and antioxidant activities, while at the same time potentially reducing the amount of added fat in the diet.
Dietary modifications that encourage more optimal food preparation techniques may be extremely useful in reducing the risk for diabetes mellitus and other diet-related disease in the Stroke Belt. The Dietary Approaches to Stop Hypertension (DASH) dietary pattern, created to diminish the risks associated with hypertension, offers preparation modification that encourages the substitution of fats (i.e. animal fats → plant fats), lower fat milk and cheeses (whole milk→ skim milk), using egg whites instead of whole eggs, removing skin from meats prior to cooking, baking or broiling instead of frying, lean meats, salt and sugar substitutes [58]. Although the DASH diet has been verified to reduce blood pressure and provide cardiometabolic benefits, it is not readily embraced by those with hypertension [59]. Cultural beliefs about certain nutrients, food selection and eating behaviors are all potential barriers to commencement and adherence to the DASH dietary pattern [60,61]. In addition, partnering with African American churches has been proposed as an integral component of promoting health in the African American community [62]. Disease prevention and health promotion campaigns and interventions within the Stroke Belt may consider further exploiting these established methods and practices. Potential opportunities within the Stroke Belt dietary pattern to promote health and prevent disease are presented in Table 1.
Conclusion
Like most chronic, diet-related disease, the risk factors for diabetes may be characterized as non-modifiable, modifiable and manageable. The dietary composition may be viewed as the most easily modified and most variable risk factor, and conversely the least easily modified and least variable. Ironically malnutrition in terms of both excess and deficiency may increase the risk for diabetes and chronic disease. Depending upon one’s stage of growth, development and physiological status along the life span nutritional needs may increase or decrease. The challenge of meeting the nutritional needs is dependent upon many economic, social, cultural and individual characteristics- which may or may not be controllable by the individual. Dietary and environmental factors characterized as diabetogenic, obesogenic, atherogenic or toxigenic may facilitate the manifestation of adverse outcomes, co- morbidities and premature mortality. Disparities in the prevalence of diabetes and other chronic diet-related diseases and conditions are widespread among at-risk minorities and other individuals living in communities with lower educational attainment, lower incomes, little or no access to sufficient quantities and quality of nutrient-dense foods, health care and other services necessary to optimize health outcomes. Further, these individuals are at an increased risk for health disparities and accompanying co- morbidities and premature mortality associated with diabetes. One such community is the Stroke Belt.
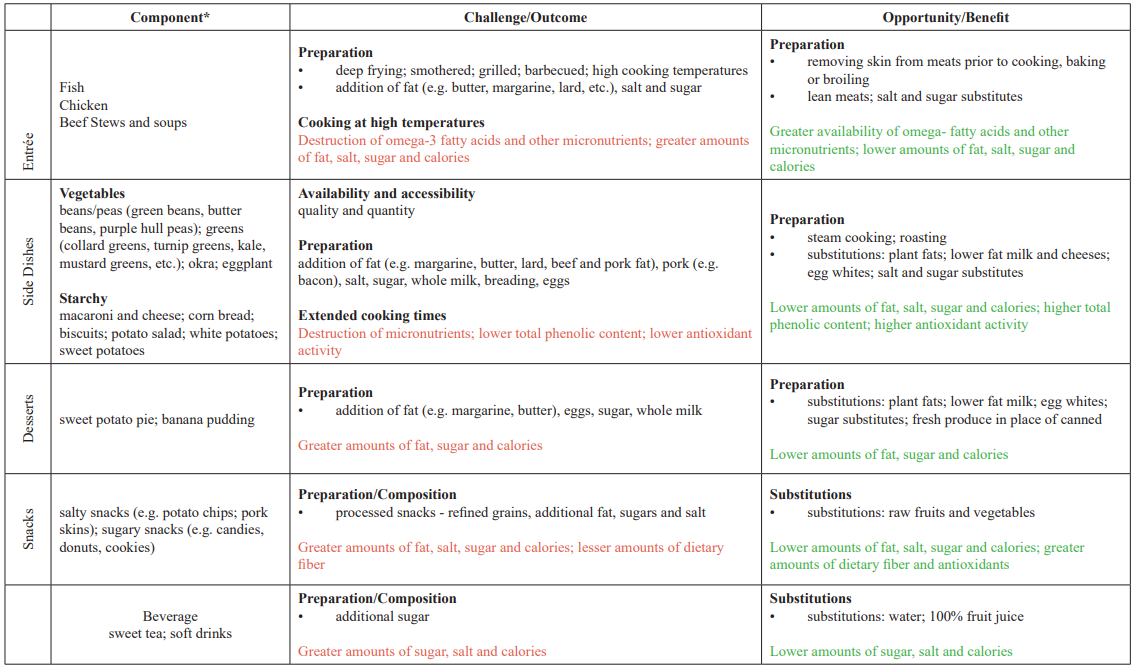
Table 1: Potential opportunities within the Stroke Belt dietary pattern to promote health and prevent disease. * Not exhaustive and does not include all of the components of the Stroke Belt dietary pattern.
The Stroke Belt, an 11-state expanse within the southeastern region of the United States, presents a unique dietary and built environment that greatly enhances the risk for diabetes, stoke, cardiovascular disease and other chronic disease. Entwined in the fabric and culture of the Stroke Belt is food- intentionally selected and prepared to “comfort the soul”. Unfortunately this “comfort” may encase the body in excessive nutrients that may interfere with optimum metabolic functioning. Although there are many dietary challenges within the Stroke Belt that may intensify diabetes risk and pathogenesis, there are available opportunities to attenuate the risks. Components of the Stroke Belt dietary pattern have demonstrated antioxidant, anti-inflammatory, hypoglycemic, hypotensive, hypocholesterolemic and cardioprotective capabilities that are critical to promoting health. Providing guidance on food intake, in addition to optimal preparation techniques, may provide cardiometabolic advantages that were previously not present. Identifying dietary challenges and opportunities within the Stroke Belt is the first of many steps in equipping individuals with scientifically-based tools and resources to significantly promote public health and prevent disease within their community.
References
- Evans JL, Goldfine A new road for treating the vascular complications of diabetes: so let's step on the gas. Diabetes. 2016; 65: 346-348.
- Gregg EW, Sattar N, Ali MK. The changing face of diabetes complications. Lancet Diabetes Endo. 2016; 4: 537-547.
- Preiss D, Sattar N. Diabetic microvascular complications as simple indicators of risk for cardiovascular outcomes and heart failure. Lancet Diabetes Endo. 2016.
- Voeks JH, McClure LA, Go RC, et Regional differences in diabetes as a possible contributor to the geographic disparity in stroke mortality. Stroke. 2008; 39: 1675-1680.
- Borhani Changes and geographic distribution of mortality from cerebrovascular disease. Am J Public Health N. 1965; 55: 673-681.
- Feinleib M, Ingster L, Rosenberg H, et Time trends, cohort effects, and geographic patterns in stroke mortality--United States. Ann Epidemiol. 1993; 3: 458-465.
- Lanska Geographic distribution of stroke mortality in the United States 1939-1941 to 1979-1981. Neurology. 1993; 43: 1839-1839.
- Howard G, Labarthe DR, Hu J, et al. Regional differences in African Americans' high risk for stroke: the remarkable burden of stroke for Southern African Americans. Ann Epidemiol. 2007; 17: 689-696.
- Liao Y, Greenlund KJ, Croft JB, et al. Factors explaining excess stroke prevalence in the US Stroke Stroke. 2009; 40: 3336-3341.
- Glymour MM, Avendano M, Berkman Is the ‘Stroke Belt’Worn From Childhood? Stroke. 2007; 38: 2415-2421.
- Myers CA, Slack T, Broyles ST, et Diabetes prevalence is associated with different community factors in the diabetes belt versus the rest of the United States. Obesity. 2017; 25: 452-459.
- Dinu M, Pagliai G, Casini A, et al. Mediterranean diet and multiple health outcomes: an umbrella review of meta- analyses of observational studies and randomised trials. Eur J Clin Nutr. 2017.
- Esposito K, Maiorino MI, Bellastella G, et al. Mediterranean diet for type 2 diabetes: cardiometabolic Endocrine. 2017; 56: 27-32.
- Estruch R, Ros E, Salas-Salvadó J, et al. Primary prevention of cardiovascular disease with a Mediterranean diet. New Engl J Med. 2013; 368: 1279-1290.
- Liu RH. Health benefits of fruit and vegetables are from additive and synergistic combinations of Am J Clin Nutr. 2003; 78: 517S-520S.
- Liu Whole grain phytochemicals and health. J Cereal Sci. 2007; 46: 207-219.
- McCullough ML, Feskanich D, Stampfer MJ, et al. Diet quality and major chronic disease risk in men and women: moving toward improved dietary guidance. Am J Clin Nutr. 2002; 76: 1261-1271.
- Jannasch F, Kröger J, Schulze Dietary Patterns and Type 2 Diabetes: A Systematic Literature Review and Meta-Analysis of Prospective Studies. J Nutr. 2017; 147: 1174-1182.
- Joint WHO/FAO, Diet, nutrition and the prevention of chronic diseases: report of a joint WHO/FAO Expert Consultation. 2003.
- Kereliuk SM, Brawerman GM, Dolinsky VW. Maternal Macronutrient Consumption and the Developmental Origins of Metabolic Disease in the Offspring. Int J Mol Sci. 2017; 18: 1451.
- St-Onge MP, Ard J, Baskin ML, et al. Meal Timing and Frequency: Implications for Cardiovascular Disease Prevention: A Scientific Statement From the American Heart Association. Circulation. 2017; 135: e96-e121.
- Harville EW, Jacobs MB, Qi L, et al. Multigenerational Cardiometabolic Risk as a Predictor of Birth Outcomes: The Bogalusa Heart Study. J Pediatr. 2017; 181: 154-162.e151.
- Psaltopoulou T, Hatzis G, Papageorgiou N, et al. Socioeconomic status and risk factors for cardiovascular disease: Impact of dietary Hell J Cardiol. 2017; 58: 32-42.
- Savitsky B, Manor O, Friedlander Y, et al. Associations of socioeconomic position in childhood and young adulthood with cardiometabolic risk factors: the Jerusalem Perinatal Family Follow-Up J Epidemiol Commun H. 2017; 71: 43-51.
- Yang Y, Buys DR, Judd SE, et al. Favorite foods of older adults living in the Black Belt Region of the United States. Influences of ethnicity, gender, and education. 2013; 63: 18-23.
- Tucker KL, Maras J, Champagne CM, et al. A regional food- frequency questionnaire for the US Mississippi Delta. Public Health Nutr. 2007; 8: 87-96.
- Champagne CM, Bogle ML, McGee BB, et Dietary intake in the lower Mississippi delta region: results from the Foods of our Delta Study. J Am Diet Assoc. 2014; 104: 199-207.
- Champagne CM, Casey PH, Connell CIL, et al. Poverty and food intake in rural America: diet quality is lower in food insecure adults in the Mississippi Delta. J Am Diet Assoc. 2007; 107: 1886-1894.
- Connell CL, Yadrick MK, Simpson P, et al. Food Supply Adequacy in the Lower Mississippi J Nutr Edu Behav. 2007; 39: 77-83.
- Judd SE, Gutiérrez OM, Newby PK, et al. Dietary Patterns Are Associated With Incident Stroke and Contribute to Excess Risk of Stroke in Black Americans. Stroke. 2013; 44: 3305-
- Liu J, Hickson DA, Musani SK, et al. Dietary patterns, abdominal visceral adipose tissue, and cardiometabolic risk factors in African Americans: the Jackson heart Obesity. 2013; 21: 644-651.
- Shikany JM, Safford MM, Newby PK, et Southern Dietary Pattern Is Associated With Hazard of Acute Coronary Heart Disease in the Reasons for Geographic and Racial Differences in Stroke (REGARDS) Study. Circulation. 2015; 132: 804- 814.
- Chan Q, Stamler J, Elliott Dietary factors and higher blood pressure in African-Americans. Curr Hypertens Rep. 2015; 17: 10.
- Newby PK, Noel SE, Grant R, et al. Race and Region Are Associated with Nutrient Intakes among Black and White Men in the United States. J Nutr. 2011; 141: 296-303.
- Chatterjee R, Brancati FL, Shafi T. Non-Traditional Risk Factors are Important Contributors to the Racial Disparity in Diabetes Risk: The Atherosclerosis Risk in Communities Study. J Gen Intern Med. 2014; 29: 290-297.
- Chatterjee R, Maruthur NM, Edelman Novel Risk Factors for Type 2 Diabetes in African-Americans. Curr Diabetes Rep. 2015; 15: 103.
- Kulkarni Food, Culture, and Diabetes in the United States. Clin Diabetes. 2004; 22: 190-192.
- Lanska DJ, Kuller The geography of stroke mortality in the United States and the concept of a stroke belt. Stroke. 1995; 26: 1145-1149.
- Lamichhane AP, Warren J, Puett R, et al. Spatial patterning of supermarkets and fast food outlets with respect to neighborhood Health & place. 2013; 23: 157- 164.
- Beaulac J, Kristjansson E, Cummins S. Peer reviewed: A systematic review of food deserts, 1966-2007. Prev Chronic Dis. 2009; 6.
- Bethea TN, Palmer JR, Rosenberg L, et al. Neighborhood Socioeconomic Status in Relation to All-Cause, Cancer, and Cardiovascular Mortality in the Black Women's Health Ethnic Dis. 2016; 26: 157-164.
- Reitzel LR, Okamoto H, Hernandez DC, et The built food environment and dietary intake among African-American adults. Am J Health Behav. 2016; 40: 3-11.
- Walker RE, Keane CR, Burke JG. Disparities and access to healthy food in the United States: A review of food deserts literature. Health & place. 2010; 16: 876-884.
- Bridle-Fitzpatrick Food deserts or food swamps?: A mixed- methods study of local food environments in a Mexican city. Soc Sci Med. 2015; 142: 202-213.
- Fielding JE, Simon PA. Food deserts or food swamps?: Comment on “Fast food restaurants and food stores”. Arch Intern Med. 2011; 171: 1171-1172.
- Luan H, Law J, Quick Identifying food deserts and swamps based on relative healthy food access: a spatio-temporal Bayesian approach. Int J Health Geogr. 2015; 14: 37.
- Huang Z, Wang B, Eaves DH, et al. Phenolic compound profile of selected vegetables frequently consumed by African Americans in the southeast United States. Food Chem. 2007; 103: 1395-1402.
- Huang Z, Wang B, Eaves DH, et al. Total phenolics and antioxidant capacity of indigenous vegetables in the southeast United States: Alabama Collaboration for Cardiovascular Equality Project. Int J Food Sci Nutr. 2009; 60: 100-108.
- Nahab F, Le A, Judd S, et Racial and geographic differences in fish consumption: The REGARDS Study. Neurology. 2011; 76: 154-158.
- Kahlon TS, Chapman MH, Smith In vitro binding of bile acids by spinach, kale, brussels sprouts, broccoli, mustard greens, green bell pepper, cabbage and collards. Food Chem. 2007b; 100: 1531-1536.
- Kahlon TS, Chiu M-C.M, Chapman MH. Steam cooking significantly improves in vitro bile acid binding of collard greens, kale, mustard greens, broccoli, green bell pepper, and cabbage. Nutr Res. 2008; 28: 351-357.
- Kahlon TS, Smith GE, Shao In vitro binding of bile acids by kidney bean (Phaseolus vulgaris), black gram (Vigna mungo), bengal gram (Cicer arietinum) and moth bean (Phaseolus aconitifolins). Food Chem. 2005; 90: 241-246.
- Kahlon TS, Chapman MH, Smith In vitro binding of bile acids by okra, beets, asparagus, eggplant, turnips, green beans, carrots, and cauliflower. Food Chem. 2007a; 103: 676-680.
- Wang S, Nie S, Zhu Chemical constituents and health effects of sweet potato. Food Res Int. 2016; 89: 90-116.
- Johnson M, Pace RD. Sweet potato leaves: properties and synergistic interactions that promote health and prevent disease. Nutr Rev. 2010; 68: 604-615.
- Johnson M, Pace RD, Dawkins NL, et al. Diets containing traditional and novel green leafy vegetables improve liver fatty acid profiles of spontaneously hypertensive rats. Lipids Health Dis. 2013; 12: 168.
- Sun H, Mu T, Xi L, et Effects of domestic cooking methods on polyphenols and antioxidant activity of sweet potato leaves. J Agr Food Chem. 2014; 62: 8982-8989.
- Rankins J, Wortham J, Brown LL. Modifying Soul Food for the Dietary Approaches to Stop Hypertension Diet(dash) Plan: Implications for Metabolic Syndrome(dash of Soul). Ethnic Dis. 2007; 17: 7-12.
- Mitka M. DASH dietary plan could benefit many, but few hypertensive patients follow it. JAMA. 2007; 298: 164-165.
- Bisogni CA, Jastran M, Seligson M, et al. How people interpret healthy eating: contributions of qualitative J Nutr Edu Behav. 2012; 44: 282-301.
- Smith SL, Quandt SA, Arcury TA, et al. Aging and eating in the rural, southern United States: beliefs about salt and its effect on health. Soc Sci Med. 2006; 62: 189-198.
- Butler-Ajibade P, Booth W, Burwell C. Partnering with the black church: recipe for promoting heart health in the stroke belt. ABNF J. 2012; 23: 34.