The Healing Effect of Minimally - Invasive Surgical Fissurectomy in Patients with Chronic Anal Verge Fissure Failed to Cure by Optimal Medical Therapy
Author'(s): Dr. Zana Nasraddin Mohialdeen MBChB, HDGS, MRCS*
MBChB-Diploma in Medicine, Kurdistan Board Emergency Medicine, Sulaimaniyah Directory of Health, Iraqi Kurdistan Ministry of Health, Iraq.
*Correspondence:
Dr. Zana Nasraddin Mohialdeen, MBChB, HDGS, MRCS-Ireland; Sulaimaniyah Polytechnic University, Department of Anaesthesia.
Received: 02 January 2020 Accepted: 30 January 2020
Citation: Zana Nasraddin Mohialdeen. The Healing Effect of Minimally - Invasive Surgical Fissurectomy in Patients with Chronic Anal Verge Fissure Failed to Cure by Optimal Medical Therapy. Gastroint Hepatol Dig Dis. 2020; 3(1): 1-4.
Abstract
Background: The search for an alternative to lateral internal sphincterotomy,the standard surgery for chronic anal fissure which may be complicated by anal fecal incontinence, is continuing. Fissurectomy is one of the alternatives, but this also done under general or spinal anesthesia. Few studies had explored the possibility of doing fissurectomy under local anesthesia anal infiltration and this study tries to explore this approach.
Aims: To evaluate the role of minimally - invasive surgical fissurectomy in patients with chronic anal verge fissure failed to cure by optimal medical therapy.
Patients and Methods: We evaluated a minimally - invasive surgical fissurectomy for inducing healing of these fissures. The procedure was done under local anesthesia (xylocaine + adrenaline 20 ccs) infiltration around the anus and conscious sedation of pethidine 100 mgm and Medazolam 5 mgm both given intravenous 5 minutes before the local xylocaine infiltration. We evaluated the patients for absence of pain during defecation and the complete
healing of the wound area, 3 weeks and 3 months after the operation., to know the short-term and long-term cure rates.
Results: Among 35 patients with chronic anal fissures failed to heal by medical therapies, fissurectomy under local anesthesia infiltration around the anus facilitated by giving a proper dose of intravenous conscious sedation, had resulted in an excellent outcome with a healing rate of 95% & fewer and less severe anal incontinence rate of 8%.
Conclusion: Anal fissure occurs in young persons more in females and commonly in posterior location of anal verge. Minimally invasive fissurectomy under local anesthesia with the help of conscious sedation can be a good alternative to classical lateral internal sphincterotomy which has higher anal incontinent rates, sometimes perminant.
Keywords
Introduction
Anal fissure is an ulceration of the anal canal anoderm [1]. It is one of the most frequent painful anal conditions [2]. Many factors contribute to its causation including mechanical trauma, sphincter spasm, and ischemia and the management should address these factors. Sphincter hypertonia causing local ischemia is considered as the main causal mechanism [3]. The American and British scientific societies have published treatment guidelines [4]. Medical treatment is non-specific, aimed at softening the stool, facilitating regular bowel movements; resulting in healing of almost 50% of acute anal fissures [5].
The risk of recurrent fissure remains high if the causative factors persist. If the former medical treatment fails, medical treatment to reversibly decrease hypertonic sphincter spasm such as local diltiazem and or botulinum toxin local injection are used [6].
When symptoms persist after 4 to 8 weeks of appropriate medical treatment, surgery should be considered. Surgery remains the most effective long-term treatment and should be offered for cases of chronic or complicated anal fissure and for acute anal fissure with severe pain or for recurrent fissure despite optimal medical treatment [7].
Surgical treatment is based on two principles that may be combined: decreasing sphincter tone and excision of the anal fissure [8]. The old forcible uncalibrated anal dilatation is no longer recommended because of high rate of incontinence [9]. Lateral internal sphincterotomy (LIS) is the best-evaluated technique and remains the gold standard, but since LIS is associated with some risk of irreversible anal incontinence, the search for more continent- saving methods continues, where fissurectomy combined with anoplasty is preferred [10]. Other techniques have been described to reduce the risk of incontinence (calibrated sphincterotomy, sphincteroplasty). The lateral internal sphincterotomy reduces the hypertonia by decreasing the pressure in the anal canal, thereby improving local vascularization and allowing the fissure to resolve, by average healing ate of 90% with recurrence rate below 10%, but associated with anal incontinence rates up to 30% in some studies [11].
Alternative techniques proposed, being associated with a lower level of evidence, are the ’tailored’ lateral sphincterotomy, pneumatic balloon dilation [12]. Foremost surgical techniques that do not divide the internal anal sphincter, namely, a subcutaneous fissurotomy and fissurectomy plus anoplasty, the so-called V-Y cutaneous flap or mucosal flap, initially those techniques were done to patients with high risk of postoperative incontinence, such as elderly people, multiparous women, patients with normal anal tone, patients with chronic diarrhea of any origin, and patients who had undergone previous anorectal surgery [13].
Because the results exhibited similar rates of healing as compared to those obtained with a lateral internal sphincterotomy, both in anecdotal and published evidence, many proctologists, adopted those sphincter-sparing techniques as a standard care for any chronic anal fissure refractory to medical management [14]. Given the trade-offs between the risks and benefits, FIAP and BT might be good alternatives for the treatment of chronic anal fissures. Fissurectomy combined with high-dose botulinum toxin A is a safe, effective, and durable option for the management of chronic anal fissure and a promising alternative to surgical sphincterotomy [15].
Aims of the Study
To evaluate the role of minimally - invasive surgical fissurectomy in patients with chronic anal verge fissure failed to cure by optimal medical therapy.
Patients and Methods
In a total of 35 patients with chronic anal verge fissure failed to cure by optimal medical therapy, we evaluated a minimally - invasive surgical fissurectomy for inducing healing of these fissures. The procedure was done under local anesthesia (xylocaine + adrenaline 20 ccs) infiltration around the anus and conscious sedation of pethidine 100 mgm and Medazolam 5 mgm both given intravenous 5 minutes before the local xylocaine infiltration. The avoidance of general and spinal anesthesia resulted in reduced costs, an important issue to our patients seeking treatment in private surgical clinics after they had been put on long waiting lists in governmental semi-free hospitals. We evaluated the patients for absence of pain during defecation and the complete healing of the wound area, 3 weeks and 3 months after the operation., to know the short-term and long-term cure rates.
Results
Discussion
The aim of this study was to evaluate the role of minimally - invasive surgical fissurectomy in patients with chronic anal verge fissure failed to cure by optimal medical therapy by avoiding the use of both general and local anesthesia by using combining local anesthesia infiltration and intravenous conscious sedation using a combination of medazolam and pethidine. Other studies had evaluated this approach for managing anal fissure with good results [16,17].
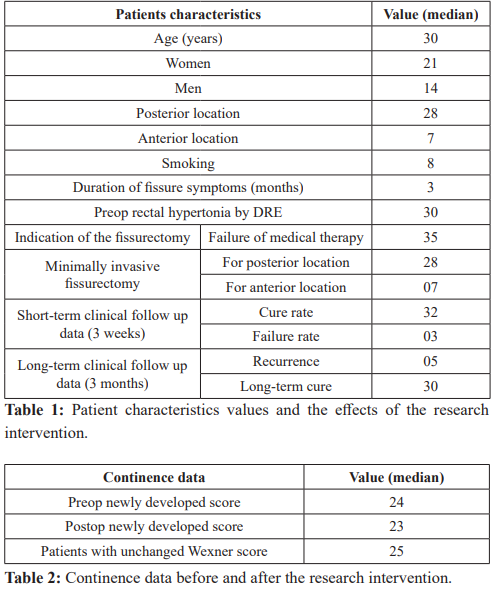
In this study 35 patients with chronic anal fissure, who failed medical therapy consisting of laxatives and local diltiazem therapy for 3 months, had undergone fissurectomy using the minimally invasive procedure mentioned above. Most patient were young and female (21 vs 14). Studies had found that fissure occur more in young females, probably related to birth trauma and constipation, both common during pregnancy and delivery [18].
Most fissure occurred in the posterior part of the anus more than the anterior part (28 vs 7). Studies had indicated that two third of fissures occur in the posterior location and those in anterior location occur more in young females [19,20].
Few patients with anal fissure in this series were chronic smokers not more than the prevalence of smoking in the general population and smoking as indicated also by other studies does not contribute to this condition [1].
We evaluated the patients for absence of pain during defecation and the complete healing of the wound area, 3 weeks and 3 months after the operation to see the short-term and long term-cure rates. We found that 32 out of 25 had complete short-term cure, while 30 out of 35 had long-term cure after 3 months, meaning that we had 5 case failure and these cases were sent for other options. Few studies had done procures similar to this study. A study done in Saudi Arabia indicated that topical anesthetics and local anesthesia can be used effectively for lateral sphincterotomy and provides an alternative to general anesthesia [21].
The long-term outcomes, in terms of complete cure, for lateral internal sphincterotomy are very good (96%) but on the expense of higher fecal incontinent rate which in some cases may be permanent [22]. The success rate in this series was 95%, a little bit lower than the classical surgery.
The anal continent results of this study were very good as only 3 patients shown in Table number 2 had incontinence only for flatus and the current study used the newly developed score published in the GUT [21] among many other. Fecal incontinence occurs in 10% after lateral internal sphincterotomy [23], while it occurred in only 8% of this series and the incontinence occurred only for flatus.
Conclusion
Anal fissure occurs in young persons more in females and commonly in posterior location of anal verge. Minimally invasive fissurectomy under local anesthesia with the help of conscious sedation can be a good alternative to classical lateral internal sphincterotomy which has higher anal incontinent rates.
References
- Higuero T. Update on the management of anal fissure. J Visc 2015; 152: S37-43.
- Ulyanov AA, Solomka AY, Achkasov EE, et Chronic anal fissure. Etiopathogenesis, diagnosis, treatment. Khirurgiia (Mosk). 2018; 11: 89-95.
- Mousavi SR, Sharifi M, Mehdikhah Z. A comparison between the results of fissurectomy and lateral internal sphincterotomy in the surgical management of chronic anal fissure. J astrointest 2009; 13: 1279-1282.
- Tsunoda A, Takahashi T, Kusanagi Fissurectomy with vertical non-full-thickness sphincterotomy for chronic anal fissure. Tech Coloproctol. 2019; 23: 1-5.
- Andicoechea Agorría A, Del Casar Lizcano JM, Barbon Remis E, et al. Treatment of a chronic anal fissure with a botulin toxin A injection and fissurectomy. Esp Enferm Dig. 2019; 111: 672-676.
- Ebinger SM, Hardt J, Warschkow, et Operative and medical treatment of chronic anal fissures-a review and network meta- analysis of randomized controlled trials. RJ Gastroenterol. 2017; 52: 663-676.
- Barnes TG, Zafrani Z, Abdelrazeq Fissurectomy Combined with High-Dose Botulinum Toxin Is a Safe and Effective Treatment for Chronic Anal Fissure and a Promising Alternative to Surgical Sphincterotomy. Dis Colon Rectum. 2015; 58: 967-973.
- Cross KL, Massey EJ, Fowler AL, et ACPGBI. The management of anal fissure. ACPGBI position statement. Colorectal Dis. 2008; 10: 1-7.
- Perry WB, Dykes SL, Buie WD, et Standards Practice Task Force of the American Society of Colon and Rectal Surgeons. Practice parameters for the management of anal fissures(3rd revision). Dis Colon Rectum. 2010; 53: 1110-1115.
- Altomare DF, Binda GA, Canuti S, et al. The management of patients with primary chronic anal fissure: a position paper. Tech 2011; 15: 135-141.
- Garg P, Garg M, Menon Long-term continence disturbance after lateral internal sphincterotomy for chronic anal fissure. A systematic review and meta-analysis. Colorectal Dis. 2013; 15: e104-117.
- García-Granero E, Sanahuja A, García-Botello SA, et The ideal lateral interna sphincterotomy: clinical and endosonographic evaluation following open and closed internal anal sphincterotomy. Colorectal Dis. 2009; 11: 502- 507.
- Renzi A, Izzo D, Di Sarno G, et Clinical, manometric, and ultrasonographic results of pneumatic balloon dilatation vs. lateral internal sphincterotomy for chronic anal fissure. A prospective, randomized, controlled trial. Dis Colon Rectum. 2008; 51: 121-127.
- Pelta AE, Davis KG, Armstrong Subcutaneous fissurotomy. A novel procedure for chronic fissure-in-ano. A review of 109 cases. Dis Colon Rectum. 2007; 50: 1662-1667.
- Schornagel IL, Witvliet M, Engel AF. Five-year results of fissurectomy for chronic anal fissure. low recurrence rate and minimal effect on continence. Colorectal Dis. 2012; 14: 997-
- Darcy Shaw, Charles A. Ternent. Perioperative Management of the Ambulatory Anorectal Surgery Clin Colon Rectal Surg. 2016; 29: 7-13.
- Douglas W Mapel, Michael Schum, Ann Von Worley. The epidemiology and treatment of anal fissures in a population- based BMC Gastroenterol. 2014; 14: 129.
- Jennifer Sam Beaty Shashidharan. Anal Fissure. Clin Colon Rectal Surg. 2016; 29: 30-37.
- Jean-David Zeitoun, Pierre Blanchard, Nadia Fathallah, et al. Long-term Outcome of a A Prospective Single- Arm Study of 50 Operations out of 349 Initial Patients. Ann Coloproctol. 2018; 34: 83-87.
- A E Al-Raymoony. Surgical treatment of anal fissures under local Saudi medical journal. 2001; 22:114-116.
- Vaizey CJ, Carapeti E, Cahill JA, et Prospective comparison of faecal incontinence grading systems. Gut. 1999; 44: 77-80.
- Nyam DC, Pemberton Long-term results of lateral internal sphincterotomy for chronic anal fissure with particular reference to incidence of fecal incontinence. Dis Colon Rectum. 1999; 42: 1306-1310.
- Rotholtz NA, Bun M, Mauri MV, et Long-term assessment of fecal incontinence after lateral internal sphincterotomy. Tech Coloproctol. 2005; 9: 115-118.