Thoracic Endovascular Aortic Repair in a Patient with Dilated Cardiomyopathy and Low Ejection Fraction: A Case Report
Author'(s): Akiko Ando1, Takeshi Umegaki1*, So Yamaki2, Kota Nishimoto1, Tomohiro Shoji1, Munenori Kusunoki1,Saya Hakata1 and Takahiko Kamibayashi1
1 Department of Anesthesiology, Kansai Medical University Hospital, Osaka, Japan.
2 Department of Surgery, Kansai Medical University Hospital,Osaka, Japan.
*Correspondence:
Takeshi Umegaki, Department of Anesthesiology, Kansai Medical University Hospital, Osaka 573-1191, Japan, Tel: +81-72-804-0101;Fax: +81-72-804-2785; E-mail: umegakit@hirakata.kmu.ac.jp
Received: 07 February 2018; Accepted: 24 March 2018
Citation: Akiko Ando, Takeshi Umegaki, So Yamaki, et al. Thoracic Endovascular Aortic Repair in a Patient with Dilated Cardiomyopathy and Low Ejection Fraction: A Case Report. Anesth Pain Res. 2018; 2(1): 1-4.
Abstract
Background: Thoracic endovascular aortic repair (TEVAR) is a common treatment for high-risk patients with thoracic aortic aneurysms. However, these aneurysms are relatively rare in patients with dilated cardiomyopathy. We successfully treated a thoracic aortic aneurysm in an older patient who presented with dilated cardiomyopathy and low ejection fraction using TEVAR under general anesthesia.
Case Presentation: An 84-year-old man was admitted to our institution with a thoracic aortic aneurysm, as well as dilated cardiomyopathy and an extremely low ejection fraction (15.4%). We scheduled the patient for TEVAR. Before administering general anesthesia, an external defibrillator was prepared for possible arrhythmia. General anesthesia was induced with 3 mg of intravenous midazolam and 100 μg of fentanyl. After endotracheal intubation, anesthesia was maintained with sevoflurane (1.2-1.5%). Intra-operative transesophageal echocardiography revealed that an end-diastolic internal diameter was about 65-70 mm and ejection fraction was 15-20%. Successful hemodynamic management during surgery was achieved with dopamine (1.6–2.4 μg/kg/min), noradrenaline (0.02– 0.06 μg/kg/min), and milrinone (0.06 μg/kg/min). TEVAR was successfully performed without complication, and the patient’s postoperative clinical course was uneventful. He was discharged 14 days after surgery.
Conclusions: We describe the uncommon use of TEVAR in an older patient with dilated cardiomyopathy and an extremely low ejection fraction. This case demonstrates that this minimally invasive surgery may be a suitable technique (under vigilant monitoring) to repair thoracic aortic aneurysms in older patients with low cardiac function.
Keywords
Introduction
Thoracic endovascular aortic repair (TEVAR) is a minimally invasive procedure widely performed in patients with a thoracic or thoraco-abdominal aortic aneurysm [1]. This procedure is especially beneficial in high-risk patients who are unable to undergo open repair [1]. Aortic aneurysms are relatively rare in patients with dilated cardiomyopathy, which is a major cause of cardiac dysfunction due to dilatation and impaired contraction of the left or both ventricles [2,3].
Here, we report our experience in treating a thoracic aortic aneurysm in an older patient who also presented with dilated cardiomyopathy and an extremely low ejection fraction (EF) The patient was successfully treated using TEVAR under general anesthesia without any complications.
Case Report
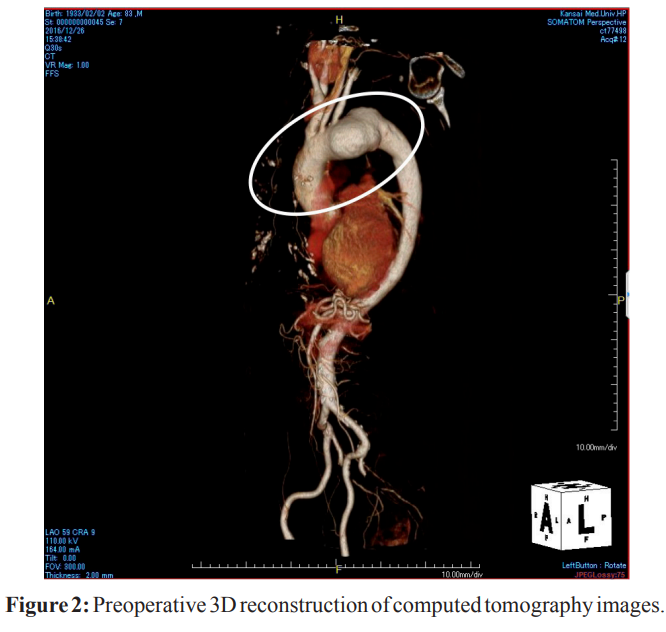
The patient was an 84-year-old man (height: 158 cm, weight: 40 kg) who was diagnosed with a thoracic aortic aneurysm (57 mm) and a Stanford type B thoracic aortic dissection (Figures 1 and 2).
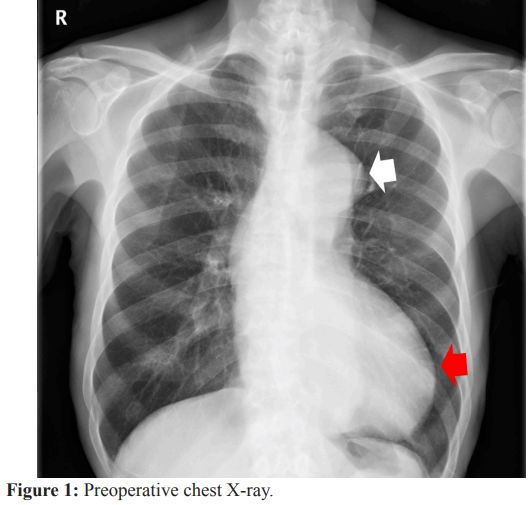
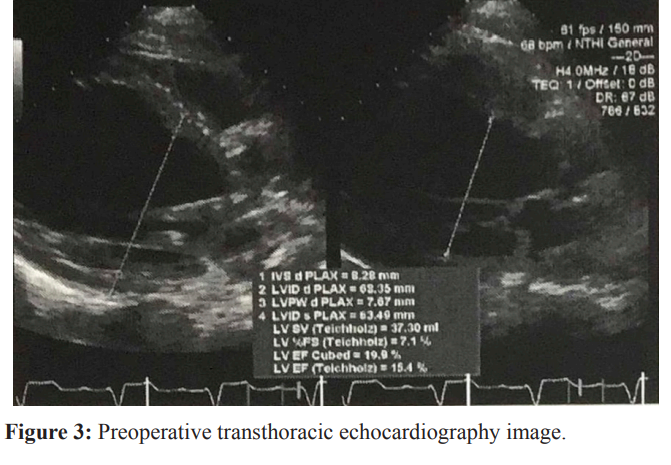
An electrocardiogram revealed complete left bundle branch block. The patient had a dilated left ventricle with an end-diastolic internal diameter of 68 mm, an end-systolic internal diameter of 63 mm, and an extremely low EF of 15.4% (Teichholz method) (Figure 3). The diameters of the left atrium and right ventricle were in the normal range (38 mm and 22 mm, respectively). We observed severe diffuse hypokinesis or akinesis of the left ventricular wall. In addition, there was moderate aortic valve regurgitation (pressure half-time: 364 ms). The patient’s functional capacity was determined to be Class II according to the New York Heart Association classification system. At the time of admission, the patient also presented with chronic renal failure (creatinine level:
After diagnosis, the patient was scheduled to undergo TEVAR. Before general anesthesia was administered, we set up an external defibrillator to account for the possibility of arrhythmia. In the operating theater, general anesthesia was induced with intravenous midazolam (3 mg) and fentanyl (100 μg). After insertion of the endotracheal tube, general anesthesia was maintained with sevoflurane (1.2-1.5%).
Then a transesophageal echocardiography probe was located. Intra-operative transesophageal echocardiography revealed that an end-diastolic internal diameter was about 65-70 mm and ejection fraction was 15-20%. No pulmonary artery catheter was used to avoid complete heart block. TEVAR with double chimney grafts (brachiocephalic artery and left common carotid artery) was performed without any complications (Figure 4).
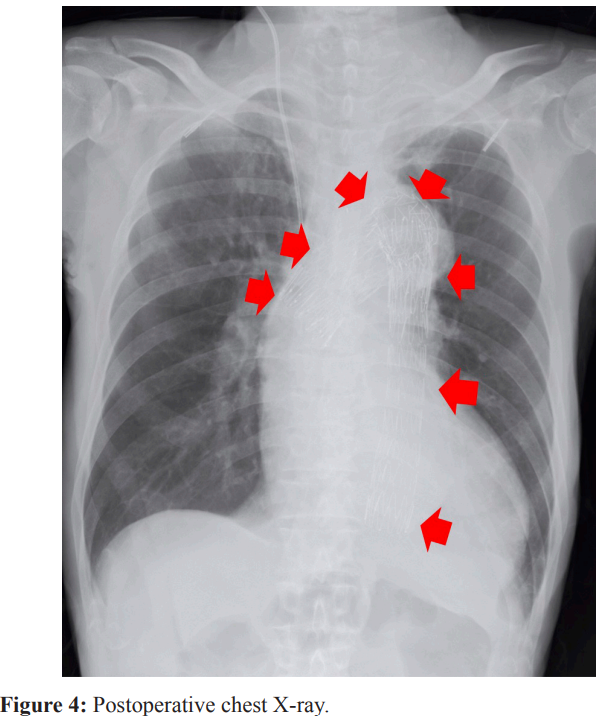
Two TX2 stent grafts (Cook Co. Ltd, Tokyo, Japan) were placed from the mid-portion of the ascending aorta to part of the descending aorta. Successful hemodynamic management (systolic blood pressure: 80-130 mmHg, heart rate: 60-90 bpm) was achieved during surgery with dopamine (1.6-2.4 μg/kg/min), noradrenaline (0.02-0.06 μg/kg/min), and milrinone (0.06 μg/kg/ min). Intraoperative blood loss was 404 ml. The total operating time was 226 min and the anesthesia time was 351 min. After general anesthesia, the patient fully recovered consciousness and was uneventfully extubated. There were no signs of cerebral ischemia.
The patient was transported to our general intensive care unit (ICU), where his postoperative clinical course was uneventful. He was then transferred to the general ward the next day, and discharged from the hospital 14 days after surgery.
Discussion
The anesthetic management of patients with dilated cardiomyopathy is challenging for anesthesiologists due to poor left systolic function and sudden arrhythmic events [2]. Here, TEVAR was successfully performed under general anesthesia to treat a thoracic aortic aneurysm in an older patient with dilated cardiomyopathy and extremely low EF.
The use of TEVAR to treat thoracic aortic aneurysms with dilated cardiomyopathy is relatively rare [4,5]. Oderich et al. reported the successful endovascular repair of an ascending aortic aneurysm in a 48-year-old man with a heart transplant due to end-stage familial dilated cardiomyopathy [4]. Pirelli et al. described the use of a direct transaortic approach to treat a 61-year-old patient with an aortic pseudoaneurysm [5]. Our patient had a considerably lower EF and was older than these previously reported cases. Patients with dilated cardiomyopathy and low EF may be successfully treated using TEVAR with careful management, such as the preparation of an external defibrillator, use of catecholamine during surgery, and postoperative ICU care.
A recent study reported a low incidence (2.4%) of perioperative adverse cardiac events (e.g., myocardial infarction or cardiac arrest) occurring after TEVAR [6]. That study also found that patients who suffered a cardiac event had an average of 4.2 cardiac risk factors (e.g., hypertension, hyperlipidemia, smoking, diabetes, coronary artery disease, history of myocardial infarction, and peripheral vascular disease) [6]. From among these risk factors, our patient only had hypertension. Nevertheless, we consider that he was at high risk of cardiac adverse events during the perioperative and postoperative periods due to dilated cardiomyopathy and low EF.
Van Dorp et al. reported that local anesthesia for TEVAR could be performed safely and effectively [7]. We, however, performed general anesthesia because of routine anesthetic method for TEVAR of even high-risk patients in our center and quick emergency conversion to open surgical repair. But we might have to consider local anesthesia for high-risk patients like this case for immediate recognition of neurologic complications.
A recent systematic review and meta-analysis showed that when compared with open repair for thoracic aortic aneurysm, TEVAR was associated with a reduced risk of mortality, paraplegia, spinal cord ischemia, and pulmonary complications within 30 days of intervention [8,9]. Endovascular repair of thoracic aortic aneurysms is technically feasible in high-risk patients with contraindications for conventional surgery [1]. Careful preoperative planning, high endovascular surgical skills, and appropriate imaging equipment are essential for successful treatment of these patients [10]. We also consider appropriate cardiovascular, respiratory, and neurological management to be necessary. However, the long-term outcomes of TEVAR are still unknown, and may be similar to conventional surgeries [8,11,12]. Therefore, the clinical benefits to the patients must be carefully considered when deciding treatment strategies.
Conclusions
A thoracic aortic aneurysm in an older patient with an extremely low EF was successfully treated using TEVAR under general anesthesia. TEVAR may be a suitable technique for repairing these aneurysms in older patients with low cardiac function.
List of Abbreviations
EF: Ejection Fraction; ICU: Intensive Care Unit; TEVAR: Thoracic Endovascular Aortic Repair.
Consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor- in-Chief of this journal.
Ethics Approval
This is an anonymous case report. Although written informed consent was obtained from the patient for publication of this case report, the ethics committee in our hospital waived the need for ethics committee approval.
Acknowledgments
The authors would like to extend their gratitude to the patient and his family members.
References
1.Semba CP, Mitchell RS, Miller DC, et al. Thoracic aortic aneurysm repair with endovascular stent-grafts. Vasc Med. 1997; 2: 98-103.
2.Chen CQ, Wang X, Zhang J, et al. Anesthetic management of patients with dilated cardiomyopathy for noncardiac surgery. Eur Rev Med Pharmacol Sci. 2017; 21: 627-634.
3.Mukerjee D, Jesuraj ML, Halder SK, et al. Annulo-aortic ectasia with thoraco-abdominal aortic aneurysm in a case of dilated cardiomyopathy. Cardiovasc J Afr. 2008; 19: 268-270.
4.Oderich GS, Pochettino A, Mendes BC, et al. Endovascular repair of saccular ascending aortic aneurysm after orthotopic heart transplantation using an investigational Zenith Ascend Stent-Graft. J Endovasc Ther. 2015; 22: 650-654.
5.Pirelli L, Kliger C, Fontana GP, et al. Direct percutaneous transaortic approach for treatment of aortic pseudoaneurysms. Interact Cardiovasc Thorac Surg. 2015; 20: 680-681.
6.Ganapathi AM, Englum BR, Schechter MA, et al. Role of cardiac evaluation before thoracic endovascular aortic repair. J Vasc Surg. 2014; 60: 1196-1203.
7.van Dorp M, Gilbers M, Lauwers P, et al. Local Anesthesia for percutaneous thoracic endovascular aortic repair. Aorta (Stamford). 2016; 4: 78-82.
8.Alsawas M, Zaiem F, Larrea-Mantilla L, et al. Effectiveness of surgical interventions for thoracic aortic aneurysms: A systematic review and meta-analysis. J Vasc Surg. 2017; 66: 1258-1268.
9.Arnaoutakis DJ, Arnaoutakis GJ, Abularrage CJ, et al. Cohort comparison of thoracic endovascular aortic repair with open thoracic aortic repair using modern end-organ preservation strategies. Ann Vasc Surg. 2015; 29: 882-890.
10.Lioupis C, Abraham CZ. Results and challenges for the endovascular repair of aortic arch aneurysms. Perspect Vasc Surg Endovasc Ther. 2011; 23: 202-213.
11.Terzi F, Rocchi G, Fattori R. Current challenges in endovascular therapy for thoracic aneurysms. Expert Rev Cardiovasc Ther. 2016; 14: 599-607.
12.Abraha I, Romagnoli C, Montedori A, et al. Thoracic stent graft versus surgery for thoracic aneurysm. Cochrane Database Syst Rev. 2016; 6: CD006796.