Using tPA Alone for Fibrinolysis has been A Longstanding Mistake
Author'(s): Victor Gurewich, MD*
Vascular Research Laboratory, Mount Auburn Hospital, Cambridge, MA, USA, Professor of Medicine, Harvard Medical School.
*Correspondence:
Victor Gurewich, MD, Vascular Research Laboratory, Mount Auburn Hospital, Cambridge, MA, USA, Professor of Medicine, Harvard Medical School.
Received: 03 March 2021; Accepted: 26 April 2021
Citation: Gurewich V. Using tPA Alone for Fibrinolysis has been A Longstanding Mistake. Cardiol Vasc Res. 2021; 5(2): 1-3.
Abstract
Fibrinolysis has used tissue plasminogen activator (tPA) alone ever since it replaced Streptokinase (SK) in therapeutic fibrinolysis. This was based on the belief that tPA was responsible for natural fibrinolysis. When prourokinase plasminogen activator was discovered (prouPA) in 1980, it was believed to be an extravascular plasminogen activator. This has turned out to be a mistaken concept. Out of the three fibrin-bound plasminogens responsible for fibrinolysis, only the first one, the one which initiates fibrinolysis, is activated by tPA. The other two are activated by prouPA and two chain uPA (urokinase) respectively. Therefore, the functions of tPA and prouPA are analogous to those of the starter and the fuel in a car. By mimicking this natural model for therapy, fibrinolysis can be made much safer because high dose infusions of tPA, that can cause bleeding at vascular repair sites, are eliminated.
Keywords
Therapeutic fibrinolysis with tPA
Therapeutic fibrinolysis has used tissue plasminogen activator (tPA) alone since 1987, when tPA was first approved for the treatment of acute myocardial infarction (AMI). This choice was based on the belief that tPA was alone responsible for fibrinolysis. However, this assumption should have been put into question from the outset after it was determined that tPA’s efficacy was only comparable to that of streptokinase (SK), an indirect activator with no fibrin clot affinity.
A total of 95,740 AMI patients were tested and in the first two mega trials there was no mortality difference between tPA and SK but there was only more intracranial hemorrhage with tPA. Finally, in the third trial, a significantly lower mortality was seen in one out of four groups. However, when these findings were re-examined by Bayesian analysis, it was concluded that a significant difference between tPA and SK had not been established [1]. Despite these findings, tPA received FDA approval for the treatment of AMI and remains the only plasminogen activator available for therapeutic use.
These first trials were a forerunner to the subsequent clinical experience with tPA, which has never lived up to early expectations. Over the past decade or so, tPA has been replaced by percutaneous coronary intervention (PCI) as the treatment of choice for AMI despite being a technically demanding and more time-consuming procedure. That PCI should nevertheless give significantly provide better clinical results is a reflection on tPA’s inefficacy. This is may be due to it being limited to a single binding site on the D-domain of fibrin, which is close to a plasminogen-binding site (see Figure). As result, a ternary complex is formed between tPA, plasminogen, and fibrin and this complex promotes plasminogen activation by tPA about 1,000-fold and initiates fibrinolysis. Due to this ternary complex, this reaction requires no more than a 5 mg bolus dose of tPA. This highly efficient reaction is, however, limited to the activation of one out of three plasminogen’s on fibrin monomer.
Since tPA is a very weak plasminogen activator when not in this ternary complex, this step completes tPA’s function in fibrinolysis. It requires quite unphysiological doses of tPA to activate the other two fibrin-bound plasminogen’s, which are located on the fibrin E-domain (see Figure). As a result of it being a weak activator, when tPA is used alone high doses must be infused to activate the two other plasminogen’s. As much as 150 mg was tried but this caused intracranial hemorrhage so that 100 mg is now the standard. However, even at these doses tPA remains a weak plasminogen activator and was never sufficiently effective. It is also subject to hemorrhagic side effects, especially when used for ischemic stroke (this is associated with 7% intracranial hemorrhage complications).
As a result percutaneous coronary intervention (PCI) has become the treatment of choice in AMI, and procedures like thrombectomy are being increasingly employed for ischemic stroke instead of or in addition to tPA. These are time-consuming hospital procedures as well, rather than tPA. However, the only rapid reperfusion method available is fibrinolysis, but both its efficacy and safety must be improved over what it is with tPA.
Why tPA monotherapy is inadequate
tPA’s unique fibrinolytic property is its fibrin affinity a single fibrin close to a plasminogen binding site. As a result of this binding proximity, tPA’s plasminogen activating activity is promoted about 1,000-fold [2].
What can be learned from endogenous fibrinolysis? The natural design
An explanation for the disappointing adequacy of tPA therapy is revealed by the biological design responsible for fibrinolysis. In contrast to therapy, in nature there is a second plasminogen activator in blood called urokinase plasminogen activator (uPA). The native form of uPA is a proenzyme, prouPA, which is stable in plasma and has fibrin-specific fibrinolytic properties [2], though it does not bind to fibrin. In physiology, tPA initiates fibrinolysis but it is then continued and completed by uPA, first by prouPA and then by two-chain uPA (tcuPA), also called urokinase (UK).
Therefore, tPA and uPA together dissolve the fibrin clot, a mechanism that is both more effective and much safer then when tPA is used alone, since the high doses of tPA that are required when used alone are associated with hemorrhagic complications due tPA binding and disrupting hemostatic fibrin sites. These sites cannot be detected ahead of time. Therefore, bleeding complications by tPA are unpredictable. They are also unnecessary, since due to tPA’s high affinity for the fibrin in a clot, a bolus is sufficient.
Avoiding infusions essentially eliminates the bleeding risk from the lysis of hemostatic sites.
Since uPA has two active forms, prouPA and tcuPA, whereas tPA has only one, uPA is responsible for 2/3 of fibrinolysis. It activates two of the three fibrin-bound plasminogen’s that are responsible for fibrinolysis. The combination of bolus tPA followed by a prouPA infusion is also much safer. It is not only because tPA infusions are eliminated but also because significantly lower doses are required. This is because tPA and prouPA have complementary modes of action, which gives their combination a synergistic effect [3].
This natural combination was once tested in a clinical study of 101 patients with AMI who were given a 5 mg bolus of tPA followed by a 90-minute infusion of prouPA (40 mg/h) (PATENT study). Compared with the best of the tPA monotherapy studies (GUSTO), this combination regimen reduced mortality 6-fold (1% vs 6%) and almost doubled the opening of the infarct artery (82% vs 45%) [4]. These findings were consistent with the in vitro clot lysis studies showing that the combination effect to be synergistic and more effective.
Had the PATENT regimen been adopted at the time it was published, almost one million AMI deaths might have been averted in the US alone. Unfortunately, no second study with the regimen was possible since following the PATENT trial, the company developing prouPA was bought by Pharmacia which decided to discontinue its cardiovascular product line.
Conclusion
The use of tPA alone for fibrinolysis remains inadequate and is due to a misunderstanding of fibrinolysis. This started in 1987 when tPA was first given FDA approval. Its inadequacy is related to tPA’s fibrin binding site restricting it to the activation of only one of the three fibrin-bound plasminogens responsible for fibrinolysis. In addition, tPA when given alone requires administration by a very high dose of 100 mg, which risks causing hemorrhagic complications due to tPA binding and disrupting hemostatic fibrin. These form at vascular repair sites that can appear anywhere.
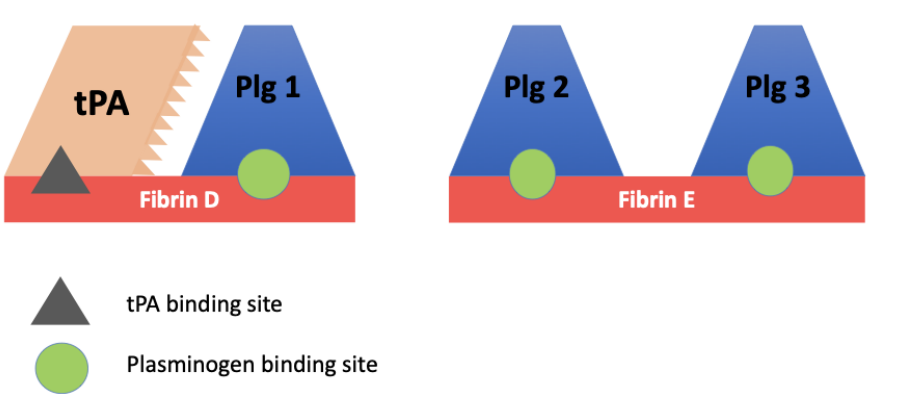
Figure 1: The plasminogen on the fibrin D-domain is activated by tPA. The two plasminogens on the E-domain are active by uPA. Plg 2 by prouPA, and Plg 3 by tcuPA (urokinase).
Instead, when the natural tPA paradigm is followed, no more than a 5 mg bolus of tPA is needed that carries little to no risk and is then is then followed by an infusion of prouPA (a proenzyme), a combination whose efficacy is promoted by synergy. Using tPA alone has been a mistake that has been hard to rereverse. Although in AMI fibrinolysis has been replaced by PCI, this method is too time- consuming to salvage function of ischemic myocardial or brain tissue in most cases. Fibrinolysis remains the simplest and fastest method to reestablish circulation and restore normal function.
References
- Brophy JM, Joseph L. Placing trials in context using Bayesian analysis. GUSTO revisited by Reverend Bayes. JAMA. 1995; 273: 871-875.
- Gurewich V, Pannell R, Louie S, et al. Effective and fibrin- specific clot lysis by a zymogen precursor of urokinase (pro- urokinase) in vitro and in two animal species. J Clin Invest. 1984; 73: 1731-1739.
- Pannell R, Black J, Gurewich V. The complementary modes of action of tissue plasminogen activator (tPA) and pro- urokinase (proUK) by which their synergistic effect in clot lysis can be explained. J Clin Invest. 1988; 81: 853-859.
- Zarich SW, Kowalchuk GJ, Weaver WD, et al. Sequential combination thrombolytic therapy for acute myocardial infarction: results of the pro-urokinase and tPA enhancement of the thrombolysis (PATENT). J Am College of Cardiology. 1995; 26: 374-379.