Vaccination against Pneumococcus and Influenza in Old Age: Evidence- Based Geriatrics
Author'(s): Jiménez-Acosta Yenesis del Carmen1, Mondragón-Cervantes Martha Ivón2, De la Cruz-Pérez Cristy Noemí2, Padilla-Sánchez Mónica Lizeth2, Franco-Navarro Alfonso2, Leal-Mora David2 and Díaz-RamosJulio Alberto1,2,3*
1Tecnologico de Monterey, Escuela de Medicina y Ciencias de la Salud, México.
2Unidad de Atención Geriátrica de Alta Especialidad, Hospital Civil Fray Antonio Alcalde, Guadalajara, Jalisco, México.
3Hospital General de Occidente, Guadalajara, Jalisco, México.
*Correspondence:
Díaz-Ramos Julio Alberto, Tecnologico de Monterey, Escuela de Medicina y Ciencias de la Salud, Avenida General Ramón Corona 2514, Nuevo México, Zapopan, Jalisco, México, Tel: (33) 3669 3000; E-mail: julio.alberto.diaz.ramos.geriatra@gmail.com.
Received: 21 August 2018; Accepted: 28 September 2018
Citation: : Jiménez-Acosta Yenesis del Carmen, Mondragón-Cervantes Martha Ivón, De la Cruz-Pérez Cristy Noemí, et al. Vaccination against Pneumococcus and Influenza in Old Age: Evidence-Based Geriatrics. Clin Immunol Res. 2018; 2(2): 1-6.
Abstract
Populations around the world are rapidly ageing. Ageing presents a diminished function of the immune system which is known as immunosenescence; therefore, the elderly develop a greater susceptibility to infections such as influenza and pneumococcal pneumonia. Vaccines schemes are one of the most cost-effective strategies because they offer a cheap alternative of preventing morbidity and mortality. Demographic aging demands the improvement in elderly care in order to prevent geriatric syndromes, which affect not only dependency but also quality of life. Negative outcomes like disability could be related to an increased mortality and a decreased likelihood of influenza and pneumococcal vaccination in older people.
The establishment of the culture of primary prevention in health directed to the population of older adults, through the strategy of vaccination in old age is one of the great challenges of geriatric medicine and public health worldwide.
The aim of this manuscript is to present a detailed description of the current scientific evidence of vaccination against pneumococcus and influenza in older adults.
Keywords
Introduction
People aged 60 and older are about 11% of the world population and it is expected to increase 22% by 2050 [1,2].
Community acquired pneumonia represents one of the most common causes of hospitalization and death in elderly. Streptococcus pneumoniae causes 400,000 hospitalizations each year, and 18,000 cases of invasive pneumococcal disease occur yearly with a case-fatality rate of 20% [3]. Diseases caused by Streptococcus pneumonia contribute considerably to morbidity and mortality worldwide [4].
On the other hand, Influenza virus is responsible for 250,000 deaths yearly and it's associated with 3-5 million cases of severe infection [5]. The risk of influenza-related death increases exponentially after the age of 65 years old, and in elderly population represents more than 90% of overall influenza related mortality annually [3- 6]. Thus seasonal influenza epidemics place a heavy socioeconomic burden on both adults and the elderly [7].
Demographic aging demands the improvement in elderly care in order to prevent geriatric syndromes, which affect not only dependency but also quality of life. Moreover adults aged 50 to 60 years with underlying diseases have a higher risk of hospitalization in the influenza season [8,9]. Thus, invasive disease is more common in patients older than 65 years and chronic conditions such as cardiovascular disease and lung disease. Pneumococcal and influenza diseases remain an important health challenge.
A simpler way to reduce both infections would be to increase vaccination among children and adults. The most important effect of group immunity with influenza vaccines was found in the routine vaccination of children in Japan between 1962 and 1994, which produced a significant decrease in cases in adults [10,11]. Vaccines are one of the most cost-effective strategies because they offer a cheap alternative of preventing potential morbidity. Aging related to the increase of infections among older people make vaccination and its research an imperative issue [4,7].
Vaccination in old age is not only an effective strategy in the prevention of infections but also in the promotion of healthy aging. The objective of this article is to present a detailed and exhaustive description of the current scientific evidence of vaccination against pneumococcus and influenza in older adults.
A non-systematic review of three databases including PubMed, the Cochrane Library and Imbiomed was conducted to identify relevant articles published between 2000 and 2018. Databases was searched for English language articles using the key words "Vaccination in old age", "vaccination scheme in adults", "immunosenence", "vaccines and geriatric syndromes", and “chronic diseases and vaccination”. Additional relevant publications were identified from article reference lists.
Vaccines in old age
Immunization strategies are changing its objectives because of the new epidemiological profile of vaccine-preventable diseases. Adult’s population is one of the most relevant new targets for vaccinations that used to be administered only to children [12]. Vaccine-preventable diseases like influenza and pneumococcal infections and their sequelae may conduce to different kinds of disability or impaired mobility in older adults, that is why vaccination is a way to prevent both the infection and functional impairment [6,7,13,14].
Thus, vaccines can preserve health and quality of life in elderly patients. Lifelong vaccination should be considered because vaccine-preventable diseases can occur at any age and can be more serious in adult and elderly patients than in children. Age based approach in vaccination strategies seems to be the best option to protect the aging population [12].
Immunosenescence
In older people many of the clinical conditions are related with immunosenescence, a phenomenon that refers to the decline of the immune system associated to aging. There is an immune phenotype related to increased mortality: inversion in CD4/CD8 ratio, low count of B cells, poor T cell proliferative response, and CMV seropositive. This is associated to an increased susceptibility to infections like influenza and pneumococcus [9]. The aging of the immune system produces a chronic pro-inflammatory state that could be more severe in women. Genetic and epigenetic factors related to immune-related genes encoding proteins that are located in the X chromosome could be involved in gender-associated response to vaccines [15].
Vaccination in the elderly based on evidence
Elderly population demonstrates less effective responses to vaccination [5]. Vaccine efficacy refers to the percent reduction in disease incidence in a vaccinated population under ideal conditions. It´s measured by hospitalization and mortality rates post-vaccination. Vaccine effectiveness refers to the ability of the vaccine to prevent disease in real worldwide population [15]. The herd immunity is the protection of a certain population against an infection due to the presence of a high percentage of immune individuals in it. Naturally, when an outbreak occurs, as in an epidemic and increase the number of immune individuals decreases the probability of contact between a susceptible and an infected, until there comes a time when the transmission of the infectious agent is blocked [16].
Center for Disease Controls (CDC) recommendations for vaccination in older adults (60 years) include the annual trivalent inactivated influenza vaccine at high dose and a booster of the pneumococcal vaccine, among other vaccines [15].
The pneumococcal vaccines recommended for 65-year-old adults and older are the 23-valent polysaccharide (PPV23) and the conjugate 13-valent (PCV13) vaccine [17]. Priming with PCV13 followed by a PPSV23 booster dose induces higher antibody levels compared with a single dose of either vaccine [11]. Table 1.
The CAPiTA study (Community-Acquired Pneumonia Immunization Trial in Adults, a Dutch clinical trial supported by the manufacturer) showed that PCV13 is efficacious in preventing two thirds of BPP (75%) and around half the NBPP (45%) cases in older adults [4]. The Spanish CAPAMIS (Community-Acquired Pneumonia, Acute Myocardial Infarction and Stroke) cohort study (funded by public authorities) confirmed that PPV23 is effective against both BPP (62%) and NBPP (48%) in adults older than 60 years [4].
There was little evidence of an impact of PPV23 on the incidence of vaccine-type invasive pneumococcal disease (VT-IPD) in those aged ≥ 65 years old. There was evidence of reasonable short-term protection to the individual thus making PPV23 vaccination is a cost effective public health intervention [18].
Influenza vaccination is the most effective method for the prevention of influenza virus infection and its complications. In a study conducted in Taiwan, influenza vaccination in older adults reduced the rate of all causes for hospitalization [19].
Vaccines and chronic non-communicable diseases
Diabetes is common in the elderly population and is considered a risk factor of pneumonia therefore these patients have a high risk of death and complications [13]. Vaccination in elderly people with diabetes reduces up to 50% the rate of hospitalizations and mortality [20].
Pneumococcal vaccination reduces the risk of death and hospital admissions in elderly patients with chronic lung disease and heart failure [21]. The protective effect of pneumococcal vaccination was additional to the protective effect of influenza vaccination. Older adults who have been recently diagnosed with cancer receive influenza immunizations at much lower rates than older adults who have not been diagnosed with cancer [22].
Likewise, disability tends to be associated with a decrease in the likelihood of vaccination. In agreement with other studies, groups of older adults with less severe diseases who are not at high risk of death are more likely to be vaccinated, while another group with more severe diseases and a high risk of mortality they do not tend to be vaccinated [23].
Patients with Chronic Cardiovascular Disease have an increased risk of complications from influenza and pneumococcal infections [8]. It is estimated that more than half of the elderly population suffers from a chronic heart condition, in these patients hospitalized for pneumonia, an increase of acute myocardial infarction has been observed. Some of the pathophysiological mechanisms of such a situation are: endothelial dysfunction, plaque instability, inflammation, sympathetic activation, volume overload and arrhythmias [24].
Vaccines and outcomes other than the reduction of infections The 80% of patients older than 65 years suffer from a chronic condition that indicates the need for the administration of influenza and pneumococcal vaccines [12]. Patients with pneumococcal vaccine have a lower risk (14% less) of cardiovascular event and 8% less of mortality; this protective role of vaccine was more prominent in the elderly and in patients with high cardiovascular risk. It seems that the pneumococcal vaccine has an important role in the balance of supply and demand of oxygen in the heart, decreasing myocardial ischemia [24].
Influenza vaccination was associated with a 44% reduction in the risk of death during influenza season [25]. Patients who received the influenza vaccine after myocardial infarction or angioplasty showed a decrease in mortality and morbidity. A study in elderly patients with heart failure (HF) showed that influenza vaccination was associated with 44% lower risk of all-cause mortality and a 22% lower risk of cardiac death [8].
Thus, vaccination is associated with a decrease in all-cause mortality and associated with cardiac causes in HF patients. As consequence, the American College of Cardiology and the American Heart Association recommend vaccination in their guidelines for the diagnosis and management of heart failure in adults [8]. Table 2.
Disability and functional impairment are confounders of the association of influenza vaccination and risk of death [25]. Influenza vaccination was associated with reduced all-cause


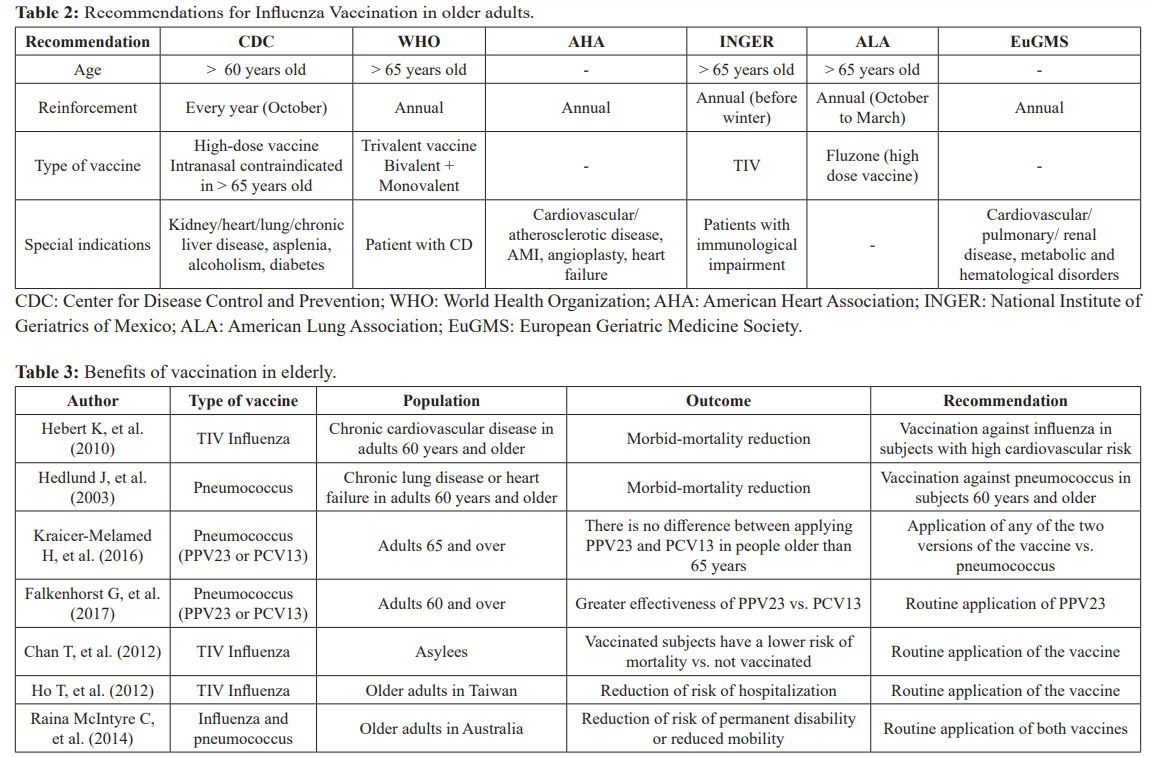
mortality in older nursing home residents with different functional status. Vaccine efficacy in reducing mortality declined with increasingly impaired functional status [26]. It was found a 61% reduction in the risk of mortality in the pre-influenza period, which indicates the presence of a healthy vaccine bias [25]. Vaccinated patients had the lowest all-cause mortality, whereas unvaccinated residents had the highest all-cause mortality [26]. Table 3.
Acceptance and rejection of vaccines in old age
Worldwide pneumococcal vaccination coverage was reported for 52.6% of adults over 60 years of age, higher in females than in males (54.8 and 50% respectively) and for influenza, older male adults presented coverage of 51.4% vs. 61.4% of women [27].
According to the literature, the decision to apply the influenza
vaccine consists of the perception of the risk of contracting the disease, understanding the severity of the consequences and the perception of preventive measures including their safety and effectiveness [28]. One study found that minorities have basic information regarding the vaccine, but no enough information about the benefits. Females report more adverse reactions and have more concerns about vaccine safety and efficacy than males [15].
The determination of vaccine eligibility in a target population is crucial for any vaccine program, and the use of electronic medical record (EMR) may significantly improve this process. However, it was seen that these templates missed some data, so the patients couldn't receive the vaccines [29].
Greater vaccination use can significantly reduce the impact of the disease in high-risk groups [7]. The financial sustainability of new vaccine introduction remains a challenge because new vaccines have to compete with other health system priorities [30]. Variants of the vaccine are manufactured directed to the older population. The differences with common vaccines are the increased amount of antigen and the intradermal route of delivery instead of intramuscular route [5]. Public health strategies must continue to improve the influenza vaccination rate among the elderly [19]. Figure 1.
Conclusion
The establishment of an effective strategy of primary prevention for the elderly population through vaccination against pneumococcus and influenza is one of the great challenges of geriatric medicine and public health policies throughout the world. We must underline the importance of monitoring vaccine schemes, since they seem to have an impact on the overall health status of the elderly. We believe that a Comprehensive Geriatric Evaluation that includes the identification of at-risk elderly people and the personal information of the vaccination schemes is an adequate tool to promote health through prevention, and to avoid the development of negative outcomes other than morbidity and mortality in the elderly.
References
- World Health Preventing Chronic Diseases: A Vital Investment. Firts edition ed. WHO, editor. Geneva: WHO press. 2005.
- Institute National Health. National Survey of Health and Nutrition. Mexico City. 2012.
- Fabel P, Horton E, Shealy K. What are the latest recommendations for pneumococcal vaccines American Academy of Physician Assistants. 2016; 29: 13-14.
- Garattini L, Padula A, Da Costa Economic Evidence of Pneumococcal Vaccination in Older Adults: Uncertain Modelling or Competitive Tendering PharmacoEconomics. 2015; 34: 221-224.
- Aspinall R, Lang Vaccine responsiveness in the elderly best practice for the clinic. Expert Review of Vaccines. 2014; 13: 885-894.
- Pop-Vicas Gravenstein S. Mini-review Iite. Gerontology.2011; 57: 397-404.
- Gasparini R,Amicizia D, Lai P, et al. Clinicalandsocioeconomic impact of seasonal and pandemic influenza in adults and the Human Vaccines & Immunotherapeutics. 2012; 8: 21-28.
- Hebert K, Marzouka G, Arcement L, et al. Prevalence of Vaccination Rates in Systolic Heart Failure A Prospective Study of 549 Patients by Age, Race, Ethnicity, and Sex in a Heart Failure Disease Management Program. Congestive Heart Failure. 2010; 16: 278-283.
- Pera A, Campos C, Lopez N, et al. Immunosenescence Implications for response to infection and vaccination in older people. Maturitas. 2015; 82: 50-55.
- Reichert TA, Sugaya N, Fedson DS et al. The Japanese experience with vaccinating schoolchildren against N Engl J Med. 2001; 344: 889-896.
- Hochman M, Cohen P. Reconsidering Guidelines on the Use of Pneumococcal Vaccines in Adults 65 Years or JAMA Internal Medicine. 2015; 175: 1895-1896.
- Bonanni P, Sacco C, Donato R, et Lifelong vaccination as a key disease-prevention strategy. Clinical Microbiology and Infection. 2014; 20: 32-36.
- Wang IK. Effectiveness of influenza vaccination in elderly diabetic patients: a retrospective cohort Vaccine. 2013; 31.
- Raina Maclntyre C, Menzies R, Kpozehouen E, et al. Equity in disease prevention Vaccines for the older adults – a national workshop, Australia 2014. Vaccine. 2016; 34: 5463-5469.
- Fink A, Klein S. Gender Impact Immune Responses to Vaccines Among the Physiology. 2015; 30: 408-416.
- Aron JL. Mathematical modeling the dynamics of infection. In Nelson KE, Williams CM, Graham Infectious Disease Epidemiology: Theory and Practice. Gaithersburg: Aspen Publishers. 2001; 149-169.
- Kraicer-Melamed H, O'Donnell S, Quach The effectiveness of pneumococcal polysaccharide vaccine 23 (PPV23) in the general population of 50 years of age and older A systematic review and meta-analysis. Vaccine. 2016; 34: 1540-1550.
- Andrews N, Waight P, George R, et Impact and effectiveness of 23-valent pneumococcal polysaccharide vaccine against invasive pneumococcal disease in the elderly in England and Wales. Vaccine. 2012; 30: 6802-6808.
- Ho T, Huang T, Huang Y, et al. The Impact of Influenza Vaccinations on the Adverse Effects and Hospitalization Rate in the Elderly: A National Based Study in an Asian Country. PLOS ONE. 2012; 7: 50337.
- Looijmans-Van den Akker I, Verheij TJ, Buskens E, et al. Clinical effectiveness of first and repeat influenza vaccination in adult and elderly diabetic Diabetes Care. 2006; 29: 1771-1776.
- Hedlund J, Christenson B, Lundbergh P, et Effects of a large- scale intervention with influenza and 23-valent pneumococcal vaccines in elderly people: a 1-year follow-up. Vaccine. 2003; 21: 3906-3911.
- Locher J, Rucks A, Spencer S, et al. Influenza Immunization in Older Adults with and without Journal of the American Geriatrics Society. 2012; 60: 2099-2103.
- Jackson LA, Nelson JC, Benson P, et Functional status is a confounder of the association of influenza vaccine and risk of all cause mortality in seniors. International Journal of Epidemiology. 2006; 35: 345-352.
- Vlachopoulos CV, Terentes-Printzios DG, Aznaouridis KA, et al. Association between pneumococcal vaccination and cardiovascular outcomes a systematic review and meta- analysis of cohort studies. European journal of preventive cardiology. 2015; 22: 1185-1199.
- Jackson Functional status is a confounder of the association of influenza vaccine and risk of all cause mortality in seniors. International Journal of Epidemiology. 2005; 35: 345-352.
- Chan T, Hung I, Luk J, et al. Functional Status of Older Nursing Home Residents Can Affect the Efficacy of Influenza The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2012; 68: 324-330.
- Gutiérrez JP, Rivera-Dommarco JASLT, Villalpando- Hernández RM. National Survey of Health and Nutrition 2012. National Results. 2a. National Institute of Public Health. 2013.
- Ward J, Raude J. Understanding influenza vaccination behaviors: a comprehensive sociocultural framework. Expert review of vaccines. 2014; 13: 17-29.
- Brownfield E, Marsden J, Iverson P, et al. Point of care experience with pneumococcal and influenza vaccine documentation among persons aged ≥65 years: High refusal rates and missing American Journal of Infection Control. 2012; 40: 672-674.
- Molina Aguilera I. Perspectives on the development and use of economic evidence for immunization decision-making in a developing country. Vaccine. 2015; 33: A6-A7.