Yes Or No for Heliosphere Airfilled Gastric Balloon
Author'(s): Falih Mohsen Algazgooz MD, Facs, Mrcs, Ali Dawood Al-Hilfi MD, Facs* and Wisam Hamza Al-Sewadi, MD, Facs, Mrcs
Basra, Sadr Teaching Hospital, Iraq.
*Correspondence:
Dr. Ali Dawood Al-Hilfi, GIT, HPB, Laparo-Endoscopic and Bariatric Surgeon, Sader Teaching Hospital, Sadr Teaching Hospital, Basra, Iraq, E-mail: alihilfi2003@yahoo.com.
Received: 01 May 2018 Accepted: 28 May 2018
Citation: Falih Mohsen Algazgooz, Ali Dawood Al-Hilfi, Wisam Hamza Al-Sewadi. Yes or No for Heliosphere Airfilled Gastric Balloon. Gastroint Hepatol Dig Dis. 2018; 1(2): 1-3.
Abstract
Objective: Obesity among the most common nutritional disorders is rising worldwide. It lead to many health problems like metabolic disorders, strock and even cancer. We share our experience by using air-filled gastric balloon (heliosphere type). Its safety, tolerability and its efficacy in weight reduction.
Methods: This study was conducted on 106 patients at one center (Al-Sadr Teaching Hospital) for the period from June 2014 to June 2015, using air-filled gastric balloon with air inflation of 600-720 ml.
The BMI of the patients was (36-58) with the prevalence of 44% male and 56% females. After consent, preballoon investigation tests, balloon was inserted with the aid of conscious sedation at the endoscopy unit. The balloon was filled with 600-720 ml of air. All patients following the procedure were given analgesia and antiemetic for five days and PPIs for six months. Diet and the importance of the exercise were part of the preballoon insertion phase and protocol. The balloon was removed after 6 months.
Results: In this study, the 106 patients with BMI (36-58) were subjected for introduction of air-filled gastric balloons over a period of six months and a follow up for them continued for up to two years.
Our patients were classified into three categories: Acceptable or good weight reduction with a mean weight reduction of 13.5 kgs, failure of weight reduction and early removal of the balloon due to unacceptable periodic pain and gastric ulcer on follow up endoscopy.
Conclusion: Despite the effective weight reduction in selected group of patients, the air filled gastric balloon is a temporary solution for obesity or as a bridge for surgery in sever morbidly obese patients. It has an unacceptable incidence of gastric ulcer.
Keywords
Introduction
Obesity is an increasing health problem worldwide. People will develop serious medical conditions, including diabetes mellitus (DM), cardiovascular diseases (CVD), stroke, liver problems, and cancer. Studies show that those potentially life threatening conditions can be improved with weight loss [1,2].
Effective weight management for individuals who are overweight is not possible, with a trail of pharmacological approaches is not achieving any significant outcomes. Bariatric surgery has provided significant weight reduction and gained popularity, but there is a price to pay, there could be complications in the procedure and its outcome, as well as associated major morbidities and even some mortality.
There is, therefore, a growing demand for the less invasive approaches such as intragastric balloon as a temporary endoscopic treatment of obesity can play an important role among the aforementioned group of obese individuals. It can also be used as a preoperative test before subjecting patients to restrictive bariatric surgery. Furthermore, the intragastric device may be applied to patients affected by severe obesity as a "bridge treatment" before they undergo major surgery in order to reduce chances of operation-related risks. Intragastric balloons have been used to induce satiety by decreasing the capacity of the gastric reservoir, thereby reducing food intake leading to weight loss in obese patients. Gastric balloons have been upgraded and improved and a number of papers on them with conflicting results have been published.[3,4,5].This paper, presents our experience of the safety, tolerance and weight reduction efficacy of the heliosphere balloon in our obese patients.
Methodology
This study was conducted on 106 patients at one center (Al-Sadr Teaching Hospital) for the period from June 2014 to June 2015), using air-filled gastric balloon with air inflation of 600-720 ml air. The BMI of the patients was (36-58) with the prevalence of 44% male and 56% females.
Exclusion criteria were as follows: Endocrinological causes of obesity, pregnancy, or planning to get pregnant, presence of gastric lesions such as active peptic ulcer disease, varices, large hiatus hernia, and previous gastric surgery, patients on anticoagulants.
Diet control of 1200 kcal and the value of regular exercise was discussed and their importance explained. Patients gave their consent, and the need for the first 3 days of adaptation was emphasized. Basic laboratory tests, that is, full blood count, biochemical profile, glycated hemoglobin, insulin level, thyroid function tests, lipid profile, electrocardiogram, . Anesthesia evaluation was done, and the procedure performed under monitored conscious sedation.
As a first step, esophagogastroduodenoscopy was performed to rule out abnormalities that would preclude balloon insertion in the patients. After the removal of the scope came the assembly of the collapsed balloon. A sheet, a collapsed balloon and the balloon filling tube were inserted into the stomach. The location of the collapsed balloon was controlled by re-inserting the scope, and under direct observation, the balloon was filled, near the antral region, with the amount of 600-720 cc of air using a 60 ml syringe.
After the balloon was filled, the scope and the syringe attached to the balloon with the filling tube were taken out. Gentle suction led to the sealing of the valve and the balloon, that is, “filling tube”. The filling tube was gently detached from the balloon and with minimum pulling pressure removed. The balloon was, therefore, left in a semi-floating condition in the stomach (Figure 1). The mean procedure time was 30 min. The patients were kept for 2 h for post procedure care and discharged home. They were allowed to start with small amounts of liquid after 6 hrs, 1.5 l in the first 24 hrs, and to start on a soft diet the 2nd day.
Antiemetic and analgesic medication (metaclopromide hydrochloride + Tramadol 50 mg twice daily) for 3 days were also given. Proton pump inhibitor (PPI) 20-40 mg once daily was to be taken for the whole period. The balloon was removed in 6 months under sedation in the endoscopy suite. The average time for the removal of the balloon was 20 min, and patients were discharged 2 hrs after the procedure, with the advice to continue the diet and exercise protocol.
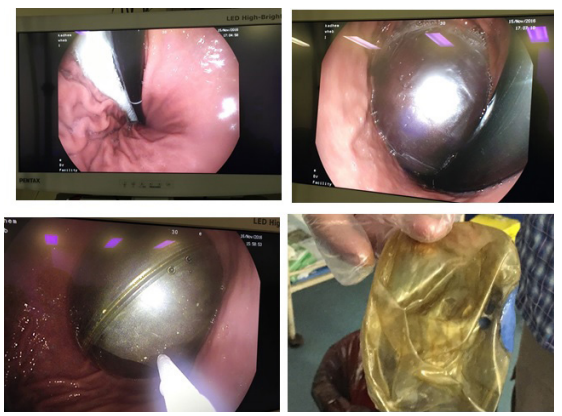
Figure 1: Steps of Balloon Application and Removal.
Results
In this study, the 106 patients with BMI (36-58) were subjected for introduction of air- filled gastric balloons over a period of six months and a follow up for them continued for up to two years.
The Exclusion criteria
- Any peptic ulcer
- Big Hiatal hernia
- Esophageal varices
- Pregnancy
- Plan for pregnancy
The study results: Mean weight reduction during 6 months of balloon application was around 13.5 kg.s.
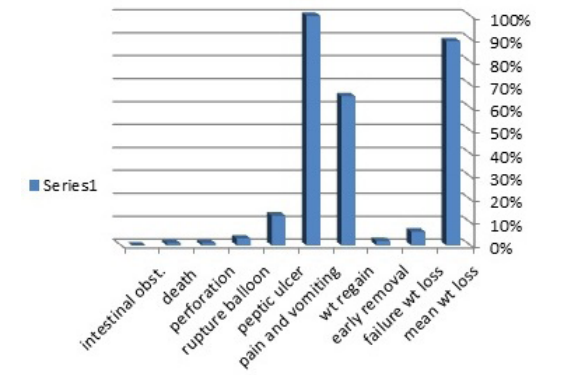
Figure 2: Outcome and Complication of Balloon Insertion.
- Failure of weight loss in 6%
- Early removal of balloon 2%
- Weight regain following removal in the period of two years follow up was 65%
- Pain and vomiting 100% especially in the first five days, which required medication
- Peptic ulcer 13% (especially gastric at upper part incisura although patients are on PPIs for three to four months of balloon application
- Ruptured balloon in 3% (diagnosed at the time of balloon extraction).
- perforation about 1%.
- death about 1%
- Intestinal obstruction 0%
Discussion
Over the years, several researchers have tried different balloon devices. One of the most recently introduced air balloon (heliosphere) is spherical in shape with a high volume capacity (600 -720 mls) and is filled with air instead of saline. Studies have shown that complication rates are very low [6-8].
The balloon itself and technique for positioning it is safe. In our study, there was one death due to perforated gastric ulcer and delayed peritonitis ended by septicemia. In addition to the unacceptable incidence of gastric ulcers especially on upper aspect of incisura that mostly occurred around four months after balloon insertion, which was diagnosed due to patient symptoms and endoscopic findings. The rate for spontaneous deflation was 3%. We found that preparation for the removal of the balloon required 2 days of intake of pure liquids with no fiber-containing nutrient.
Four to five days of analgesics and antiemetic's with regular long- term 20 mg, PPI was found to be extremely helpful for early abdominal distention, colicky pain, and vomiting.
Although PPI was extremely effective for the prevention of ulcer and balloon damage from the effect of gastric acid in other study, in our study there is unreasonable incidence of gastric ulcers (Figure 3) , while patients are on PPIs for 6 months.
Weight loss traditionally is the main objective. Weight-loss in our dedicated group of patients was impressive, with the average weight loss of 13.5 kg. However, in 2-years follow-up in this group of patients, 65% of the lost weight had been regained. Obviously, this outcome is not comparable with the results obtained in bariatric surgery, but there were noteworthy resolution of co-morbidities. The benefit of 10 kg weight loss in terms of co-morbidities (DM, HTN, and dyslipidemia) are well documented [9,10].
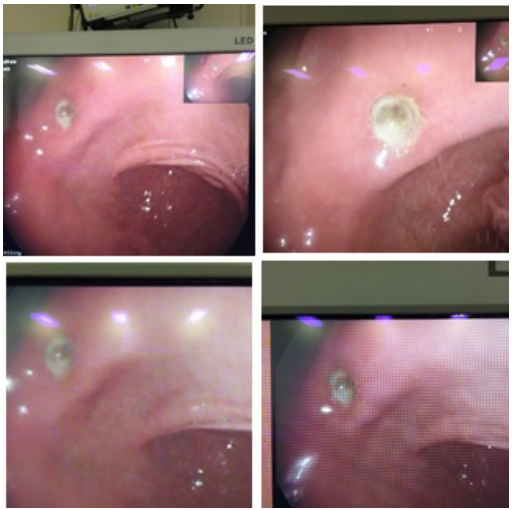
Figure 3: Oesophagogastroduodenoscopy showing gastric ulcer.
Conclusion
Despite the effective weight reduction in selected group of patients, the air filled gastric balloon is a temporary solution for obesity or as a bridge for surgery in sever morbidly obese patients. It has an unacceptable incidence of gastric ulcer.
References
- Obesity: Preventing and managing the global epidemic. Report of a WHO World Health Organ Tech Rep Ser. 2000; 894: i.
- Genco A, Cipriano M, Bacci V, et al. BioEnterics Intragastric Balloon (BIB): A short-term, double-blind, randomised, controlled, crossover study on weight reduction in morbidly obese patients. Int J Obes (Lond) 2006; 30: 129-133.
- Ponce J, Quebbemann BB, Patterson Prospective, randomized, multicenter study evaluating safety and efficacy of intragastric dual-balloon in obesity. Surg Obes Relat Dis. 2013; 9: 290-295.
- Giuricin M, Nagliati C, Palmisano S, et al. Short- and long-term efficacy of intragastric air-filled balloon (Heliosphere® BAG) among obese patients. Obes Surg. 2012; 22: 1686-1689.
- Ganesh R, Rao AD, Baladas HG, et The Bioenteric Intragastric Balloon (BIB) as a treatment for obesity: Poor results in Asian patients. Singapore Med J. 2007; 48: 227-231.
- Totté E, Hendrickx L, Pauwels M, et al. Weight reduction by means of intragastric device: Experience with the bioenterics intragastric balloon. Obes Surg. 2001; 11: 519-523.
- Roman S, Napoléon B, Mion F, et al. Intragastric balloon for “non-morbid” obesity: A retrospective evaluation of tolerance and efficacy. Obes Surg. 2004; 14: 539-544.
- Sallet JA, Marchesini JB, Paiva DS, et al. Brazilian multicenter study of the intragastric balloon. Obes Surg. 2004; 14: 991-998.
- Deitel How much weight loss is sufficient to overcome major co- morbidities? Obes Surg. 2001; 11: 659.
- Pinkney JH, Sjöström CD, Gale Should surgeons treat diabetes in severely obese people? Lancet. 2001; 357: 1357-1359.